Abstract
Objective
Staphylococcus lugdunensis is considered to be more aggressive than other coagulase-negative staphylococci (CoNS). There are gaps in knowledge regarding the importance of isolating S. lugdunensis from different sources and in different patient subsets. Our objective was to describe the spectrum, clinical manifestations, and outcomes of infections caused by S. lugdunensis in patients with cancer.
Methods
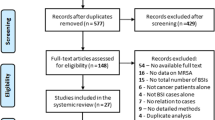
A retrospective review of all cancer patients from whom S. lugdunensis was isolated in a pure culture from clinically significant sites.
Results
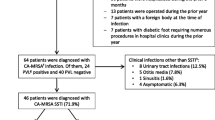
Between 2011 and 2014, 2263 CoNS were isolated, of them 45 S. lugdunensis were isolated in a pure culture and were included in this analysis. Only three patients were neutropenic. Skin and skin structure infections (SSSIs) occurred most often (36 cases) followed by five blood stream infections, one of which had destructive endocarditis and four infections at other sites. Of the 36 SSSIs, 29 were related to surgical or invasive procedures, and six of these involved an implanted medical device. All isolates were susceptible to vancomycin, 98% to levofloxacin and 89% to oxacillin. All patients responded to the therapy.
Conclusions
Cancer patients including those with neutropenia do not appear to have an increased frequency of infections caused by S. lugdunensis. SSSIs are predominant and are often associated with surgical procedures and/or implanted medical devices. Blood stream infections caused by S. lugdunensis are uncommon but may have an increased rate of serious complications such as endocarditis. Nevertheless, these organisms are generally susceptible to multiple classes of antimicrobial agents, and the overall response to therapy is high.


Similar content being viewed by others
References
Nesher L, Rolston KV (2014) The current spectrum of infection in cancer patients with chemotherapy related neutropenia. Infection 42(1):5–13
Freney J, Brun Y, Bes M, Meugnier H, Grimont F, Grimont P (1988) Staphylococcus lugdunensis sp. nov. and staphylococcus schleiferi sp. nov., two species from human clinical specimens. Int J Syst Bacteriol 38:168–172
Frank KL, Del Pozo JL, Patel R (2008) From clinical microbiology to infection pathogenesis: how daring to be different works for Staphylococcus lugdunensis. Clin Microbiol Rev 21(1):111–133
Liang M, Mansell C, Wade C, Fisher R, Devlin G (2012) Unusually virulent coagulase-negative Staphylococcus lugdunensis is frequently associated with infective endocarditis: a Waikato series of patients. N Z Med J 125(1354):51–59
Shah NB, Osmon DR, Fadel H, Patel R, Kohner PC, Steckelberg JM et al (2010) Laboratory and clinical characteristics of staphylococcus lugdunensis prosthetic joint infections. J Clin Microbiol 48(5):1600–1603
Klotchko A, Wallace MR, Licitra C, Sieger B (2011) Staphylococcus lugdunensis: an emerging pathogen. South Med J 104(7):509–514
Liesenborghs L, Peetermans M, Claes J, Veloso TR, Vandenbriele C, Criel M et al (2016) Shear-resistant binding to von willebrand factor allows staphylococcus lugdunensis to adhere to the cardiac valves and initiate endocarditis. J Infect Dis 213(7):1148–1156
Fadel HJ, Patel R, Vetter EA, Baddour LM (2011) Clinical significance of a single Staphylococcus lugdunensis-positive blood culture. J Clin Microbiol 49(4):1697–1699
German GJ, Wang B, Bernard K, Stewart N, Chan F, Pacheco AL et al (2013) Staphylococcus lugdunensis: low prevalence and clinical significance in a pediatric microbiology laboratory. Pediatr Infect Dis J 32(1):87–89
Bieber L, Kahlmeter G (2010) Staphylococcus lugdunensis in several niches of the normal skin flora. Clin Microbiol Infect 16(4):385–388
Bellamy R, Barkham T (2002) Staphylococcus lugdunensis infection sites: predominance of abscesses in the pelvic girdle region. Clin Infect Dis 35(3):E32–E34
Lina B, Vandenesch F, Reverdy ME, Greenland T, Fleurette J, Etienne J (1994) Non-puerperal breast infections due to Staphylococcus lugdunensis. Eur J Clin Microbiol Infect Dis 13(8):686–687
Hellbacher C, Törnqvist E, Söderquist B (2006) Staphylococcus lugdunensis: clinical spectrum, antibiotic susceptibility, and phenotypic and genotypic patterns of 39 isolates. Clin Microbiol Infect 12(1):43–49
Kleiner E, Monk AB, Archer GL, Forbes BA (2010) Clinical significance of staphylococcus lugdunensis isolated from routine cultures. Clin Infect Dis 51(7):801–803
Beekmann SE, Diekema DJ, Doern GV (2005) Determining the clinical significance of coagulase-negative staphylococci isolated from blood cultures. Infect Control Hosp Epidemiol 26(6):559–566
Sabe MA, Shrestha NK, Gordon S and Menon V 2014 Staphylococcus lugdunensis: a rare but destructive cause of coagulase-negative staphylococcus infective endocarditis. Eur Heart J Acute Cardiovasc Care
Streit JM, Jones RN, Sader HS, Fritsche TR (2004) Assessment of pathogen occurrences and resistance profiles among infected patients in the intensive care unit: report from the sentry antimicrobial surveillance program (north america, 2001). Int J Antimicrob Agents 24(2):111–118
Sahm DF, Deane J, Bien PA, Locke JB, Zuill DE, Shaw KJ et al (2015) Results of the surveillance of tedizolid activity and resistance program: in vitro susceptibility of gram-positive pathogens collected in 2011 and 2012 from the United States and Europe. Diagn Microbiol Infect Dis 81(2):112–118
Biedenbach DJ, Arhin FF, Moeck G, Lynch TF, Sahm DF (2015) In vitro activity of oritavancin and comparator agents against staphylococci, streptococci and enterococci from clinical infections in Europe and North America, 2011–2014. Int J Antimicrob Agents 46(6):674–681
Tan TY, Ng SY, He J (2008) Microbiological characteristics, presumptive identification, and antibiotic susceptibilities of Staphylococcus lugdunensis. J Clin Microbiol 46(7):2393–2395
Giormezis N, Kolonitsiou F, Makri A, Vogiatzi A, Christofidou M, Anastassiou ED et al (2015) Virulence factors among staphylococcus lugdunensis are associated with infection sites and clonal spread. Eur J Clin Microbiol Infect Dis 34(4):773–778
Yen TY, Sung YJ, Lin HC, Peng CT, Tien N, Hwang KP et al. 2014 Emergence of oxacillin-resistant staphylococcus lugdunensis carrying staphylococcal cassette chromosome mec type v in central taiwan. J Microbiol Immunol Infect
Liu C, Shen D, Guo J, Wang K, Wang H, Yan Z et al (2012) Clinical and microbiological characterization of staphylococcus lugdunensis isolates obtained from clinical specimens in a hospital in China. BMC Microbiol 12:168
Tseng SP, Lin YT, Tsai JC, Hung WC, Chen HJ, Chen PF et al. 2013 Genotypes and phenotypes of staphylococcus lugdunensis isolates recovered from bacteremia. J Microbiol Immunol Infect
Pereira EM, Schuenck RP, Nouér SA, Santos KR (2011) Methicillin-resistant Staphylococcus lugdunensis carrying SCCmec type V misidentified as MRSA. Braz J Infect Dis 15(3):293–295
Ebright JR, Penugonda N, Brown W (2004) Clinical experience with Staphylococcus lugdunensis bacteremia: a retrospective analysis. Diagn Microbiol Infect Dis 48(1):17–21
Sato M, Kubota N, Horiuchi A, Kasai M, Minami K, Matsui H (2016) Frequency, clinical manifestations, and outcomes of Staphylococcus lugdunensis Bacteremia in children. J Infect Chemother 22(5):298–302
Zinkernagel AS, Zinkernagel MS, Elzi MV, Genoni M, Gubler J, Zbinden R et al. Significance of Staphylococcus lugdunensis bacteremia: report of 28 cases and Infection. 2008;36(4):314–321.
Choi SH, Chung JW, Lee EJ, Kim TH, Lee MS, Kang JM et al (2010) Incidence, characteristics, and outcomes of Staphylococcus lugdunensis bacteremia. J Clin Microbiol 48(9):3346–3349
Lin JF, Cheng CW, Kuo AJ, Liu TP, Yang CC, Huang CT et al (2015) Clinical experience and microbiologic characteristics of invasive Staphylococcus lugdunensis infection in a tertiary center in northern Taiwan. J Microbiol Immunol Infect 48(4):406–412
Wu AB, Wang MC, Tseng CC, Lin WH, Teng CH, Huang AH et al (2011) Clinical and microbiological characteristics of community-acquired Staphylococcus lugdunensis infections in Southern Taiwan. J Clin Microbiol 49(8):3015–3018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported in part by the NIH/NCI under award number P30CA016672 and used the Cancer Center Support Grant resources. The authors had a full control of the data, analysis, and writing of the manuscript, and no others had any input.
Rights and permissions
About this article
Cite this article
Nesher, L., Tarrand, J., Chemaly, R.F. et al. Staphylococcus lugdunensis infections, filling in the gaps: a 3-year retrospective review from a comprehensive cancer center. Support Care Cancer 25, 1063–1069 (2017). https://doi.org/10.1007/s00520-016-3493-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3493-7