Abstract
Background
Laparoscopic fundoplication in children under 5 kg is still debated. Our objective was to evaluate the safety and efficacy of laparoscopic fundoplication (LF) in children under 5 kg.
Methods
We reviewed the cases of 96 children treated by laparoscopic fundoplication between 2005 and 2014. Thirty-five patients had a weight of 5 kg or less at the time of LF (Low Weight Group) and 61 patients had a weight between 5.1 and 10 kg (High Weight Group). The pre-operative, peri-operative, post-operative data regarding surgery and anesthesia were compared between groups.
Results
Mean weight was 3.9 ± 0.8 kg in the LWG and 7.8 ± 1.5 kg in the HWG. Children in the LWG were more prone to pre-operative respiratory management (40% mechanical ventilation and 42.9% oxygen therapy). The operating times (82 ± 28 min for LWG and 85 ± 31 min for HWG) and respiratory parameters during the procedure (PCO2) were comparable between groups. Post-operative complications were 1 gastric perforation with peritonitis and 1 small bowel obstruction in the LWG, 2 cases of gastric perforation with peritonitis in the HWG. Mean follow-up was 67 ± 44 months. Significant recurrence of GERD requiring a redo fundoplication was noted in 3 patients in the LWG and 1 patient in the HWG.
Conclusion
Laparoscopic fundoplication is a safe procedure in infants ≤ 5 kg without increase of post-operative complications, recurrence, or mean operative time.
Similar content being viewed by others
Gastro-oesophageal reflux surgery is one of the most common surgeries performed by pediatric surgeons. According to recent guidelines, antireflux surgery may be considered in children when gastro-esophageal reflux disease (GERD) is refractory to optimal medical management [1,2,3]. Other indications are erosive esophagitis and its complications, recurrent aspiration and apnea if diagnosis of GERD has been documented, paraoesophageal hernia, and long-term thickened enteral feeding [2, 4]. Several indications for fundoplication in children with neurological impairment have also been reported. In this group of patients, LF is associated with a high recurrence rate of GERD in the long-term [5].
Laparoscopic fundoplication (LF) has replaced open fundoplication as the standard procedure for this surgery in children, because of reduced length of stay, post-operative pain, and pulmonary complications without increased long-term recurrence of GERD [1, 3, 6, 7]. Three fundoplication procedures (Nissen, Toupet, and Thal) have shown similar long-term efficacy in children and the choice of procedure mainly depends on the team [7].
There is no recommended lower age limit for performing LF. Current guidelines for GERD in older children tend to recommend non-operative management as an alternative option to surgery. However, in very small infants, GERD refractory to medical management can cause severe respiratory or cardiac complications (ALTE), or erosive oesophagitis causing reduced oral feeding and weight loss. These severe situations may influence decision toward an early surgical management of the reflux, to prevent recurrence of ALTE or protect the lower respiratory tract [8]. In addition, infants with feeding disorders due to neurologic, genetic, or metabolic conditions or prematurity may require gastrostomy tube feeding. In these small patients with hypotonia, enteral nutrition may increase the risk for aspiration pneumonia. Some teams perform prophylactic LF associated with gastrostomy tube placement in these cases. LF associated with gastrostomy tube placement increases tolerance to feeds, optimizing nutritional status [9] and may allow an earlier discharge from the hospital.
Few studies have reported data on safety of fundoplication in infants. A single-center retrospective report of open-surgery Nissen fundoplication in 102 infants under 3 months showed that the procedure was safe, with low post-operative mortality and morbidity rates and little long-term recurrence of GERD [10]. Another study focused on safety of the laparoscopic procedure in infants under 5 kg showing few complications [11]. No study has, to our knowledge, compared outcomes of early LF to LF after 5 kg.
The aim of this study was to evaluate the safety and efficacy of laparoscopic fundoplication (LF) in infants under 5 kg compared to infants weighing more than 5 kg, in terms of tolerance of the laparoscopic fundoplication, post-operative complications, and recurrence rate of GERD.
Materials and methods
Patients
We retrospectively reviewed the charts of all infants < 3 years treated by laparoscopic fundoplication according to the Nissen or Toupet technique between January 2005 and December 2014, by a single surgeon (TP) in the department of Pediatric Surgery of the University Hospital of Caen. Ninety-six infants fulfilled these criteria.
The study population was divided into two groups depending on patient’s weight at the time of the surgery: the “Low Weight group” (LWG) for patients weighing 5 kg or less, and the “High Weight Group” (HWG) between 5.1 and 10 kg. Medical records were reviewed in order to compare the peri-operative and post-operative courses between groups.
Pre-operative management and surgery
All patients were selected for surgery after evaluation by a pediatric surgeon and pediatric gastroenterologist. Diagnosis of Gastro-esophageal reflux disease was documented by one or several of the following procedures: pH monitoring, esophagogastroduodenoscopy (EGD), or upper gastrointestinal imaging (UGI). Treatments received before surgery were a combination of thickened formula, acid buffering agents, and anti-secretory agents. Indications for LF were either: GERD with severe digestive or non-digestive complications despite optimal medical treatment, or to increase tolerance to enteral feeds in patients with feeding disorders requiring a gastrostomy tube placement. Indications for gastrostomy are listed in Table 3.
Surgical technique
The initial approach was a laparoscopic fundoplication, according to the previously described Nissen or Toupet techniques. The standard procedure was a Toupet fundoplication, as this procedure is considered to cause less post-operative dysphagia. In patients requiring a gastrostomy tube placement or who already had a gastrostomy tube in place, a Nissen fundoplication was performed. All procedures were done using a 5-mm telescope (30°) and 3-mm instruments for all four ports. During the laparoscopic procedure, the objective was to maintain intra-abdominal pressure under 8 mmHg for children > 5 kg and under 6 mmHg for children ≤ 5 kg, in order to minimize cardiovascular effects.
Follow-up and post-operative management
The patients either recovered in the post-operative recovery room and were transferred to the pediatric surgery ward, or were transferred directly after the procedure to the neonatal intensive care unit (ICU) (patients ≤ 5 kg) or the pediatric ICU (> 5 kg) unit if they needed mechanical ventilation or close monitoring. Post-operative standardized care included early post-operative feeding, proton pump inhibitors for 4 days, reduced intravenous fluid administration if necessary, and peri-operative antibioprophylaxis. A post-operative UGI was performed between 3 and 4 months after the surgery.
Data analysis
Data collection
The list of patients fulfilling the inclusion criteria was retrieved from the hospital database. Data were collected retrospectively from the charts by a single investigator and included: demographic data, gestational age at birth, comorbidity, indication for surgery, treatments received before LF, pre-operative workup, type and duration of surgery, respiratory parameters during surgery, description of post-operative recovery, and immediate and long-term complications, with a study end-point at December 2017. Post-operative mortality was defined as death during the same hospitalization.
Study end-points
The primary end-point was to determine if laparoscopic fundoplication was associated with an increase of post-operative mortality and morbidity in patients ≤ 5 kg.
The secondary end-points were to determine if LF in patients ≤ 5 kg was
-
(i)
associated with an increase of post-operative respiratory events
-
(ii)
associated with an increase of short-term or long-term recurrence.
Ethical considerations
The study protocol was approved by the French Pediatric Society Ethics committee (Comité d’éthique de la recherche de la Société Française de Pediatrie). All parents were informed of the study. Written consent was not necessary for participation in this retrospective observational study, according to the French Ethical laws.
Statistical analysis
Continuous variables were described as mean ± standard deviation, or median [range] for quantitative data and values (%) for qualitative data.
Dichotomous variables were tested with the χ2 test or Fisher’s exact test when necessary. Continuous variables were tested with the t test or Mann–Whitney test.
All statistical analyses were performed using R software, 3.2.2 version (BM).
Results
Population characteristics
Mean weight at the date of LF was 3.90 kg [2.6–5.0] in the LWG, and 7.80 kg [5.2–10.0] in the HWG. The two groups were comparable regarding sex, ASA Physical Status Classification, gestational age, and comorbidities (Table 1).
Fourty-two patients had underlying conditions predisposing to more severe GERD: neurologic impairment (n = 33), repaired esophageal atresia or other congenital esophageal diseases (n = 9) with no patient in the LWG.
Pre-operative management
Clinical symptoms of GERD were similar in the two groups. Significantly more patients in the LWG required respiratory assistance (mechanical ventilation, oxygen therapy, caffeine administration) and ICU hospitalization than in the HWG (p < 0.0001, p < 0.0001, p < 0.03, and p < 0.0001, respectively) (Table 2).
Diagnostic workup before LF was the following: 9 (9.4%) patients were tested by esophageal pH monitoring, 29 (30.2%) patients underwent endoscopy with biopsies, 74 (86%) patients had a UGI, and 2 (2%) had an esophageal manometry. Pre-operative investigations by group are detailed in Table 2.
Indication for LF in the LWG was GERD associated with respiratory complications (N = 3) and/or malnutrition (N = 30) and/or ALTE [2]. Indication for LF in the HWG was chronic relapsing GERD refractory to medical treatment (30) and/or associated malnutrition (31).
Peri-operative management
In all, 64 (66.7%) Nissen procedures and 32 (33.3%) Toupet procedures were performed. Patients in the LWG were treated preferably by Nissen rather than Toupet (p = 0.003), whereas in the HWG the rates of the two procedures were comparable. No patient required a conversion to laparotomy. Eighty-six percent of patients in the LWG had a gastrostomy insertion at the same time as the LF, compared to 51% in the HWG (p < 0001) (Table 3).
Respiratory parameters and peri-operative CO2 levels were comparable between groups. Sixty-nine percent of patients in the LWG and 90% of patients in the HWG had peri-operative intra-abdominal pressure above the optimal cutoff (≤ 6 mmHg in the LWG and ≤ 8 mmHg in the HWG). However, cardiovascular function was not impeded during the procedure in these patients.
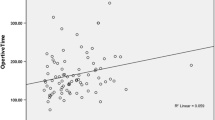
None of the patients needed an peri-operative transfusion. Mean operating time was similar between groups: 82 ± 28 min in the LWG and 85 ± 31 min in the HWG (p = 0.67) (Table 3).
Among patients in the LWG, 20 (57.1%) were extubated in the recovery room and the others were transferred to the neonatal ICU immediately after surgery. Among patients in the HWG, 53 (86.9%) were extubated in the recovery room and then transferred to the surgical ward and the others were transferred to the pediatric ICU, still intubated (p = 0.07).
Sixty-one patients (63.5%) resumed feeding at post-operative day 1. The delay before initiation of feeding was not different between groups (p = 0.76).
Morbidity and mortality (Table 4)
None of the children needed a post-operative transfusion. Seventy-one percent of patients in the LWG required to be transferred to the ICU after their surgery compared to 34% of the HWG. The proportion of patients requiring post-operative mechanical ventilation was higher in the LWG: 43 vs. 16% of the HWG (p = 0.002). In addition, significantly more patients from the LWG required post-operative oxygen therapy: 34 vs. 5% for the HWG (p < 0.001). Duration of mechanical ventilation was similar between groups: median duration 12 [2–168] in the LWG and 2 [1–32] in the HWG (p = 0.07). Post-operative parameters are summarized in Table 4.
Complications related to fundoplication and leading to a reoperation were noted in 4 patients (4.2%). In the LWG, there was one case of gastric perforation with peritonitis at post-operative day 2 (POD2) and 1 small bowel obstruction at POD72. In the HGW, there were 2 cases of gastric perforation with peritonitis that occurred at POD2 and POD4, respectively. All of these patients had been operated initially using a Nissen technique with concomitant gastrostomy tube placement. One of the patients was severely preterm, the others were born full term. All 4 patients had severe underlying conditions (malformation syndrome, neurological impairment, metabolic disease). All patients were managed successfully. None died from the complication.
None of the children died during the peri-operative period. Three patients died after discharge, within 90 days of LF. The reported cause of death was progression of the severe underlying medical condition. One patient with Zellweger syndrome died at POD39, one patient with a genetic mutation (del Q11.2) died at POD80, and one patient with Allan Hendon Duddley syndrome died at POD31. There had been no clinical recurrence of GERD after LF in these 3 patients.
Long-term outcomes
Median follow-up was 66 months. A post-operative UGI was performed in 81 patients at a median 3 months after the LF [range 1–14]. No abnormality was noted on these UGIs.
Four children had a significant recurrence of GERD requiring a redo LF procedure, 3 in the LWG (8%) and 1 in the HWG (2%) (p = 0.14, Fisher). The redo procedure was performed after a median delay of 26 months after the initial LF (8–84) (Table 5). The initial type of procedure was Nissen associated with gastrostomy tube placement in all 3 patients from the LWG and Toupet without gastrostomy in the patient from the HWG. Recurrence of GERD was suspected clinically in the 3 patients from the LWG on the basis of GERD, pulmonary infections, and vomiting for two of them. Recurrence of GERD was confirmed radiologically by UGI in all cases. One patient had evidence of herniated fundoplication (paraesophageal hernia) on the UGI. Redo procedure was performed according to the Nissen technique in all 4 cases, with hiatus hernia repair if necessary. Partial disassembly of the fundoplication was confirmed during surgery in all cases.
Among the 61 patients who had a feeding gastrostomy at the same time as the Nissen fundoplication, 11/30 (36.7%) in the LWG group and 4/31 (12.9%) in the HWG group could be weaned from enteral nutrition during follow-up and the gastrostomy was closed.
Discussion
Gastro-esophageal reflux disease (GERD) occurs frequently in the pediatric population [12]. The first line of treatment in infants is to reduce the volume of feeds and to thicken the formula. The second line of medical treatment involves H2 antihistamines or a trial of proton pump inhibitors for 4 weeks (PPI) [2]. In severe GERD resistant to medical treatment, or to increase tolerance of long-term thickened enteral feeding through a feeding tube, antireflux surgery is an established treatment option. The success of surgery is most often determined clinically by the resolution of symptoms of GERD [12].
Laparoscopic fundoplication has become a common procedure performed in children over the last 20 years, with good results reported [6, 13, 14].
For small children, in 1999, Fonkalsrud et al. reported a series of 110 children with neurological impairment who had an open antireflux surgery under 3 months of age, with a complete resolution of symptoms in 79% of the patients [10]. The benefits of LF are reduction in pulmonary complications, a hallmark of neurologically impaired patients [15]. In addition, small children are often premature with multiple respiratory, cardiac, and digestive comorbidities, that required intervention [16].
Laparoscopic procedure is debated in children under 5 kg. Recently, Papandria et al. compared the results of Nissen procedures between two groups of patients (open and laparoscopic) with a mean age of 6.4 months and a mean weight of 6.0 kg. They showed that the duration of an open Nissen procedure was significantly shorter (91 min) than a laparoscopic Nissen (173 min). In their series, only 17/39 patients (44%) were operated by laparoscopy [17]. On the contrary, our results are rather in favor of laparoscopic Nissen, with a median operating time of only 82 min in children under 5 kg (85 min in the HWG), which could be explained at least in part by the experience of the single operator who performed all the procedures. To obtain optimal operating times, the learning curve for laparoscopic surgery is estimated between 20 and 50 cases [1, 6]. Experience may also explain why there was no conversion. In the literature, Shah et al. report that laparoscopic Nissen can be safely performed in small children under 5 kg with a 6.6% conversion rate [11].
In our study, laparoscopic fundoplication was feasible and safe in the group of patients ≤ 5 kg (LWG) compared to those > 5 kg (HWG), with similar operative times and respiratory parameters during the procedure, and no need for conversion to open surgery. Although the rate of post-operative complications and reoperations was low in both groups, the immediate post-operative course was associated with a higher ICU admission rate, a higher rate of post-operative mechanical ventilation, and longer hospital stay in the LWG than in the HWG.
For pediatric anesthesiologists, the criteria to evaluate tolerance of laparoscopy are mainly CO2 monitoring [18]. In 2003, Mattioli et al. compared two groups of children (mean age 6 years) to evaluate respiratory effects of a laparoscopic Nissen. They studied CO2, O2, and non-invasive blood pressure monitoring. Laparoscopy with intra-abdominal pressure maintained lower than 10 mmHg did not interfere with gas exchanges [19]. In our series, we showed that the respiratory tolerance of LF in children under 5 kg was similar to that of patients over 5 kg, with similar peri-operative CO2 levels for both groups despite different intra-abdominal pressure levels. The laparoscopic technique in the group of patients ≤ 5 kg did not deteriorate the patients’ respiratory condition: post-operative respiratory status was unchanged from the pre-operative respiratory status. The duration of ICU stay and the duration of intubation were significantly higher in the LWG. This could be explained by the fact that some of the patients in the LWG were already dependent on mechanical ventilation and oxygen therapy in the pre-operative period. We believe care must be taken to an optimal pre-operative respiratory management in order to reduce post-operative ICU stay.
Regarding long-term outcome, we evaluated the recurrence of gastro-esophageal reflux. Rates of recurrence of GERD after laparoscopic Nissen reported in the literature are between 2.5 and 37% [11, 17, 20]. Shah et al., in a similar study, found a rate of recurrence of 3.3% and a post-operative complication rate of 4.9% [11]. Rothenberg et al. reported 1050 laparoscopic Nissen fundoplications performed in children from 5 days to 18 years (weight range 1.2–120 kg), with a 3.1% rate of reflux recurrence caused by breakdown of the fundoplication, and an peri- and post-operative complication rate of 4.8% [6].
In our study, we found a rate of recurrence of GERD requiring a redo LF of 8% in patients under 5 kg and 2% in patients over 5 kg. The recurrences occurred within 84 months of LF, and in particular during the first two years. With a follow-up of 67 ± 44 months, we believe few recurrences would have been missed in the rest of the study population.
During the post-operative course, 4 patients required surgical intervention due to perforation or small bowel obstruction. All of these patients had had a Nissen procedure with gastrostomy tube placement. Complications were noted during the first 4 post-operative days in most cases. Gastrostomy tube placement was considered to be directly responsible for the perforation in 3 out of 4 cases. In one patient, dislodgement of the gastrostomy tube was confirmed during the second surgery. The number of reinterventions was too small to be significant but these observations confirm Capito’s data that gastrostomy seems to be a risk factor for reintervention in case of fundoplication [15]. Indeed, Capito et al. reported a case of fatal peritonitis caused by the dislodgement of a gastrostomy tube [15].
According to the current ESPGHAN recommendations, an anticipated duration of enteral nutrition exceeding 4–6 weeks is an indication for gastrostomy and it can be prolonged in many cases [21]. All of the patients in our series failed medical treatment. In addition, 64% of the patients (86% in the LWG and 51% in HWG) were dependent on enteral nutrition due to their comorbidities. In all these patients, the enteral feeding was not tolerated with recurrent vomiting or pneumonias, which the team considered as a formal indication for surgery.
We recognize that associating systematically a LF to all gastrostomy tube placements in infants ≤ 5 kg is debatable. Rates of GERD after gastrostomy tube placement of up to 8.3% have been described in the literature [4, 22]. In a recent pediatric study on the complications of different gastrostomy placement techniques, between 3.7 and 6.7% of patients developed GERD requiring a Nissen fundoplication [20]. Preventing complications of GERD and a second general anesthesia are the main reasons why our center has chosen to associate systematically a LF to surgical gastrostomy placement.
Comorbidities were equal in the two groups but respiratory burden in the LWG was more important with feeding support more frequent. Some authors consider that patients with cardiac risk factors, pre-operative oxygen support or ventilator dependence, and pneumonia were all more likely to undergo fundoplication which corresponds to our cohort [23, 24].
In order to further elucidate the benefits of early antireflux surgery, a prospective study comparing surgery to medical treatment alone would be necessary. In addition to protecting the airways, antireflux surgery could be beneficial for the patient’s quality of life as described before by Brendan et al. [23]. To this purpose, our team is currently conducting a study on quality of life after Nissen LF in children.
Conclusion
Laparoscopic fundoplication is a safe procedure in infants ≤ 5 kg without increase of post-operative complications, recurrence ,or mean operating time than in the older patients. No conversion and no mortality due to the LF were noted.
References
Kane TD, Brown MF, Chen MK (2009) Position paper on laparoscopic antireflux operations in infants and children for gastroesophageal reflux disease. J Pediatr Surg 44:1034–1040
Davies I, Burman-roy S (2015) Gastro-oesophageal reflux disease in children: NICE. Br Med J 7703:1–7
Siddiqui MRS, Abdulaal Y, Nisar A, Ali H, Hasan F (2011) A meta-analysis of outcomes after open and laparoscopic Nissen’s fundoplication for gastro-oesophageal reflux disease in children. Pediatr Surg Int 27(4):359–366
Jancelewicz T, Lopez ME, Downard CD, Islam S, Baird R, Rangel SJ et al (2017) Surgical management of gastroesophageal reflux disease (GERD) in children: a systematic review. J Pediatr Surg 52(8):1228–1238
Fonkalsrud EW, Bustorff-Silva J, Perez CA, Quintero R, Martin L, Atkinson JB (1999) Antireflux surgery in children under 3 months of age. J Pediatr Surg 34(4):527–531
Rothenberg SS (2005) The first decade’s experience with laparoscopic Nissen fundoplication in infants and children. J Pediatr Surg 40:142–147
Esposito C, Montupet P, Van Der Zee D, Settimi A, Centonze A, Bax NKM (2006) Long-term outcome of laparoscopic Nissen, Toupet, and Thal antireflux procedures for neurologically normal children with gastroesophageal reflux disease. Surg Endosc 20:855–858
Monti MC, Borrelli P, Nosetti L, Taj S, Perotti M, Bonarrigo D et al (2017) Incidence of apparent life-threatening events and post-neonatal risk factors. Acta Paediatr 106(2):204–210
Barnhart DC, Hall M, Mahant S, Goldin AB, Berry JG, Faix RG et al (2013) Effectiveness of fundoplication at the time of gastrostomy in infants with neurological impairment. JAMA Pediatr 167(10):911–918
Fonkalsrud BEW, Bustorff-Silva J, Perez CA, Martin L, Atkinson JB (1999) J Pediatr Surg 34(4):527–531
Shah SR, Jegapragasan M, Fox MD, Prince JM, Segura BJ, Kane TD (2010) A review of laparoscopic Nissen fundoplication in children weighing less than 5 kg. J Pediatr Surg 45(6):1165–1168
Mauritz FA, Conchillo JM, van Heurn LWE, Siersema PD, Sloots CEJ, Houwen RHJ, van der Zee DC, van Herwaarden-Lindeboom MYA (2017) Effects and efficacy of laparoscopic fundoplication in children with GERD: a prospective, multicenter study. Surg Endosc 31(3):1101–1110
Steyaert H, Mohaidly M, Lembo MA, Carfagna L, Tursini S, Valla JS (2001) Long-term outcome of laparoscopic Nissen and Toupet fundoplication in normal and neurologically impaired children. Surg Endosc 17:543–546
Ponsky TA, Rothenberg SS (2008) Minimally invasive surgery in infants less than 5 kg: experience of 649 cases. Surg Endosc 22:2214–2219
Capito C, Leclair M, Piloquet H, Plattner V, Heloury Y, Podevin G (2008) Long-term outcome of laparoscopic Nissen-Rossetti fundoplication for neurologically impaired and normal children. Surg Endosc 22:875–880
Yoo BG, Yang HK, Lee YJ, Byun SY, Kim HY, Park JH (2014) Fundoplication in neonates and infants with primary. Pediatr Gastroenterol Hepatol Nutr 17(2):93–97
Papandria D, Goldstein SD, Salazar JH, Cox JT, Mciltrot K, Stewart FD et al (2015) A randomized trial of laparoscopic versus open Nissen fundoplication in children under two years of age. J Pediatr Surg 50(2):267–271
De Waal E, Kalkman C (2003) Haemodynamic changes during low-pressure carbon dioxide pneumoperitoneum in young children.pdf. Paediatr Anaesth 13:18–25
Mattioli G, Montobbio G, Prato AP, Repetto P, Carlini C, Gentilino V et al (2003) Anesthesiologic aspects of laparoscopic fundoplication for gastroesophageal reflux in children with chronic respiratory and gastroenterological symptoms. Surg Endosc 17:559–566
Graziano K, Teitelbaum DH, Mclean K, Hirschl RB, Coran AG, Geiger JD (2003) Recurrence after laparoscopic and open Nissen fundoplication A comparison of the mechanisms of failure. Surg Endosc 17:704–707
Wiernicka A, Matuszczyk M, Szlagatys-Sidorkiewicz A, Toporowska-Kowalska E, Popińska K, Chlebowczyk-Grzybowska U et al (2016) The protocol for a randomised-controlled trial of the evaluation of the tolerance and safety of early enteral nutrition in children after percutaneous endoscopic gastrostomy placement (protocol version 09.01.2015). BMC Pediatr 16(1):1–7
Wales PW, Diamond IR, Dutta S, Muraca S, Chait P, Connolly B et al (2017) Fundoplication and gastrostomy versus image-guided gastrojejunal tube for enteral feeding in neurologically impaired children with gastroesophageal reflux. J Pediatr Surg 37(3):407–412
Yap B, Nah SA, Chen Y, Low Y (2017) Fundoplication with gastrostomy vs gastrostomy alone: a systematic review and meta-analysis of outcomes and complications. Pediatr Surg Int 33(2):217–228
Berman L, Sharif I, Rothstein D, Hossain J, Vinocur C (2015) Concomitant fundoplication increases morbidity of gastrostomy tube placement. J Pediatr Surg 50(7):1104–1108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Claire Dupont-Lucas has received honoraria and reimbursed travel from Abbvie. Dr. Benjamin Menahem has received reimbursed travel from Sanofi Aventis. Dr. Julien Rod has received reimbursed travel from Wellspect healthcare. Drs. Thierry Petit, Philippe Ravasse, Jean-Baptiste Marret, and Camille Godet have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Marret, JB., Dupont-Lucas, C., Petit, T. et al. Safety of laparoscopic fundoplication in children under 5 kg: a comparative study. Surg Endosc 32, 4191–4199 (2018). https://doi.org/10.1007/s00464-018-6164-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6164-6