Abstract
Background
Rectal neuroendocrine tumor (NET) is the most common NET in Asia. The risk factors associated with rectal NETs are unclear because of the overall low incidence rate of these tumors and the associated difficulty in conducting large epidemiological studies on rare cases. The aim of this study was to exploit the benefits of big data analytics to assess the risk factors associated with rectal NET.
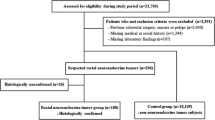
Methods
A retrospective case–control study was conducted, including 102 patients with histologically confirmed rectal NETs and 52,583 healthy controls who underwent screening colonoscopy at the Center for Health Promotion of the Samsung Medical Center in Korea between January 2002 and December 2012. Information on different risk factors was collected and logistic regression analysis applied to identify predictive factors.
Results
Four factors were significantly associated with rectal NET: higher levels of cholesterol [odds ratio (OR) = 1.007, 95 % confidence interval (CI), 1.001–1.013, p = 0.016] and ferritin (OR = 1.502, 95 % CI, 1.167–1.935, p = 0.002), presence of metabolic syndrome (OR = 1.768, 95 % CI, 1.071–2.918, p = 0.026), and family history of cancer among first-degree relatives (OR = 1.664, 95 % CI, 1.019–2.718, p = 0.042).
Conclusion
The findings of our study demonstrate the benefits of using big data analytics for research and clinical risk factor studies. Specifically, in this study, this analytical method was applied to identify higher levels of serum cholesterol and ferritin, metabolic syndrome, and family history of cancer as factors that may explain the increasing incidence and prevalence of rectal NET.
Similar content being viewed by others
References
Kulke MH, Mayer RJ. Carcinoid tumors. N Engl J Med. 1999;340:858–68.
Karzinoide SO. Tumoren des Dunndarms. Frankf Z Pathol. 1907;1:426–32.
Jernman J, Valimaki MJ, Louhimo J, Haglund C, Arola J. The novel WHO 2010 classification for gastrointestinal neuroendocrine tumours correlates well with the metastatic potential of rectal neuroendocrine tumours. Neuroendocrinology. 2012;95:317–24.
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. Geneva: World Health Organization, 2010.
Godwin JD. 2nd. Carcinoid tumors. An analysis of 2,837 cases. Cancer. 1975;36:560–9.
Naunheim KS, Zeitels J, Kaplan EL, et al. Rectal carcinoid tumors—treatment and prognosis. Surgery. 1983;94:670–6.
Scherubl H. Rectal carcinoids are on the rise: early detection by screening endoscopy. Endoscopy. 2009;41:162–5.
Modlin IM, Oberg K, Chung DC, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008;9:61–72.
Cho MY, Kim JM, Sohn JH, et al. Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000–2009: multicenter study. Cancer Res Treat. 2012;44:157–65.
Ito T, Sasano H, Tanaka M, et al. Epidemiological study of gastroenteropancreatic neuroendocrine tumors in Japan. J Gastroenterol. 2010;45:234–43.
Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113:2655–64.
Konishi T, Watanabe T, Muto T, Kotake K, Nagawa H. Site distribution of gastrointestinal carcinoids differs between races. Gut. 2006;55:1051–2.
Mandair D, Caplin ME. Colonic and rectal NET’s. Best Pract Res Clin Gastroenterol. 2012;26:775–89.
Fan J, Han F, Liu H. Challenges of big data analysis. Natl Sci Rev. 2014;1:293–314.
Chen CC, Neugut AI, Rotterdam H. Risk factors for adenocarcinomas and malignant carcinoids of the small intestine: preliminary findings. Cancer Epidemiol Biomarkers Prev. 1994;3:205–7.
Chow WH, Linet MS, McLaughlin JK, Hsing AW, Chien HT, Blot WJ. Risk factors for small intestine cancer. Cancer Causes Control. 1993;4:163–9.
Cross AJ, Leitzmann MF, Subar AF, Thompson FE, Hollenbeck AR, Schatzkin A. A prospective study of meat and fat intake in relation to small intestinal cancer. Cancer Res. 2008;68:9274–9.
Feldman JM, Plonk JW, Bivens CH, Lebovitz HE. Glucose intolerance in the carcinoid syndrome. Diabetes. 1975;24:664–71.
Hassan MM, Phan A, Li D, Dagohoy CG, Leary C, Yao JC. Risk factors associated with neuroendocrine tumors: a U.S.-based case-control study. Int J Cancer. 2008;123:867–73.
Hassan MM, Phan A, Li D, Dagohoy CG, Leary C, Yao JC. Family history of cancer and associated risk of developing neuroendocrine tumors: a case-control study. Cancer Epidemiol Biomarkers Prev. 2008;17:959–65.
Kaerlev L, Teglbjaerg PS, Sabroe S, et al. The importance of smoking and medical history for development of small bowel carcinoid tumor: a European population-based case-control study. Cancer Causes Control. 2002;13:27–34.
Mayoral W, Salcedo J, Al-Kawas F. Ampullary carcinoid tumor presenting as acute pancreatitis in a patient with von Recklinghausen’s disease: case report and review of the literature. Endoscopy. 2003;35:854–7.
Halfdanarson TR, Bamlet WR, McWilliams RR, et al. Risk factors for pancreatic neuroendocrine tumors: a clinic-based case-control study. Pancreas. 2014;43:1219–22.
Hiripi E, Bermejo JL, Sundquist J, Hemminki K. Familial gastrointestinal carcinoid tumours and associated cancers. Ann Oncol. 2009;20:950–4.
Konishi T, Watanabe T, Kishimoto J, Kotake K, Muto T, Nagawa H. Prognosis and risk factors of metastasis in colorectal carcinoids: results of a nationwide registry over 15 years. Gut. 2007;56:863–8.
Jung YS, Yun KE, Chang Y, et al. Risk factors associated with rectal neuroendocrine tumors: a cross-sectional study. Cancer Epidemiol Biomarkers Prev. 2014;23:1406–13.
Giovannucci E, Goldin B. The role of fat, fatty acids, and total energy intake in the etiology of human colon cancer. Am J Clin Nutr. 1997;66:1564s–71s.
Esposito K, Chiodini P, Capuano A, et al. Colorectal cancer association with metabolic syndrome and its components: a systematic review with meta-analysis. Endocrine. 2013;44:634–47.
Giovannucci E. Metabolic syndrome, hyperinsulinemia, and colon cancer: a review. Am J Clin Nutr. 2007;86:s836–42.
Kesse E, Clavel-Chapelon F, Boutron-Ruault MC. Dietary patterns and risk of colorectal tumors: a cohort of French women of the National Education System (E3 N). Am J Epidemiol. 2006;164:1085–93.
Norat T, Bingham S, Ferrari P, et al. Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst. 2005;97:906–16.
Slattery ML, Boucher KM, Caan BJ, Potter JD, Ma KN. Eating patterns and risk of colon cancer. Am J Epidemiol. 1998;148:4–16.
Norat T, Lukanova A, Ferrari P, Riboli E. Meat consumption and colorectal cancer risk: dose-response meta-analysis of epidemiological studies. Int J Cancer. 2002;98:241–56.
Wells AM, Haub MD, Fluckey J, Williams DK, Chernoff R, Campbell WW. Comparisons of vegetarian and beef-containing diets on hematological indexes and iron stores during a period of resistive training in older men. J Am Diet Assoc. 2003;103:594–601.
Ferrannini E. Insulin resistance, iron, and the liver. Lancet. 2000;355:2181–2.
Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB. Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. JAMA. 2004;291:711–7.
Piperno A, Trombini P, Gelosa M, et al. Increased serum ferritin is common in men with essential hypertension. J Hypertens. 2002;20:1513–8.
Halle M, Konig D, Berg A, Keul J, Baumstark MW. Relationship of serum ferritin concentrations with metabolic cardiovascular risk factors in men without evidence for coronary artery disease. Atherosclerosis. 1997;128:235–40.
Gillum RF. Association of serum ferritin and indices of body fat distribution and obesity in Mexican American men—the Third National Health and Nutrition Examination Survey. Int J Obes Relat Metab Disord. 2001;25:639–45.
Mateo-Gallego R, Calmarza P, Jarauta E, Burillo E, Cenarro A, Civeira F. Serum ferritin is a major determinant of lipid phenotype in familial combined hyperlipidemia and familial hypertriglyceridemia. Metabolism. 2010;59:154–8.
Kim CH, Kim HK, Bae SJ, Park JY, Lee KU. Association of elevated serum ferritin concentration with insulin resistance and impaired glucose metabolism in Korean men and women. Metabolism. 2011;60:414–20.
Simcox JA, McClain DA. Iron and diabetes risk. Cell Metab. 2013;17:329–41.
Bartsch H, Nair J. Chronic inflammation and oxidative stress in the genesis and perpetuation of cancer: role of lipid peroxidation, DNA damage, and repair. Langenbecks Arch Surg. 2006;391:499–510.
Berkovic MC, Jokic M, Marout J, Radosevic S, Zjacic-Rotkvic V, Kapitanovic S. IL-2 -330 T/G SNP and serum values—potential new tumor markers in neuroendocrine tumors of the gastrointestinal tract and pancreas (GEP-NETs). J Mol Med (Berl). 2010;88:423–9.
Garrelds IM, van Meeteren ME, Meijssen MA, Zijlstra FJ. Interleukin-2-deficient mice: effect on cytokines and inflammatory cells in chronic colonic disease. Dig Dis Sci. 2002;47:503–10.
Yao JC, Hoff PM, Hoff AO, eds. Neuroendocrine tumors. New York: Humana, 2011.
Debelenko LV, Zhuang Z, Emmert-Buck MR, et al. Allelic deletions on chromosome 11q13 in multiple endocrine neoplasia type 1-associated and sporadic gastrinomas and pancreatic endocrine tumors. Cancer Res. 1997;57:2238–43.
Hammel PR, Vilgrain V, Terris B, et al. Pancreatic involvement in von Hippel–Lindau disease. The Groupe Francophone d’Etude de la Maladie de von Hippel-Lindau. Gastroenterology. 2000;119:1087–95.
Lubensky IA, Pack S, Ault D, et al. Multiple neuroendocrine tumors of the pancreas in von Hippel–Lindau disease patients: histopathological and molecular genetic analysis. Am J Pathol. 1998;153:223–31.
Cappelli C, Agosti B, Braga M, et al. Von Recklinghausen’s neurofibromatosis associated with duodenal somatostatinoma. A case report and review of the literature. Minerva Endocrinol. 2004;29:19–24.
Yao JC. Neuroendocrine tumors. Molecular targeted therapy for carcinoid and islet-cell carcinoma. Best Pract Res Clin Endocrinol Metab. 2007;21:163–72.
Verhoef S, van Diemen-Steenvoorde R, Akkersdijk WL, et al. Malignant pancreatic tumour within the spectrum of tuberous sclerosis complex in childhood. Eur J Pediatr. 1999;158:284–7.
Eledrisi MS, Stuart CA, Alshanti M. Insulinoma in a patient with tuberous sclerosis: is there an association? Endocr Pract. 2002;8:109–12.
Katdare MV, Fichera A, Heimann TM. Familial rectal carcinoid: report of two first-degree relatives with rectal carcinoid and review of the literature. Tech Coloproctol. 2006;10:143–6.
Holland PW, Rubin DB. Causal inference in retrospective studies. Eval Rev. 1988;12:203–31.
Acknowledgments
This study was supported by Samsung Medical Center Grant [#SMO1131951].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pyo, J.H., Hong, S.N., Min, BH. et al. Evaluation of the risk factors associated with rectal neuroendocrine tumors: a big data analytic study from a health screening center. J Gastroenterol 51, 1112–1121 (2016). https://doi.org/10.1007/s00535-016-1198-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1198-9