Abstract
Pharyngeal lumen volume is prone to increase as a consequence of pharyngeal muscle atrophy in aging. Yet, the impact of this on swallowing mechanics and function is poorly understood. We examined the relationship between pharyngeal volume and pharyngeal swallowing mechanics and function in a sample of healthy community-dwelling seniors. Data were collected from 44 healthy seniors (21 male, mean age = 76.9, SD = 7.1). Each participant swallowed 9 boluses of barium (3 × 5 ml thin, 3 × 20 ml thin, 3 × 5 ml nectar). Pharyngeal shortening, pharyngeal constriction, pyriform sinus and vallecular residue were quantified from lateral view videofluorosopic swallowing studies. Pharyngeal lumen volume was captured during an oral breathing task with acoustic pharyngometry. In addition, within-participant measures of strength and anthropometrics were collected. Four linear mixed effects regression models were run to study the relationship between pharyngeal volume and pharyngeal constriction, pharyngeal shortening, pyriform sinus residue, and vallecular residue while controlling for bolus condition, age, sex, and posterior tongue strength. Increasing pharyngeal lumen volume was significantly related to worse constriction and vallecular residue. In general, larger and thicker boluses resulted in worse pharyngeal constriction and residue. Pharyngeal shortening was only significantly related to posterior tongue strength. Our work establishes the utility of acoustic pharyngometry to monitor pharyngeal lumen volume. Increasing pharyngeal lumen volume appears to impact both pharyngeal swallowing mechanics and function in a sample of healthy, functional seniors.


Similar content being viewed by others
Change history
16 September 2020
This erratum notifies the readers of the Dysphagia journal of an error in the original published version of this manuscript. In that manuscript, a previously available open source spreadsheet tool was used to calculate the position of the posterior laryngeal air column on lateral view videofluoroscopic images as a proxy for the bottom of the pharynx. We have subsequently been made aware of an error in the mathematical formula built into the spreadsheet, which resulted in a reversal of the results for the X and Y planes of measurement. This erratum provides corrections to the results and interpretations of the original manuscript.
References
Ortman JM, Velkoff VA, Hogan H: An aging nation: the older population in the United States. Current population reports, U.S. Census Bureau: 25-1140, 2014.
Robbins J. Guest editorial: the current state of clinical geriatric dysphagia research. J Rehabil Res Dev. 2002;4:vii–ix.
Chen P, Golub JS, Hapner ER, Johns MM III. Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia. 2009;1:1–6.
Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in the elderly: preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann Otol Rhinol Laryngol. 2007;11:858–65.
Bloem BR, Lagaay AM, van Beek W, Haan J, Roos RA, Wintzen AR. Prevalence of subjective dysphagia in community residents aged over 87. BMJ. 1990;6726:721–2.
Yang EJ, Kim MH, Lim J, Paik N. Oropharyngeal dysphagia in a community-based elderly cohort: The Korean longitudinal study on health and aging. J Korean Med Sci. 2013;10:1534–9.
Kikawada M, Iwamoto T, Takasaki M. Aspiration and infection in the elderly. Drugs Aging. 2005;2:115–30.
Holland G, Jayasekeran V, Pendleton N, Horan M, Jones M, Hamdy S. Prevalence and symptom profiling of oropharyngeal dysphagia in a community dwelling of an elderly population: a self-reporting questionnaire survey. Dis Esophagus. 2011;7:476–80.
Altman KW, Yu G, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010;8:784–9.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;9:1483–9.
Nagai H, Russell JA, Jackson MA, Connor NP. Effect of aging on tongue protrusion forces in rats. Dysphagia. 2008;2:116–21.
Ota F, Connor NP, Konopacki R. Alterations in contractile properties of tongue muscles in old rats. Annal Otol Rhinol Laryngol. 2005;10:799–803.
Butler SG, Stuart A, Leng X, Wilhelm E, Rees C, Williamson J, Kritchevsky SB. The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol Ser A Biol Sci Med Sci. 2011;4:452–8.
Feng X, Todd T, Lintzenich CR, Ding J, Carr JJ, Ge Y, Browne JD, Kritchevsky SB, Butler SG. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol Ser A Biol Sci Med Sci. 2013;7:853–60.
Leonard R, Kendall KA, McKenzie S. Structural displacements affecting pharyngeal constriction in nondysphagic elderly and nonelderly adults. Dysphagia. 2004;2:133–41.
Kendall KA, Leonard RJ. Pharyngeal constriction in elderly dysphagic patients compared with young and elderly nondysphagic controls. Dysphagia. 2001;4:272–8.
Aminpour S, Leonard R, Fuller SC, Belafsky PC. Pharyngeal wall differences between normal younger and older adults. ENT. 2011;4:1–4.
Molfenter SM, Amin M, Branski RC, Brumm J, Hagiwara M, Roof S, Lazarus CL. Age-related changes in pharyngeal lumen size: a retrospective MRI analysis. Dysphagia. 2015;3:321–7.
Inamoto Y, Saitoh E, Okada S, Kagaya H, Shibata S, Baba M, Onogi K, Hashimoto S, Katada K, Wattanapan P. Anatomy of the larynx and pharynx: effects of age, gender and height revealed by multidetector computed tomography. J Oral Rehabil. 2015;9:670–7.
Dejaeger E, Pelemans W, Ponette E, Joosten E. Mechanisms involved in postdeglutition retention in the elderly. Dysphagia. 1997;2:63–7.
Frederick MG, Ott DJ, Grishaw EK, Gelfand DW, Chen MYM. Functional abnormalities of the pharynx: a prospective analysis of radiographic abnormalities relative to age and symptoms. Am J Roentgenol. 1996;2:353–7.
Rofes L, Arreola V, Romea M, Palomera E, Almirall J, Cabré M, Serra-Prat M, Clavé P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil. 2010;8:851-858+e230.
Kamal I. Test-retest validity of acoustic pharyngometry measurements. Otolaryngol Head Neck Surg. 2004;2:223–8.
Brooks LJ, Byard PJ, Fouke JM, Strohl KP. Reproducibility of measurements of upper airway area by acoustic reflection. J Appl Physiol. 1989;6:2901–5.
Marshall I, Maran NJ, Martin S, Jan MA, Rimmington JE, Best JJK, Drummond GB, Douglas NJ. Acoustic reflectometry for airway measurements in man: implementation and validation. Physiol Meas. 1993;2:157–69.
Hoffstein V, Fredberg JJ. The acoustic reflection technique for non-invasive assessment of upper airway area. Eur Respir J. 1991;5:602–11.
Fredberg JJ, Wohl MEB, Glass GM, Dorkin HL. Airway area by acoustic reflections measured at the mouth. J Appl Physiol Respir Environ Exerc Physiol. 1980;5:749–58.
Bradley TD, Brown IG, Grossman RF, Zamel N, Martinez D, Phillipson EA, Hoffstein V. Pharyngeal size in snorers, nonsnorers, and patients with obstructive sleep apnea. N Engl J Med. 1986;21:1327–31.
Viviano JS. Acoustic reflection: review and clinical applications for sleep-disordered breathing. Sleep Breath. 2002;3:129–49.
D’Urzo AD, Rubinstein I, Lawson VG, Vassal KP, Rebuck AS, Slutsky AS, Hoffstein V. Comparison of glottic areas measured by acoustic reflections vs. computerized tomography. J Appl Physiol. 1988;1:367–70.
Molfenter SM. The reliability of oral and pharyngeal dimensions captured with acoustic pharyngometry. Dysphagia. 2016;4:555–9.
Nicosia MA, Hind JA, Roecker EB, Carnes M, Doyle J, Dengel GA, Robbins J. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci. 2000;11:M634–40.
Youmans SR, Youmans GL, Stierwalt JA. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;1:57–65.
Stierwalt JA, Youmans SR. Tongue measures in individuals with normal and impaired swallowing. Am J Speech Lang Pathol. 2007;2:148–56.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;12:919–24.
DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol. 1992;12:1259–61.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;3:M146–56.
Vorperian HK: VTLab Acoustic Pharyngometry (APh) Protocol: Data collection (Part I) & data analysis (Part II) 09/09, 2013.
D’Urzo AD, Lawson VG, Vassal KP, Rebuck AS, Slutsky AS, Hoffstein V. Airway area by acoustic response measurements and computerized tomography. Am Rev Respir Dis. 1987;2:392–5.
Fink TA, Ross JB. Are we testing a true thin liquid? Dysphagia. 2009;3:285–9.
Molfenter SM, Steele CM. Variation in temporal measures of swallowing: sex and volume effects. Dysphagia. 2013;2:226–33.
Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;7:671.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;2:93–8.
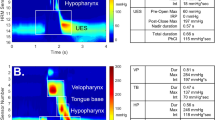
Stokely SL, Peladeau-Pigeon M, Leigh C, Molfenter SM, Steele CM. The relationship between pharyngeal constriction and post-swallow residue. Dysphagia. 2015;30:349–56.
Leonard R, Rees CJ, Belafsky P, Allen J. Fluoroscopic surrogate for pharyngeal strength: the pharyngeal constriction ratio (PCR). Dysphagia. 2011;1:13–7.
Olsson R, Castell J, Johnston B, Ekberg O, Castell DO. Combined videomanometric identification of abnormalities related to pharyngeal retention. Acad Radiol. 1997;5:349–54.
Kahrilas PJ, Logemann JA, Lin S, Ergun GA. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992;1:128–36.
Molfenter SM, Hsu CY, Lu Y, Lazarus CL. Alterations to swallowing physiology as the result of effortful swallowing in healthy seniors. Dysphagia. 2018;33:380–8.
Pearson WG Jr, Molfenter SM, Smith ZM, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013;2:167–77.
Fleiss JL. The design and analysis of clinical experiments. New York: Wiley; 1986.
Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Dysphagia. 2010;4:347–8.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;4:270–4.
Sporns PB, Muhle P, Hanning U, Suntrup-Krueger S, Schwindt W, Eversmann J, Warnecke T, Wirth R, Zimmer S, Dziewas R. Atrophy of swallowing muscles is associated with severity of dysphagia and age in patients with acute stroke. J Am Med Dir Assoc. 2017;18(7):635-e1.
Nativ-Zeltzer N, Logemann JA, Zecker SG, Kahrilas PJ. Pressure topography metrics for high-resolution pharyngeal-esophageal manofluorography-a normative study of younger and older adults. Neurogastroenterol Motil. 2016;5:721–31.
Stokely S, Molfenter SM, Leigh C, Peladeau-Pigeon M, Steele CM. The relationship between pharyngeal constriction and post-swallow residue. Abstract, Dysphagia Research Society Meeting. Dysphagia. 2014;6:737.
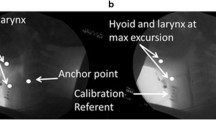
Molfenter SM, Steele CM. Use of an anatomical scalar to control for sex-based size differences in measures of hyoid excursion during swallowing. J Speech Lang Hear Res. 2014;3:768–78.
Acknowledgements
The authors would like to thank Erica Herzberg, Danielle Brates, Mehak Noorani, Emily Ottinger, Shelby Norman, Il Young Jung, Julie Bancroft, Wendy Liang, Chelsea Sandler, Marina Casale, and Katrin Gabriel for their assistance during data collection and data analysis and Chuan-Ya Hsu and Ying Lu for statistical consultation.
Funding
This study was funded by NIH National Institute on Deafness and Other Communication Disorders 1R21DC015067.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Molfenter, S.M., Lenell, C. & Lazarus, C.L. Volumetric Changes to the Pharynx in Healthy Aging: Consequence for Pharyngeal Swallow Mechanics and Function. Dysphagia 34, 129–137 (2019). https://doi.org/10.1007/s00455-018-9924-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9924-5