Abstract
Purpose
To compare the response of long-term oral contraceptive users (WomenOC; n = 8) to naturally menstruating women (WomenNM; n = 8) at rest and during exercise in temperate (TEMP; 22 °C) and hot (HEAT; 35 °C) conditions.
Methods
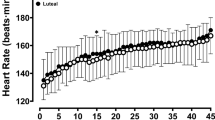
Participants performed a three-stage cycling trial in each condition at 90, 135, and 180% of lactate threshold 1 (total = 52.5 min). Heart rate (HR) and core temperature (T c) were recorded continuously, whereas blood pressure (BP), ratings of perceived exertion (RPE), blood lactate [La−], and skin blood flow (BFsk) were recorded every 7.5 min.
Results
Baseline T c was higher in WomenOC (37.5 ± 0.2, 37.6 ± 0.3 °C) than WomenNM (37.2 ± 0.2, 37.0 ± 0.4 °C) before the TEMP (p = 0.03) and HEAT (p < 0.01) trials, respectively. This difference remained for 22.5 min into both trials (p ≤ 0.05), after which time no between-group differences were found (p > 0.05). BFsk measured in WomenNM plateaued from 7.5 min in the HEAT, whereas BFsk measured in WomenOC increased for 15.0 min (p = 0.02) before plateauing. There were no between-group differences in HR, BP, or blood [La−] before or throughout either trial (p > 0.05). WomenOC had higher (p ≤ 0.04) RPE values than WomenNM in the HEAT, reporting 8 ± 1 and 6 ± 2 at the end of Stage 3, respectively.
Conclusions
WomenOC concluded both trials with a comparable T c to WomenNM, but had a prolonged BFsk response and elevated RPE in the HEAT. Changes to BFsk and RPE observed in women using OC may have implications for exercise tolerance in hot conditions.


Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- BFsk :
-
Skin blood flow
- BP:
-
Blood pressure
- C:
-
Celsius
- cm:
-
Centimeter (s)
- h:
-
Hour (s)
- HEAT:
-
Heat trial (35 °C)
- HR:
-
Heart rate
- kg:
-
Kilogram (s)
- [La−]:
-
Lactate
- L min−1 :
-
Liters per minute
- LT:
-
Lactate threshold
- min:
-
Minute (s)
- mL:
-
Milliliter (s)
- mmol/L:
-
Millimoles per liter
- OC:
-
Oral contraceptives
- RPE:
-
Ratings of perceived exertion
- rpm:
-
Revolutions per minute
- s:
-
Second (s)
- SD:
-
Standard deviation
- T c :
-
Core temperature
- TEMP:
-
Temperate trial (22 °C)
- V02 :
-
Oxygen consumption
- W:
-
Watts
- wk:
-
Week
- WomenNM:
-
Naturally menstruating women
- WomenOC:
-
Women on oral contraception
References
Baker FC, Mitchell D, Driver HS (2001) Oral contraceptives alter sleep and raise body temperature in young women Pflügers. Archiv 442:729–737
Borg G (1998) Borg’s perceived exertion and pain scales. Human kinetics, Champaign
Burrows M, Peters CE (2007) The influence of oral contraceptives on athletic performance in female athletes. Sports Med 37:557–574
Buxton C, Atkinson W (1948) Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. J Clin Endo Met 8:544–549
Charkoudian N (2003) Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. In: Mayo Clinic Proceedings, vol 5. Elsevier, pp 603–612
Charkoudian N (2010) Mechanisms and modifiers of reflex induced cutaneous vasodilation and vasoconstriction in humans. J Appl Physiol 109:1221–1228
Charkoudian N, Johnson JM (1997) Modification of active cutaneous vasodilation by oral contraceptive hormones. J Appl Physiol 83:2012–2018
Charkoudian N, Johnson JM (1999) Reflex control of cutaneous vasoconstrictor system is reset by exogenous female reproductive hormones. J Appl Physiol 87:381–385
Charkoudian N, Johnson JM (2000) Female reproductive hormones and thermoregulatory control of skin blood flow. Exerc Sport Sci Rev 28:108–112
Charkoudian N, Stachenfeld N (2016) Sex hormone effects on autonomic mechanisms of thermoregulation in humans. Auton Neurosci 196:75–80
Cheng B, Kuipers H, Snyder A, Keizer H, Jeukendrup A, Hesselink M (1992) A new approach for the determination of ventilatory and lactate thresholds. Int J Sports Med 13:518–522
Cherney DZ et al (2007) The effect of oral contraceptives on the nitric oxide system and renal function. Am J Physiol Renal Physiol 293:F1539–F1544
Cheuvront S, Kenefick R, Montain S, Sawka M (2010) Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol 109:1989–1995
Coyle EF (1999) Physiological determinants of endurance exercise performance. J Sci Med Sport 2:181–189
Crewe H, Tucker R, Noakes TD (2008) The rate of increase in rating of perceived exertion predicts the duration of exercise to fatigue at a fixed power output in different environmental conditions. Eur J Appl Physiol 103:569–577
Horvath S, Drinkwater B (1982) Thermoregulation and the menstrual cycle. Aviat Space Environ Med 53:790–794
Houghton BL, Holowatz LA, Minson CT (2005) Influence of progestin bioactivity on cutaneous vascular responses to passive heating. Med Sci Sports Exerc 37:45–51 (discussion 52)
Kamon E, Pandolf K, Cafarelli E (1974) The relationship between perceptual information and physiological responses to exercise in the heat. J Hum Ergol (Tokyo) 3:45–54
Kolka MA, Stephenson LA (1997) Effect of luteal phase elevation in core temperature on forearm blood flow during exercise. J Appl Physiol 82:1079–1083
Lee S, Williams W, Schneider S (2000) Core temperature measurement during submaximal exercise: Esophageal, rectal, and intestinal temperatures. National Aeronautics and Space Administration
Lei TH, Stannard SR, Perry BG, Schlader ZJ, Cotter JD, Mündel T (2016) Influence of menstrual phase and arid vs. humid heat stress on autonomic and behavioural thermoregulation during exercise in trained but unacclimated women. J Physiol 595:2823–2837
Martin J, Buono M (1997) Oral contraceptives elevate core temperature and heart rate duringexercise in the heat. Clin Physiol 17:401–408
Rechichi C, Dawson B, Goodman C (2009) Athletic performance and the oral contraceptive. Int J Sports Physiol Perform 4:151–162
Rogers S, Baker M (1996) Thermoregulation during exercise in women who are taking oral contraceptives. Eur J Appl Physiol Occup Physiol 75:34–38
Stachenfeld NS, Silva C, Keefe DL (2000) Estrogen modifies the temperature effects of progesterone. J Appl Physiol 88:1643–1649
Stephens DP, Bennett LAT, Aoki K, Kosiba WA, Charkoudian N, Johnson JM (2002) Sympathetic nonnoradrenergic cutaneous vasoconstriction in women is associated with reproductive hormone status. Am J Physiol Heart Circ Physiol 282:H264–H272
Stephenson L, Kolka MA (1985) Menstrual cycle phase and time of day alter reference signal controlling arm blood flow and sweating. Am J Physiol Regul Integr Comp Physiol 249:R186–R191
Sunderland C, Nevill M (2003) Effect of the menstrual cycle on performance of intermittent, high-intensity shuttle running in a hot environment. Eur J Appl Physiol 88:345–352
Tenaglia SA, McLellan TM, Klentrou PP (1999) Influence of menstrual cycle and oral contraceptives on tolerance to uncompensable heat stress. Eur J Appl Physiol Occup Physiol 80:76–83
Wendt D, van Loon L (2007) Thermoregulation during exercise in the heat: strategies for maintaining health and performance. Sports Med 37:669–682
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
This study was funded by the Queensland Academy of Sport, Centre of Excellence for Applied Sport Science Research.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Narihiko Kondo.
Rights and permissions
About this article
Cite this article
Minahan, C., Melnikoff, M., Quinn, K. et al. Response of women using oral contraception to exercise in the heat. Eur J Appl Physiol 117, 1383–1391 (2017). https://doi.org/10.1007/s00421-017-3628-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-017-3628-7