Abstract
Introduction
The role of impedance testing in selecting patients for antireflux surgery is poorly understood. The aim of this study was to compare the outcomes of patients that underwent antireflux surgery for GERD based on an abnormal pH/abnormal impedance test versus a normal pH/abnormal impedance test.
Methods
Records of patients who had an abnormal off-medication impedance test (≥ 48 total reflux events) who underwent antireflux surgery were reviewed and divided into two groups: normal [pH−] or abnormal [pH+] esophageal acid exposure (DeMeester score > 14.7). Symptom resolution was compared: scale 1 (no resolution) to 5 (complete resolution).
Results
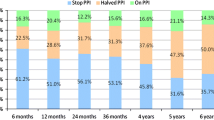
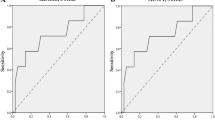
Eighty-two patients met criteria: 44 [pH+] and 38 [pH−]. There were no differences in the demographics or indications for surgery. The frequencies of heartburn and regurgitation symptoms were significantly reduced by fundoplication in both groups. Complete resolution of heartburn was more common in the [pH+] group (90%) compared to the [pH−] group (67%) [p = 0.02]. Resolution of regurgitation was similar in both groups (90% in the [pH+] group vs 79% in the [pH−] group, p = 0.20). The mean dysphagia frequency score decreased for the [pH+] group, but increased in the [pH−] group. New-onset dysphagia was more common in [pH−] patients (23%) compared to [pH+] patients (5%), (p = 0.02). Continued use of PPI medications was significantly more likely in [pH−] group (42%) compared to the [pH+] group (21%). There was no difference in surgical satisfaction rates between groups.
Discussion
Patients with abnormal impedance and increased esophageal acid exposure had significantly better symptom resolution, less dysphagia, and less frequent PPI use with antireflux surgery versus those with normal pH. These findings urge caution in the use of abnormal impedance values with normal esophageal acid exposure for the selection of patients for an antireflux operation.



Similar content being viewed by others
References
Dent J, El-Serag HB, Wallander MA et al (2005) Epidemiology of gastrooesophageal reflux disease: a systematic review. Gut 54:710–717
Kahrilas PJ, Shaheen NJ, Vaezi MF (2008) American Gastroenterological Association Institute technical review on the management of gastroesophageal reflux disease. Gastroenterology 135:1383–1413
Inadomi JM, McIntyre L, Bernard L, Fendrick AM (2003) Step-down from multiple to single-dose proton pump inhibitors (PPIs): a prospective study of patients with heartburn or acid regurgitation completely relieved with PPIs. Am J Gastroenterol 98:1940–1944
Campos GM, Peters JH, DeMeester TR, Oberg S, Crookes PF, Tan S et al (1999) Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 3:292–300
Herregods TV, Troelstra M, Weijenborg PW, Bredenoord AJ, Smout AJ (2015) Patients with refractory reflux symptoms often do not have GERD. Neurogastroenterol Motil 27(9):1267–1273
Pandolfino JE, Vela MF (2009) Esophageal reflux monitoring. Gastrointest Endosc 69:917–930
Ayazi S, Lipham JC, Portale G, Peyre CG, Streets CG, Leers JM, DeMeester SR, Banki F, Chan LS, Hagen JA, DeMeester TR (2009) Bravo catheter-free pH monitoring: normal values, concordance, optimal diagnostic thresholds, and accuracy. Clin Gastroenterol Hepatol 7(1):60–67
Agrawal A, Castell D (2008) Clinical importance of impedance measurements. J Clin Gastroenterol 42:579–583
Silny J (1991) Intraluminal multiple electric impedance procedure for measurement of gastrointestinal motility. J Gastrointest Motil 3:151–162
Tutuian R, Mainie I, Agrawal A et al (2006) Normal values for ambulatory 24-h combined impedance-pH monitoring on acid suppressive therapy. Gastroenterology 130(Suppl 2):A171
Ward MA, Dunst CM, Glasgow ME, Teitelbaum EN, Abdelmoaty WF, Reavis KM, Swanstrӧm LL, DeMeester SR (2019) Can impedance-pH testing on medications reliably identify patients with GERD as defined by pathologic esophageal acid exposure off medications? J Gastrointest Surg 23:1301–1308
Mainie I, Tutuian R, Argawal A, Adams D, Castell DO (2006) Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg Soc 95:1483–1487
Hoppo T, Sanz AF, Nason KS, Carroll TL, Rosen C, Normolle DP, Shaheen NJ, Luketich JD, Jobe AB (2012) How much pharyngeal exposure is “normal”? Normative data for laryngopharyngeal reflux events using hypopharyngeal multichannel intraluminal impedance (HMII). J Gastrointest Surg 16:16–25
Zerbib F, des Varannes S, Roman S et al (2005) Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian; French cohort of healthy subjects. Aliment Pharmacol Ther 22:1011–1021
Zentilin P, Iiritano E, Dulbecco P, Bilardi C, Savarino E, De Conca S, Parodi A, Reglioni S, Vigneri S, Savarino V (2006) Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Digest Liver Dis 38(4):226–232
Xiao YL, Lin JK, Cheung TK, Wong NY, Yang L, Hung IF, Wong BC, Chen MH (2009) Normal values of 24-hour combined esophageal multichannel intraluminal impedance and pH monitoring in the Chinese population. Digestion 79(2):109–114
Ayazi S, Lipham JC, Portale G, Peyre CG, Streets CG, Leers JM, Demeester SR, Banki F, Chan LS, Hagen JA, Demeester TR (2009) Bravo catheter-free pH monitoring: normal values, concordance, optimal diagnostic thresholds, and accuracy. Clin Gastroenerol Hepatol 7(1):60–67
Blonski W, Vela M, Castell D (2009) Comparison of reflux frequency during prolonged multichannel intraluminal impedance and pH monitoring On and Off acid suppression therapy. J Clin Gastroenterol 43(9):816–820
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Reavis is a consultant for Boston Scientific, Endogastric Solutions, and Stryker, and receives teaching or advisory honoraria from Ethicon, Mederi, Gore, and Apollo. Dr. Swanstrom is on the scientific advisory boards of Olympus, Apollo, Titan, and Boston Scientific. Dr. DeMeester is a consultant for Bard, Gore, Endogastric Solutions, C2 Therapeutics, Novadaq, Mauna Kea, and CDx Diagnostics. Dr. Dunst is a consultant for Bard Davol. These disclosures are not relevant to the current study.Authors Matt Glasgow, Naly Setthavongsack, Hannah Creasey, Dr. Davila Bradley, and Dr. Abdelmoaty have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Glasgow, M.E., Dunst, C.M., Abdelmoaty, W.F. et al. The outcome of fundoplication in patients with GERD based on abnormal impedance testing. Surg Endosc 34, 2601–2607 (2020). https://doi.org/10.1007/s00464-019-07029-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07029-w