Abstract
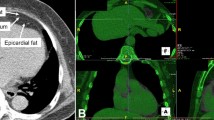
Patients with schizophrenia are at increased risk of diabetes, cardiovascular disease (CVD) and associated mortality versus the general population. Increased intra-abdominal and pericardial adipose tissue are associated with elevated CVD and mortality in the general population, but little is known about these in patients with schizophrenia. This study examined pericardial and intra-abdominal adipose tissue in schizophrenia and compared this to healthy controls. Thirty-one patients with schizophrenia (mean age 41.2 years, 76% males) and 30 healthy volunteers (CTRL) were examined in this study. The primary outcomes were the volumes of pericardial adipose tissue and intra-abdominal adipose tissue, measured using magnetic resonance imaging. Secondary outcomes included diabetes and cardiac event risk assessed by established instruments. Volumes of pericardial adipose tissue were increased in male and female patients with schizophrenia compared to healthy controls after the adjustment of age, sex and body mass index (P < 0.005). The 10-year risk of a cardiac event was significantly higher in patients with schizophrenia. Furthermore, the risk for developing type-2 diabetes mellitus was slightly increased in schizophrenia. Volumes of intra-abdominal adipose tissue were slightly increased in male and female patients with schizophrenia, albeit not statistically significant. This study demonstrates that patients with schizophrenia have increased pericardial adipose tissue versus controls. This increased fat deposit around the heart is highly relevant for understanding the comorbidity between heart disease and schizophrenia. Interventions aiming to reduce pericardial and intra-abdominal adipose tissue, such as exercise, may be essential to reduce the burden of heart disease in schizophrenia.


Similar content being viewed by others
References
Alexopoulos N, Katritsis D, Raggi P (2014) Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis 233(1):104–112
Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamathee SG (2014) Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc 62(2):253–260
Björntorp P, Rosmond R (1999) Visceral obesity and diabetes. Drugs 58(Suppl 1):13–18
Chen DC, Zhou MA, Zhou DH, Xiu MH, Wu GY, Kosten et al (2011) Gender differences in the prevalence of diabetes mellitus in chronic hospitalized patients with schizophrenia on long-term antipsychotics. Psychiatry Res 186(2–3):451–453
Correll CU, Solmi M, Veronese N, Bortolato B, Santonastaso P, Thapa-Chhetri N et al (2017) Prevalence, incidence and mortality from cardovascular disease in patients with pooled and specific severe mental illness: a large scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 16(2):163–180
Cuppett M, Latin RW (2002) A survey of physical activity levels of certified athletic trainers. J Athl Train 37(3):281–285
De Hert M, Dekker JM, Wood D, Kahl KG, Holt RIG, Möller H-J (2009) Cardiovascular disease and diabetes in patients with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry 24(6):412–424
Ding J, Hsu F-C, Harris TB, Liu Y, Kritchevsky SB, Szklo M et al (2009) The association of pericardial fat with incident coronary heart disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 90(3):499–504
Fan Z, Wu Y, Shen J, Ji T, Zhan R (2013) Schizophrenia and the risk of cardiovascular diseases: a meta-analysis of thirteen cohort studies. J Psychiatr Res 47(11):1549–1556
Galling B, Roldán A, Nielsen RE, Nielsen J, Gerhard T, Carbon M et al (2016) Type 2 diabetes mellitus in youth exposed to antipsychotics: a systematic review and meta-analysis. JAMA Psychiatry 73(3):247–259
Gilles M, Hentschel F, Paslakis G, Glahn V, Lederbogen F, Deuschle M (2010) Visceral and subcutaneous fat in patients treated with olanzapine: a case series. Clin Neuropharmacol 33(5):248–249
Heald A, Pendlebury J, Anderson S, Narayan V, Guy M, Gibson M et al (2017) Lifestyle factors and the metabolic syndrome in Schizophrenia: a cross-sectional study. Ann Gen Psychiatry 16:12
Hyuk Kim T, Hoon Yu S, Hee Choi S, Won Yoon J, Mee Kang S, Ju Chun et al (2011) Pericardial fat amount is an independent risk factor of coronary artery stenosis assessed by multidetector-row computed tomography: The Korean Atherosclerosis Study 2. Obesity 19(5):1028–1034
Iacobellis G, Singh N, Wharton S, Sharma AM (2008) Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity 16(7):1693–1697
Kahl KG, Hueper K, Schweiger U, Gutberlet M, Detlef A-M, Weiss C et al (2014) Pericardial, intra-abdominal, and subcutaneous adipose tissue in patients with major depressive disorder. Acta Psychiatr Scand 130(2):137–143
Kahl KG, Schweiger U, Correll C, Müller C, Busch ML, Bauer et al (2015) Depression, anxiety disorders, and metabolic syndrome in a population at risk for type 2 diabetes mellitus. Brain Behav 5(3):e00306
Kahl KG, Kerling A, Tegtbur U, Gützlaff E, Herrmann J, Borchert L et al (2016) Effects of additional exercise training on epicardial, intra-abdominal and subcutaneous adipose tissue in major depressive disorder: a randomzied pilot study. J Affect Disord 1(192):91–97
Katsiki N, Athyros VG, Mikhailidis DP (2016) Abnormal peri-organ or intra-organ fat (APIFat) deposition: an underestimated predictor of vascular risk? Curr Vasc Pharmacol 14(5):432–441
Kim M-K, Tomita T, Kim M-J, Sasai H, Maeda S, Tanaka K (2009) Aerobic exercise training reduces epicardial fat in obese men. J Appl Physiol 106(1):5–11
Konarzewska B, Stefańska E, Wendołowicz A, Cwalina U, Golonko A, Małus A et al (2014) Visceral obesity in normal-weight patients suffering from chronic schizophrenia. BMC Psychiatry 14:35
Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R et al (2006) Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14(2):336–341
Miao C, Chen S, Ding J, Liu K, Li D, Macedo R et al (2011) The association of pericardial fat with coronary artery plaque index at MR imaging: The Multi-Ethnic Study of Atherosclerosis (MESA). Radiology 261(1):109–111
Misawa F, Shimizu K, Fujii Y, Miyata R, Koshiishi F, Kobayashi M et al (2011) Is antipsychotic polypharmacy associated with metabolic syndrome even after adjustment for lifestyle effects?: a cross-sectional study. BMC Psychiatry 11:118
Mitchell AJ, Vancampfort D, Sweers K, Van Winkel R, Yu W, De Hert M (2013) Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders-a systematic review and meta-analysis. Schizophr Bull 39(2):306–318
Nicklas BJ, Penninx BWJH, Cesari M, Kritchevsky SB, Newman AB, Kanaya AM et al (2004) Association of visceral adipose tissue with incident myocardial infarction in older men and women: the health, aging and body composition study. Am J Epidemiol 160(8):741–749
Poulin MJ, Chaput JP, Simard V, Vincent P, Bernier J, Gauthier Y et al (2007) Management of antipsychotic-incluced weight gain: prospective naturalistic study of the effectiveness of a supervised exercise programme. Aust N Z J Psychiatry 41(12):980–989
Ryan MCM, Flanagan S, Kinsella U, Keeling F, Thakore JH (2004) The effects of atypical antipsychotics on visceral fat distribution in first episode, drug-naive patients with schizophrenia. Life Sci 74(16):1999–2008
Stubbs B, Firth J, Berry A, Schuch FB, Rosenbaum S, Gaughran F et al (2016) How much physical activity do patients with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res 176(2):431–440
Stubbs B, Williams J, Gaughran F, Craig T (2016) How sedentary are patients with psychosis? A systematic review and meta-analysis. Schizophr Res 171(1–3):103–109
Stubbs B, Vancampfort D, De Hert M, Mitchell AJ (2015) The prevalence and predictors of type two diabetes mellitus in patients with schizophrenia: a systematic review and comparative meta-analysis. Acta Psychiatr Scand 132(2):144–157
Tadros T, Massaro J, Rosito G, Hoffmann U, Vasan R, Larson M et al (2010) Pericardial fat volume correlates with inflammatory markers: The Framingham Heart Study. Obesity 18(5):1039–1045
Thakore JH, Mann JN, Vlahos I, Martin A, Reznek R (2002) Increased visceral fat distribution in drug-naive and drug-free patients with schizophrenia. Int J Obes Relat Metab Disord 26(1):137–141
Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB et al (2015) Risk of metabolic syndrome and its components in patients with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry 14(3):339–347
Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB et al (2016) Diabetes mellitus in patients with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta-analysis. World Psychiatry 15(2):166–174
Vancampfort D, Rosenbaum S, Schuch F, Ward PB, Richards J, Mugisha J et al (2017) Cardiorespiratory fitness in severe mental illness: A Systematic Review and Meta-analysis. Sports Med 47(2):343–352
Walker ER, McGee RE, Druss BG (2015) Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 72(4):334–341
Wannamathee SG, Atkins JL (2015) Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc 74(4):405–412
Willens HJ, Byers P, Chirinos JA, Labrador E, Hare JM, de Marchena E (2007) Effects of weight loss after bariatric surgery on epicardial fat measured using echocardiography. Am J Cardiol 99(9):1242–1245
Yun CH, Lin TY, Wu YJ, Liu CC, Kuo JY, Yeh HI et al (2012) Pericardial and thoracic peri-aortic adipose tissue contributes to systemic inflammation and calcified coronary artherosclerosis independent of body fat composition, anthropometric measures and traditional cardiovascular risks. Eur J Radiol 81(4):749–756
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V (2008) Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis 18(5):388–395
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Ruppert, J., Hartung, D., Westhoff-Bleck, M. et al. Increased pericardial adipose tissue and cardiometabolic risk in patients with schizophrenia versus healthy controls. Eur Arch Psychiatry Clin Neurosci 268, 719–725 (2018). https://doi.org/10.1007/s00406-017-0858-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-017-0858-y