Abstract
Purpose
The purpose of this study was to evaluate the discontinuation of adalimumab (ADA) treatment in patients with juvenile idiopathic arthritis-associated uveitis (JIAU).
Methods
Patients in whom ADA treatment was initiated for JIAU were included in this retrospective analysis. Reasons for discontinuing ADA treatment in patients with primary treatment response were analysed.
Results
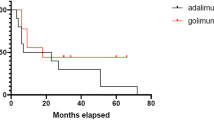
Within a group of 387 JIAU patients, 59 of 68 patients who were treated with ADA achieved a sufficient response to treatment within 6 months. Here, 39 patients (66.1 %) were still on therapy at their last follow-up visit (mean treatment duration of 38.3 months, range 12–91). In another 20 patients, ADA had been discontinued after 1 or 2 years or later, in 10 % (n = 2), 45 % (n = 9) and 45 % (n = 9) of patients, respectively (mean 30.6 months; range 10–65). Reasons for discontinuing ADA were reactivation of uveitis (n = 8, 3.93 per 100 patient-years) or arthritis (n = 4; 1.97 per 100 patient-years), or ≥2 years of complete disease inactivity (n = 3, 1.47 per 100 patient-years), adverse events (n = 4; 1.89 per 100 patient-years), or other (n = 1; 0.47 per 100 patient-years).
Conclusions
The data show a good primary response to ADA in patients with refractory JIAU. Due to the increasing rate of adalimumab failure or adverse events during long-term treatment, further treatment options may be required.


Similar content being viewed by others
References
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
BenEzra D, Cohen E, Maftzir G (2005) Uveitis in children and adolescents. Br J Ophthalmol 89:444–448. doi:10.1136/bjo.2004.050609
Carvounis PE, Herman DC, Cha S et al (2006) Incidence and outcomes of uveitis in juvenile rheumatoid arthritis, a synthesis of the literature. Graefes Arch Clin Exp Ophthalmol 244:281–290. doi:10.1007/s00417-005-0087-3
Foeldvari I, Becker I, Horneff G (2015) Uveitis events during adalimumab, etanercept, and methotrexate therapy in juvenile idiopathic arthritis: data from the Biologics in Pediatric Rheumatology Registry. Arthritis Care Res (Hoboken) 67:1529–1535. doi:10.1002/acr.22613
Heiligenhaus A, Heinz C, Edelsten C et al (2013) Review for disease of the year: epidemiology of juvenile idiopathic arthritis and its associated uveitis: the probable risk factors. Ocul Immunol Inflamm 21:180–191. doi:10.3109/09273948.2013.791701
Kotaniemi K, Kautiainen H, Karma A et al (2001) Occurrence of uveitis in recently diagnosed juvenile chronic arthritis: a prospective study. Ophthalmology 108:2071–2075
Heiligenhaus A, Niewerth M, Ganser G et al (2007) Prevalence and complications of uveitis in juvenile idiopathic arthritis in a population-based nation-wide study in Germany: suggested modification of the current screening guidelines. Rheumatology (Oxford, England) 46:1015–1019. doi:10.1093/rheumatology/kem053
Edelsten C, Lee V, Bentley CR et al (2002) An evaluation of baseline risk factors predicting severity in juvenile idiopathic arthritis associated uveitis and other chronic anterior uveitis in early childhood. Br J Ophthalmol 86:51–56
Edelsten C, Reddy MA, Stanford MR et al (2003) Visual loss associated with pediatric uveitis in english primary and referral centers. Am J Ophthalmol 135:676–680
Sijssens KM, Rothova A, Berendschot TTJM et al (2006) Ocular hypertension and secondary glaucoma in children with uveitis. Ophthalmology 113:853–859.e2. doi:10.1016/j.ophtha.2006.01.043
Thorne JE, Woreta F, Kedhar SR et al (2007) Juvenile idiopathic arthritis-associated uveitis: incidence of ocular complications and visual acuity loss. Am J Ophthalmol 143:840–846. doi:10.1016/j.ajo.2007.01.033
Gregory AC, Kempen JH, Daniel E et al (2013) Risk factors for loss of visual acuity among patients with uveitis associated with juvenile idiopathic arthritis: the Systemic Immunosuppressive Therapy for Eye Diseases Study. Ophthalmology 120:186–192. doi:10.1016/j.ophtha.2012.07.052
de Boer J, Steijaert A, van den Bor R et al (2015) Development of macular edema and impact on visual acuity in uveitis associated with juvenile idiopathic arthritis. Ocul Immunol Inflamm 23:67–73. doi:10.3109/09273948.2013.871566
Heiligenhaus A, Foeldvari I, Edelsten C et al (2012) Proposed outcome measures for prospective clinical trials in juvenile idiopathic arthritis-associated uveitis: a consensus effort from the multinational interdisciplinary working group for uveitis in childhood. Arthritis Care Res (Hoboken) 64:1365–1372. doi:10.1002/acr.21674
Bou R, Adán A, Borrás F et al (2015) Clinical management algorithm of uveitis associated with juvenile idiopathic arthritis: interdisciplinary panel consensus. Rheumatol Int 35:777–785. doi:10.1007/s00296-015-3231-3
Heiligenhaus A, Michels H, Schumacher C et al (2012) Evidence-based, interdisciplinary guidelines for anti-inflammatory treatment of uveitis associated with juvenile idiopathic arthritis. Rheumatol Int 32:1121–1133
Simonini G, Druce K, Cimaz R et al (2014) Current evidence of anti-tumor necrosis factor α treatment efficacy in childhood chronic uveitis: a systematic review and meta-analysis approach of individual drugs. Arthritis Care Res 66:1073–1084. doi:10.1002/acr.22214
Vazquez-Cobian LB, Flynn T, Lehman TJA (2006) Adalimumab therapy for childhood uveitis. J Pediatr 149:572–575. doi:10.1016/j.jpeds.2006.04.058
Biester S, Deuter C, Michels H et al (2007) Adalimumab in the therapy of uveitis in childhood. Br J Ophthalmol 91:319–324. doi:10.1136/bjo.2006.103721
Jabs DA, Nussenblatt RB, Rosenbaum JT et al (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140:509–516
Ruperto N, Ravelli A, Falcini F, Italian Pediatric Rheumatology Study Group et al (1998) Performance of the preliminary definition of improvement in juvenile chronic arthritis patients treated with methotrexate. Ann Rheum Dis 57:38–41
Foeldvari I, Nielsen S, Kümmerle-Deschner J et al (2007) Tumor necrosis factor-alpha blocker in treatment of juvenile idiopathic arthritis-associated uveitis refractory to second-line agents: results of a multinational survey. J Rheumatol 34:1146–1150
Kotaniemi K, Säilä H, Kautiainen H (2011) Long-term efficacy of adalimumab in the treatment of uveitis associated with juvenile idiopathic arthritis. Clin Ophthalmol 5:1425–1459. doi:10.2147/OPTH.S23646
Doycheva D, Zierhut M, Blumenstock G et al (2014) Immunomodulatory therapy with tumour necrosis factor α inhibitors in children with antinuclear antibody-associated chronic anterior uveitis: long-term results. Br J Ophthalmol 98:523–528. doi:10.1136/bjophthalmol-2013-303935
Tynjälä P, Kotaniemi K, Lindahl P et al (2008) Adalimumab in juvenile idiopathic arthritis-associated chronic anterior uveitis. Rheumatology (Oxford, England) 47:339–344. doi:10.1093/rheumatology/kem356
Magli A, Forte R, Navarro P et al (2013) Adalimumab for juvenile idiopathic arthritis-associated uveitis. Graefes Arch Clin Exp Ophthalmol 251:1601–1606. doi:10.1007/s00417-013-2275-x
Simonini G, Taddio A, Cattalini M et al (2011) Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of adalimumab versus infliximab. Arthritis Care Res 63:612–618. doi:10.1002/acr.20404
Zannin ME, Birolo C, Gerloni VM et al (2013) Safety and efficacy of infliximab and adalimumab for refractory uveitis in juvenile idiopathic arthritis: 1-year followup data from the Italian Registry. J Rheumatol 40:74–79. doi:10.3899/jrheum.120583
Simonini G, Taddio A, Cattalini M et al (2013) Superior efficacy of adalimumab in treating childhood refractory chronic uveitis when used as first biologic modifier drug: adalimumab as starting anti-TNF-α therapy in childhood chronic uveitis. Pediatr Rheumatol Online J 11:16. doi:10.1186/1546-0096-11-16
García-De-Vicuña C, Díaz-Llopis M, Salom D et al (2013) Usefulness of adalimumab in the treatment of refractory uveitis associated with juvenile idiopathic arthritis. Mediat Inflamm 2013:560632. doi:10.1155/2013/560632
Lerman MA, Lewen MD, Kempen JH et al (2015) Uveitis reactivation in children treated with tumor necrosis factor alpha inhibitors. Am J Ophthalmol 160:193–200.e1. doi:10.1016/j.ajo.2015.04.016
Schmeling H, Minden K, Foeldvari I et al (2014) Efficacy and safety of adalimumab as the first and second biologic agent in juvenile idiopathic arthritis: the German Biologics JIA Registry. Arthritis Rheumatol 66:2580–2589. doi:10.1002/art.38741
Tarkiainen M, Tynjälä P, Vähäsalo P et al (2015) Occurrence of adverse events in patients with JIA receiving biologic agents: long-term follow-up in a real-life setting. Rheumatology (Oxford, England) 54:1170–1176. doi:10.1093/rheumatology/keu457
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Funding
No funding was received for this research.
Ethical approval
This study was conducted as a retrospective trial. For this type of study formal consent is not required.
Additional information
Marc Breitbach and Christoph Tappeiner contributed equally to this work.
Rights and permissions
About this article
Cite this article
Breitbach, M., Tappeiner, C., Böhm, M.R.R. et al. Discontinuation of long-term adalimumab treatment in patients with juvenile idiopathic arthritis-associated uveitis. Graefes Arch Clin Exp Ophthalmol 255, 171–177 (2017). https://doi.org/10.1007/s00417-016-3497-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3497-5