Abstract
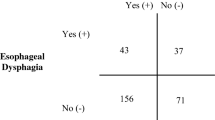
Oropharyngeal and esophageal dysphagia may occur simultaneously. However, symptoms are often evaluated separately. Few standardized, multi-texture esophageal screening protocols exist as an addition to the modified barium swallow study (MBSS). Given the gap in MBSS evaluation standards, providers may be lacking information needed to fully assess the swallowing process and create appropriate dysphagia management plans. The aim was to assess the diagnostic accuracy of a standardized esophageal screening protocol performed by an SLP compared to formal reference esophageal examinations. A cross-sectional analytic study was performed. Consecutively referred patients who underwent same-day consultation with the SLP and a gastroenterologist were included. MBSS with a standardized esophageal screen was performed. Same-day formal esophageal testing was completed and included timed barium emptying study or high-resolution manometry. Summary diagnostic accuracy measures were calculated. Seventy-three patients matched the inclusion criteria. Median age was 62.5 years (25–87), 55% were female. Sensitivity of the esophageal screen for the detection of esophageal abnormality was 83.7% (95% CI 70–91.9%); specificity was 73.7% (95% CI 55.6–85.8%). The positive likelihood ratio was 3.14 (95% CI 1.71–5.77), whereas the negative likelihood ratio was 0.22 (95% CI 0.11–0.45). Positive and negative predictive values were 82% and 76%, respectively. Use of a systematic, multi-texture esophageal screen protocol interpreted by SLPs accurately identifies multiphase dysphagia and should be considered in addition to standard MBSS testing. Inclusion of a cursory esophageal view may more adequately assess dysphagia symptoms and help to promote multidisciplinary care.


Similar content being viewed by others
References
Cangelosi MJ, Rodday AM, Saunders T, Cohen JT. Evaluation of the economic burden of diseases associated with poor nutrition status. J Parent Enteral Nutr. 2013;38(2 Suppl):35S-41S. https://doi.org/10.1177/0148607113514612.
Guyomard V, Fulcher RA, Redmayne O, Metcalf AK, Potter JF, Myint PK. Effect of dysphasia and dysphagia on inpatient mortality and hospital length of stay: a database study. J Am Geriatr Soc. 2009;57(11):2101–6. https://doi.org/10.1111/j.1532-5415.2009.02526.x.
Allen J, Greene M, Sabido I, Stretton M, Miles A. Economic costs of dysphagia among hospitalized patients. Laryngoscope. 2020;130(4):974–9.
Bonilha HS, Simpson AN, Ellis C, Mauldin P, Martin-Harris B, Simpson K. The one-year attributable cost of post-stroke dysphagia. Dysphagia. 2014;29(5):545–52. https://doi.org/10.1007/s00455-014-9543-8.
Bhattacharyya N. The prevalence of dysphagia among adults in the United States. Otolaryngol Head Neck Surg. 2014;151(5):765–9. https://doi.org/10.1177/0194599814549156.
Triadafilopoulos G, Hallstone A, Nelson-Abbott H, Bedinger K. Oropharyngeal and esophageal interrelationships in patients with nonobstructive dysphagia. Dig Dis Sci. 1992;37(4):551–7.
O’Rourke A, Morgan LB, Coss-Adame E, Morrison M, Weinberger P, Postma G. The effect of voluntary pharyngeal swallowing maneuvers on esophageal swallowing physiology. Dysphagia. 2014;29(2):262–8.
Borgstrom PS, Olsson R, Sundkvist G, Ekberg O. Pharyngeal and oesophageal function in patients with diabetes mellitus and swallowing complaints. Br J Radiol. 1988;61(729):817–21.
Farwell DG, Rees CJ, Mouadeb DA, Allen J, Chen AM, Enepekides DJ, Belafsky PC. Esophageal pathology in patients after treatment for head and neck cancer. Otolaryngol Head Neck Surg. 2010;143(3):375–8.
Huffman JA. Esophageal considerations after spinal cord injury. Perspectives on swallowing and swallowing disorders. Dysphagia. 2011;20(1):9–13.
Leopold NA, Kagel MC. Pharyngo-esophageal dysphagia in Parkinson’s disease. Dysphagia. 1997;12(1):11–8.
Montesi A, Pesaresi A, Cavalli ML, Ripa G, Candela M, Gabrielli A. Oropharyngeal and esophageal function in scleroderma. Dysphagia. 1991;6(4):219–23.
Elkberg O. To sweep or not to sweep. Dysphagia. 2019;34(1):1–1. https://doi.org/10.1007/s00455-018-09967-4.
American Speech-Language-Hearing Association: Practice portal for adult dysphagia (2017) http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589942550§ion=Assessment. Accessed 5/5/2020
Miles A, McMillan J, Ward K, Allen J. Esophageal visualization as an adjunct to the videofluoroscopic study of swallowing. Otolaryngol Head Neck Surg. 2016;152(3):488–93.
Allen JE, White C, Leonard R, Belafsky PC. Comparison of esophageal screen findings on videofluoroscopy with full esophagram results. Head Neck. 2012;34(2):264–9. https://doi.org/10.1002/hed.21727.
Watts S, Gaziano J, Jacobs J, Richter J. Improving the diagnostic capability of the modified barium swallow study through standardization of an esophageal sweep protocol. Dysphagia. 2019;34(1):34–42.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS measurement tool for swallow impairment—MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AM, International High Resolution Manometry Working Group. Chicago classification criteria of esophageal motilitydisorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl. 1):57–65.
Oliveira JM, Birgisson S, Doinoff C, Einstein D, Herts B, Davros W, Obuchowski N, Koehler RE, Richter JE, Baker ME. Timed barium swallow: a simple technique for evaluating esophageal emptying in patients with achalasia AJR. Am J Roentgenol. 1997;169(2):473–9.
Blonski W, Kumar A, Feldman J, Richter JE. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophagogastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018;113(2):196–203.
Edwards DAW. Discriminitive information in the diagnosis of dysphagia. J R Coll Phys Lond. 1975;9(3):257–63.
Roeder BE, Murry JA, Dierkhising RA. Patient localization of esophageal dysphagia. Dig Dis Sci. 2004;49(4):697–701.
Marvin S, Thibeault S. Pharyngeal versus esophageal stasis: accuracy of symptom localization. Am J Speech Lang Pathol. 2020;29(2):664–72. https://doi.org/10.1044/2019_AJSLP-19-00161.
Castell JA, Johnston BT, Colcher A, Li Q, Gideon RM, Castell DO. Manometric abnormalities of the oesophagus in patients with Parkinson’s disease. Neurogastroenterol Motil. 2001;13(4):361–4.
Mendell D, Logemann JA. A retrospective analysis of the pharyngeal swallow in patients with a clinical diagnosis of GERD compared with normal controls: a pilot study. Dysphagia. 2002;17(3):220–6.
Sivit CJ, Curtis DJ, Crain M, Cruess DF, Winters C. Pharyngeal swallow in gastroesophageal reflux disease. Dysphagia. 1988;2(3):151–5.
Lever TE, Cox KT, Holbert D, Shahrier M, Hough M, Kelley-Salamon K. The effect of an effortful swallow on the normal adult esophagus. Dysphagia. 2007;22(4):312–25.
Vanek AW, Diamant NE. Responses of the human esophagus to paired swallows. Gastroenterology. 1987;92(3):643–50.
Gullung JL, et al. Oropharyngeal and esophageal swallowing impairments: their association and the predictive value of the modified barium swallow impairment profile and combined multichannel intraluminal impedance-esophageal manometry. Ann Otology Rhinol Laryn. 2012;121(11):738–745
Jou J, Radowsky J, Gangnon R, Sadowski E, Kays S, Hind J, Gaumnitz E, Taylor AJR. Esophageal clearance patterns in normal older adults as documented with videofluoroscopic esophagram. Gastroenterol Res Pract. 2009;1:1–6.
Levine M, Rubesin S, Laufer I. Barium studies in modern radiology: do they have a role? Radiology. 2009;250(1):18–22.
Attrill S, White S, Murray J, Hammond S, Doeltgen S. Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: a systematic review. BMC Health Serv Res. 2018;18(1):594. https://doi.org/10.1186/s12913-018-3376-3.
Author information
Authors and Affiliations
Contributions
SW: study concept and design, acquisition of data, drafting of the manuscript, statistical analysis. JG: data analysis, manuscript preparation. AK: statistical analysis. JR: study concept and design, study supervision, critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watts, S., Gaziano, J., Kumar, A. et al. Diagnostic Accuracy of an Esophageal Screening Protocol Interpreted by the Speech-Language Pathologist. Dysphagia 36, 1063–1071 (2021). https://doi.org/10.1007/s00455-020-10239-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10239-3