Abstract
Purpose
Pars planitis is a commonly observed type of pediatric uveitis. The aim of this study was to evaluate the implications of pars planitis–associated cystoid macular edema (CME) on visual outcome and treatment modalities.
Methods
A retrospective review of medical records in a single center with academic practice.
Results
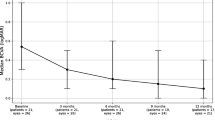
Included were 33 children (mean age 8 years, 58 eyes). Eighteen eyes developed CME (31%): in 67% of them, CME was diagnosed at presentation and in 33%, it developed at a mean of 57 months after presentation. Anterior and posterior segment complications were more prevalent in eyes with CME. Papillitis was significantly associated with the development of CME (OR 12.4, 95% CI 2.3 to 65.6, p = 0.003). Patients with CME were 1.7 times more likely to be treated with systemic therapy. By the last follow-up, 50% of patients who never developed CME were without systemic therapy compared with 13% of patients who developed CME (p = 0.034). LogMAR visual acuity improvement between presentation and month 36 was 0.41 for eyes with CME compared with 0.14 for eyes that never developed CME (p = 0.009).
Conclusion
Pars planitis–associated CME entailed higher prevalence of ocular complications, more frequent use of immunomodulatory therapy, and a lower rate of remission.


Similar content being viewed by others
Data availability
The corresponding author has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis as well as the decision to submit for publication.
References
Ozdal PC, Berker N, Tugal-Tutkun I (2015) Pars planitis: epidemiology, clinical characteristics, management and visual prognosis. J Ophthalmic Vis Res 10:469–480
Sancho L, Kramer M, Koriat A et al (2019) Complications in intermediate uveitis: prevalence, time of onset, and effects on vision in short-term and long-term follow-up. Ocul Immunol Inflamm 27:447–455
Habot-Wilner Z, Tiosano L, Sanchez JM et al (2018) Demographic and clinical features of pediatric uveitis in Israel. Ocul Immunol Inflamm 17:1–11
de Boer J, Wulffraat N, Rothova A (2003) Visual loss in uveitis of childhood. Br J Ophtalmol 87:879–884
Tugal-Tutkun I (2011) Pediatric uveitis. J Ophthalmic Vis Res 6:259–269
de Boer J, Berendschot TT, van der Does P, Rothova A (2006) Long-term follow-up of intermediate uveitis in children. Am J Ophthalmol 141:616–621
Jabs DA, Nussenblatt RB, Rosenbaum JT, Standardization of Uveitis Nomenclature (SUN) Working Group (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140:509–516
Nussenblatt RB, Palestine AG, Chan CC, Roberge F (1985) Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology 92:467–471
Sicotte NL, Voskuhl RR (2001) Onset of multiple sclerosis associated with anti-TNF therapy. Neurology. 57:1885–1888
Paroli MP, Spinucci G, Monte R et al (2011) Intermediate uveitis in a pediatric Italian population. Ocul Immunol Inflamm 19:321–326
Jain R, Ferrante P, Reddy GT, Lightman S (2005) Clinical features and visual outcome of intermediate uveitis in children. Clin Exp Ophthalmol 33:22–25
Rosenberg KD, Feuer WJ, Davis JL (2004) Ocular complications of pediatric uveitis. Ophthalmology 111:2299–2306
Khairallah M, Attia S, Zaouali S et al (2006) Pattern of childhood-onset uveitis in a referral center in Tunisia, North Africa. Ocul Immunol Inflamm 14:225–231
Ganesh SK, Bala A, Biswas J, Ahmed AS, Kempen JH (2016) Pattern of pediatric uveitis seen at a tertiary referral center from India. Ocul Immunol Inflamm 24(4):402–409
Keino H, Watanabe T, Taki W et al (2017) Clinical features of uveitis in children and adolescents at a tertiary referral centre in Tokyo. Br J Ophthalmol 101:406–410
Päivönsalo-Hietanen T, Tuominen J, Saari KM (2000) Uveitis in children: population-based study in Finland. Acta Ophthalmol Scand 78(1):84–88
Azar D, Martin F (2004) Paediatric uveitis: a Sydney clinic experience. Clin Exp Ophthalmol 32(5):468–471
Kump LI, Cervantes-Castañeda RA, Androudi SN, Foster CS (2005) Analysis of pediatric uveitis cases at a tertiary referral center. Ophthalmology 112:1287–1292
Kalinina Ayuso V, ten Cate HA, van den Does P et al (2011) Young age as a risk factor for complicated course and visual outcome in intermediate uveitis in children. Br J Ophthalmol 95:646–651
Le Scanff J, Sève P, Renoux C et al (2008) Uveitis associated with multiple sclerosis. Mult Scler 14:415–417
Smith JR, Rosenbaum JT (2004) Neurological concomitants of uveitis. Br J Ophthalmol 88:1498–1499
Zein G, Berta A, Foster CS (2004) Multiple sclerosis-associated uveitis. Ocul Immunol Inflamm 12:137–142
van Oosten B, Barkhof F, Truyen L et al (1996) Increased MRI activity and immune activation in two multiple sclerosis patients treated with the monoclonal anti-tumor necrosis factor antibody cA2. Neurology 47:1531–1534
The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group (1999) TNF neutralization in MS: results of a randomized, placebo controlled multicenter study. Neurology 53:457–465
Probert L (2015) TNF and its receptors in the CNS: the essential, the desirable and the deleterious effects. Neuroscience 302:2–22
Ding T, Ledingham J, Luqmani R et al (2010) BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies. Rheumatology 49:2217–2219
Kemanetzoglou E, Andreadou E (2017) CNS demyelination with TNF-α blockers. Curr Neurol Neurosci Rep 17:36
Author information
Authors and Affiliations
Contributions
All authors contributed by collecting information and analyzing, writing, and reviewing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This type of study does not require informed consent.
Code availability
Not relevant
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarrete, A., Koriat, A. & Amer, R. Implications of pars planitis-associated cystoid macular edema on visual outcome and management in children. Graefes Arch Clin Exp Ophthalmol 258, 1803–1811 (2020). https://doi.org/10.1007/s00417-020-04696-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04696-7