Abstract
Purpose
One in three breast cancer survivors experiences persistent cognitive changes that can negatively impact daily functioning and quality of life. In our cancer center, the largest tertiary cancer center in Canada, patients with self-reported cancer-related cognitive dysfunction (CRCD) are offered psychoeducation intended to reduce distress about CRCD symptoms and improve everyday cognitive performance, but evidence regarding this intervention’s impact is lacking. Here, we assess whether a 1-hour (h), individual psychoeducational intervention designed to promote self-management of CRCD symptoms can improve attitudes and coping with memory-related difficulties in women with breast cancer.
Methods
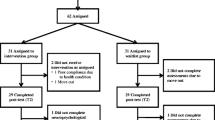
Breast cancer survivors with self-reported CRCD (N = 100) were assessed immediately before, immediately after, and 6 weeks following the intervention. Participants’ memory contentment, knowledge of CRCD, symptom distress, and self-efficacy to cope with symptoms were measured.
Results
Participants showed improvements in memory contentment immediately after the intervention (Cohen’s d effect size and 95% CI = 0.87 [0.58, 1.16]) and 6 weeks later (d = 0.77 [0.48, 1.05]). Significant improvements in secondary study outcomes, including knowledge of CRCD (d = 1.32 [1.01, 1.63]), symptom distress (d = − 0.82 [− 1.11, − 0.53]), and self-efficacy to cope with cognitive symptoms (d = 1.45 [1.14, 1.76]), were also observed.
Conclusions
A single, 1-hour psychoeducational intervention can achieve lasting and improved adjustment to memory symptoms in breast cancer survivors with self-reported CRCD. Further investigation using a randomized controlled study design is warranted. Comparisons with previously reported psychoeducational interventions for CRCD are made, and next steps for this research are discussed.
Similar content being viewed by others
References
Ahles TA, Saykin AJ, Furstenberg CT, Cole B, Mott LA, Skalla K, Whedon MB, Bivens S, Mitchell T, Greenberg ER, Silberfarb PM (2002) Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol 20(2):485–493. https://doi.org/10.1200/jco.2002.20.2.485
Bernstein LJ, Catton PA, Tannock IF (2014) Intra-individual variability in women with breast cancer. J Int Neuropsychol Soc 20(4):380–390. https://doi.org/10.1017/s1355617714000125
Jenkins V, Shilling V, Deutsch G, Bloomfield D, Morris R, Allan S, Bishop H, Hodson N, Mitra S, Sadler G, Shah E, Stein R, Whitehead S, Winstanley J (2006) A 3-year prospective study of the effects of adjuvant treatments on cognition in women with early stage breast cancer. Br J Cancer 94(6):828–834. https://doi.org/10.1038/sj.bjc.6603029
Schagen SB, van Dam FS, Muller MJ, Boogerd W, Lindeboom J, Bruning PF (1999) Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer 85(3):640–650. https://doi.org/10.1002/(SICI)1097-0142(19990201)85:3<640::AID-CNCR14>3.0.CO;2-G
Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA (2004) The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer 100(11):2292–2299. https://doi.org/10.1002/cncr.20272
Wieneke MH, Dienst ER (1995) Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psychooncology 4(1):61–66. https://doi.org/10.1002/pon.2960040108
Yao C, Rich JB, Tirona K, Bernstein LJ (2017) Intraindividual variability in reaction time before and after neoadjuvant chemotherapy in women diagnosed with breast cancer. Psychooncology 26(12):2261–2268. https://doi.org/10.1002/pon.4351
Bernstein LJ, McCreath GA, Komeylian Z, Rich JB (2017) Cognitive impairment in breast cancer survivors treated with chemotherapy depends on control group type and cognitive domains assessed: a multilevel meta-analysis. Neurosci Biobehav Rev 83:417–428. https://doi.org/10.1016/j.neubiorev.2017.10.028
Edelstein K, Bernstein LJ (2014) Cognitive dysfunction after chemotherapy for breast cancer. J Int Neuropsychol Soc 20(4):351–356. https://doi.org/10.1017/S1355617714000149
Yao C, Bernstein LJ, Rich JB (2017) Executive functioning impairment in women treated with chemotherapy for breast cancer: a systematic review. Breast Cancer Res Treat 166(1):15–28. https://doi.org/10.1007/s10549-017-4376-4
Wefel JS, Schagen SB (2012) Chemotherapy-related cognitive dysfunction. Curr Neurol Neurosci Rep 12(3):267–275. https://doi.org/10.1007/s11910-012-0264-9
Janelsins MC, Heckler CE, Peppone LJ, Kamen C, Mustian KM, Mohile SG, Magnuson A, Kleckner IR, Guido JJ, Young KL, Conlin AK, Weiselberg LR, Mitchell JW, Ambrosone CA, Ahles TA, Morrow GR (2017) Cognitive complaints in survivors of breast cancer after chemotherapy compared with age-matched controls: an analysis from a nationwide, multicenter, prospective longitudinal study. J Clin Oncol 35(5):506–514. https://doi.org/10.1200/JCO.2016.68.5826
Myers JS (2012) Chemotherapy-related cognitive impairment: the breast cancer experience. Oncol Nurs Forum 39(1):E31–E40. https://doi.org/10.1188/12.ONF.E31-E40
Shilling V, Jenkins V (2007) Self-reported cognitive problems in women receiving adjuvant therapy for breast cancer. Eur J Oncol Nurs 11(1):6–15. https://doi.org/10.1016/j.ejon.2006.02.005
Von Ah D, Habermann B, Carpenter JS, Schneider BL (2013) Impact of perceived cognitive impairment in breast cancer survivors. Eur J Oncol Nurs 17(2):236–241. https://doi.org/10.1016/j.ejon.2012.06.002
Vardy JL, Bray VJ, Dhillon HM (2017) Cancer-induced cognitive impairment: practical solutions to reduce and manage the challenge. Future Oncol 13(9):767–771. https://doi.org/10.2217/fon-2017-0027
Crouch A, Von AD, Storey S (2017) Addressing cognitive impairment after breast cancer: what do women want? Clin Nurse Spec 31(2):82–88. https://doi.org/10.1097/NUR.0000000000000279
Fitch MI, Armstrong J, Tsang S (2008) Patients’ experiences with cognitive changes after chemotherapy. Can Oncol Nurs J 18(4):180–192. https://doi.org/10.5737/1181912x184180185
King S, Green HJ (2015) Psychological intervention for improving cognitive function in cancer survivors: a literature review and randomized controlled trial. Front Oncol 5:72. https://doi.org/10.3389/fonc.2015.00072
Boykoff N, Moieni M, Subramanian SK (2009) Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv 3(4):223–232. https://doi.org/10.1007/s11764-009-0098-x
Joly F, Giffard B, Rigal O, De Ruiter MB, Small BJ, Dubois M, LeFel J, Schagen SB, Ahles TA, Wefel JS, Vardy JL, Pancre V, Lange M, Castel H (2015) Impact of cancer and its treatments on cognitive function: advances in research from the Paris International Cognition and Cancer Task Force Symposium and update since 2012. J Pain Symptom Manag 50(6):830–841. https://doi.org/10.1016/j.jpainsymman.2015.06.019
Vance DE, Frank JS, Bail J, Triebel KL, Niccolai LM, Gerstenecker A, Meneses K (2017) Interventions for cognitive deficits in breast cancer survivors treated with chemotherapy. Cancer Nurs 40(1):E11–E27. https://doi.org/10.1097/NCC.0000000000000349
Kucherer S, Ferguson RJ (2017) Cognitive behavioral therapy for cancer-related cognitive dysfunction. Curr Opin Support Palliat Care 11(1):46–51. https://doi.org/10.1097/SPC.0000000000000247
Ferguson RJ, Ahles TA, Saykin AJ, McDonald BC, Furstenberg CT, Cole BF, Mott LA (2007) Cognitive-behavioral management of chemotherapy-related cognitive change. Psychooncology 16(8):772–777. https://doi.org/10.1002/pon.1133
Ferguson RJ, McDonald BC, Rocque MA, Furstenberg CT, Horrigan S, Ahles TA, Saykin AJ (2012) Development of CBT for chemotherapy-related cognitive change: results of a waitlist control trial. Psychooncology 21(2):176–186. https://doi.org/10.1002/pon.1878
Ferguson RJ, Sigmon ST, Pritchard AJ, LaBrie SL, Goetze RE, Fink CM, Garrett AM (2016) A randomized trial of videoconference-delivered cognitive behavioral therapy for survivors of breast cancer with self-reported cognitive dysfunction. Cancer 122(11):1782–1791. https://doi.org/10.1002/cncr.29891
Schuurs A, Green HJ (2013) A feasibility study of group cognitive rehabilitation for cancer survivors: enhancing cognitive function and quality of life. Psychooncology 22(5):1043–1049. https://doi.org/10.1002/pon.3102
Ercoli LM, Castellon SA, Hunter AM, Kwan L, Kahn-Mills BA, Cernin PA, Leuchter AF, Ganz PA (2013) Assessment of the feasibility of a rehabilitation intervention program for breast cancer survivors with cognitive complaints. Brain Imaging Behav 7(4):543–553. https://doi.org/10.1007/s11682-013-9237-0
Ercoli LM, Petersen L, Hunter AM, Castellon SA, Kwan L, Kahn-Mills BA, Embree LM, Cernin PA, Leuchter AF, Ganz PA (2015) Cognitive rehabilitation group intervention for breast cancer survivors: results of a randomized clinical trial. Psychooncology 24(11):1360–1367. https://doi.org/10.1002/pon.3769
Troyer AK, Rich JB (2002) Psychometric properties of a new metamemory questionnaire for older adults. J Gerontol B Psychol Sci Soc Sci 57(1):P19–P27. https://doi.org/10.1093/geronb/57.1.P19
Kinsella GJ, Mullaly E, Rand E, Ong B, Burton C, Price S, Phillips M, Storey E (2009) Early intervention for mild cognitive impairment: a randomised controlled trial. J Neurol Neurosurg Psychiatry 80(7):730–736. https://doi.org/10.1136/jnnp.2008.148346
Regan B, Wells Y, Farrow M, O'Halloran P, Workman B (2017) MAXCOG-maximizing cognition: a randomized controlled trial of the efficacy of goal-oriented cognitive rehabilitation for people with mild cognitive impairment and early Alzheimer disease. American J Geriatr Psychiatry 25(3):258–269. https://doi.org/10.1016/j.jagp.2016.11.008
Troyer AK, Murphy KJ, Anderson ND, Moscovitch M, Craik FI (2008) Changing everyday memory behaviour in amnestic mild cognitive impairment: a randomised controlled trial. Neuropsychol Rehabil 18(1):65–88. https://doi.org/10.1080/09602010701409684
Lakens D (2013) Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 4:863
Rosenthal R (1991) Meta-analytic procedures for social research. https://doi.org/10.4135/9781412984997
Jacobson NS, Truax P (1991) Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 59(1):12–19. https://doi.org/10.1037/0022-006X.59.1.12
R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Illman NA, Moulin CJ, Kemp S (2015) Assessment of everyday memory functioning in temporal lobe epilepsy and healthy adults using the Multifactorial Memory Questionnaire (MMQ). Epilepsy Res 113:86–89. https://doi.org/10.1016/j.eplepsyres.2015.03.011
Donovan HS, Kwekkeboom KL, Rosenzweig MQ, Ward SE (2009) Nonspecific effects in psychoeducational intervention research. West J Nurs Res 31(8):983–998. https://doi.org/10.1177/0193945909338488
Vardy JL, Dhillon HM, Pond GR, Rourke SB, Bekele T, Renton C, Dodd A, Zhang H, Beale P, Clarke S (2015) Cognitive function in patients with colorectal cancer who do and do not receive chemotherapy: a prospective, longitudinal, controlled study. J Clin Oncol 33(34):4085–4092. https://doi.org/10.1200/JCO.2015.63.0905
Zer A, Pond GR, Razak ARA, Tirona K, Gan HK, Chen EX, O’Sullivan B, Waldron J, Goldstein DP, Weinreb I, Hope AJ, Kim JJ, Chan KKW, Chan AK, Siu LL, Bernstein LJ (2018) Association of neurocognitive deficits with radiotherapy or chemoradiotherapy for patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg 144(1):71–79. https://doi.org/10.1001/jamaoto.2017.2235
Funding
Support for this study was provided by the Princess Margaret Cancer Foundation, the Canadian Breast Cancer Foundation, the Canadian Institutes of Health Research (CIHR) disease management grant RN 142313-261573, and a CIHR Canada Graduate Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants
All procedures performed in this study were in accordance with the ethical standards of the local institutional review board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Prior to participation, all patients provided written informed consent.
Role of the funding source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Bernstein, L.J., McCreath, G.A., Nyhof-Young, J. et al. A brief psychoeducational intervention improves memory contentment in breast cancer survivors with cognitive concerns: results of a single-arm prospective study. Support Care Cancer 26, 2851–2859 (2018). https://doi.org/10.1007/s00520-018-4135-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4135-z