Abstract
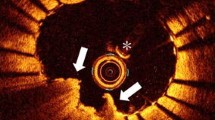
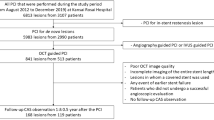
Although drug-eluting stents have improved clinical outcomes, percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) remains a challenging procedure in terms of thrombus management. A new-generation P2Y12 receptor inhibitor, prasugrel, provides more rapid and potent antiplatelet action compared with clopidogrel. Prasugrel achieved significant reduction of ischemic events compared with clopidogrel in ACS. The aim of this optical coherence tomography (OCT) study was to evaluate temporal changes in tissue prolapse after stenting under different antiplatelet regimens (aspirin plus prasugrel or clopidogrel) in ACS patients. A total of 119 ACS patients were randomized to either prasugrel or clopidogrel at the time of PCI. OCT analysis was available in 119 patients at baseline (just after stenting), 77 patients at 2 weeks, and 62 patients at 4 months after stenting. Cross-sectional analysis for every 1 mm was performed at in-stent and adjacent reference segment. Tissue prolapse area was calculated by lumen area minus stent area within the stented segment. Baseline patient and procedural characteristics were not different between the prasugrel and clopidogrel groups. Tissue prolapse area was significantly lower in the prasugrel compared with the clopidogrel group after stenting (0.24 ± 0.23 vs. 0.36 ± 0.23 mm2, p = 0.003) and at 2 weeks (0.11 ± 0.13 vs. 0.19 ± 0.16 mm2, p = 0.005). However, there was no significant difference at 4 months. In conclusion, our study suggests prasugrel was effective in reducing tissue prolapse in the super acute phase in ACS patients compared with clopidogrel. However, the effect of tissue prolapse reduction was not different up to 4 months follow-up.





Similar content being viewed by others
References
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O'Gara PT, Sabatine MS, Smith PK, Smith SC Jr (2016) 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Circulation 134:e123–155
Saito S, Isshiki T, Kimura T, Ogawa H, Yokoi H, Nanto S, Takayama M, Kitagawa K, Nishikawa M, Miyazaki S, Nakamura M (2014) Efficacy and safety of adjusted-dose prasugrel compared with clopidogrel in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. Circ J 78:1684–1692
Steinhubl SR, Berger PB, Mann JT 3rd, Fry ET, DeLago A, Wilmer C, Topol EJ, Investigators C (2002) Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 288:2411–2420
Jang IK, Bouma BE, Kang DH, Park SJ, Park SW, Seung KB, Choi KB, Shishkov M, Schlendorf K, Pomerantsev E, Houser SL, Aretz HT, Tearney GJ (2002) Visualization of coronary atherosclerotic plaques in patients using optical coherence tomography: comparison with intravascular ultrasound. J Am Coll Cardiol 39:604–609
Kubo T, Akasaka T, Shite J, Suzuki T, Uemura S, Yu B, Kozuma K, Kitabata H, Shinke T, Habara M, Saito Y, Hou J, Suzuki N, Zhang S (2013) OCT compared with IVUS in a coronary lesion assessment: the OPUS-CLASS study. J Am Coll Cardiol Img 6:1095–1104
Ozaki Y, Katagiri Y, Onuma Y, Amano T, Muramatsu T, Kozuma K, Otsuji S, Ueno T, Shiode N, Kawai K, Tanaka N, Ueda K, Akasaka T, Hanaoka KI, Uemura S, Oda H, Katahira Y, Kadota K, Kyo E, Sato K, Sato T, Shite J, Nakao K, Nishino M, Hikichi Y, Honye J, Matsubara T, Mizuno S, Muramatsu T, Inohara T, Kohsaka S, Michishita I, Yokoi H, Serruys PW, Ikari Y, Nakamura M, Task Force on Primary Percutaneous Coronary Intervention of the Japanese Cardiovascular Interventional T (2018) CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) in 2018. Cardiovasc Interv Ther 33:178–203
Shimoda M, Ando H, Naito K, Suzuki A, Sakurai S, Nakano Y, Kurita A, Waseda K, Takashima H, Murotani K, Uetani T, Amano T (2018) Early-phase vascular healing of bioabsorbable vs. durable polymer-coated everolimus-eluting stents in patients with ST-elevation myocardial infarction- 2-week and 4-month analyses with optical coherence tomography. Circ J 82:2594–2601
Soeda T, Uemura S, Park SJ, Jang Y, Lee S, Cho JM, Kim SJ, Vergallo R, Minami Y, Ong DS, Gao L, Lee H, Zhang S, Yu B, Saito Y, Jang IK (2015) Incidence and clinical significance of poststent optical coherence tomography findings: one-year follow-up study from a multicenter registry. Circulation 132:1020–1029
Palmerini T, Biondi-Zoccai G, Della Riva D, Stettler C, Sangiorgi D, D'Ascenzo F, Kimura T, Briguori C, Sabate M, Kim HS, De Waha A, Kedhi E, Smits PC, Kaiser C, Sardella G, Marullo A, Kirtane AJ, Leon MB, Stone GW (2012) Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet 379:1393–1402
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM, Investigators T-T (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Hong YJ, Jeong MH, Choi YH, Song JA, Kim DH, Lee KH, Yamanaka F, Lee MG, Park KH, Sim DS, Yoon NS, Yoon HJ, Kim KH, Park HW, Kim JH, Ahn Y, Cho JG, Park JC, Kang JC (2013) Impact of tissue prolapse after stent implantation on short- and long-term clinical outcomes in patients with acute myocardial infarction: an intravascular ultrasound analysis. Int J Cardiol 166:646–651
Prati F, Romagnoli E, Gatto L, La Manna A, Burzotta F, Limbruno U, Versaci F, Fabbiocchi F, Di Giorgio A, Marco V, Ramazzotti V, Di Vito L, Trani C, Porto I, Boi A, Tavazzi L, Mintz GS (2016) Clinical impact of suboptimal stenting and residual intrastent plaque/thrombus protrusion in patients with acute coronary syndrome: The CLI-OPCI ACS substudy (Centro per la Lotta Contro L'Infarto-Optimization of Percutaneous Coronary Intervention in Acute Coronary Syndrome). Circ Cardiovasc Interv 9:e003726
Brandt JT, Close SL, Iturria SJ, Payne CD, Farid NA, Ernest CS 2nd, Lachno DR, Salazar D, Winters KJ (2007) Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost 5:2429–2436
Umemura K, Iwaki T (2016) The pharmacokinetics and pharmacodynamics of prasugrel and clopidogrel in healthy Japanese volunteers. Clin Pharmacol Drug Dev 5:480–487
Farid NA, Kurihara A, Wrighton SA (2010) Metabolism and disposition of the thienopyridine antiplatelet drugs ticlopidine, clopidogrel, and prasugrel in humans. J Clin Pharmacol 50:126–142
Rollini F, Franchi F, Hu J, Kureti M, Aggarwal N, Durairaj A, Park Y, Seawell M, Cox-Alomar P, Zenni MM, Guzman LA, Suryadevara S, Antoun P, Bass TA, Angiolillo DJ (2016) Crushed prasugrel tablets in patients with STEMI undergoing primary percutaneous coronary intervention: The CRUSH Study. J Am Coll Cardiol 67:1994–2004
Jinnai T, Horiuchi H, Makiyama T, Tazaki J, Tada T, Akao M, Ono K, Hoshino K, Naruse Y, Takahashi K, Watanabe H, Kita T, Kimura T (2009) Impact of CYP2C19 polymorphisms on the antiplatelet effect of clopidogrel in an actual clinical setting in Japan. Circ J 73:1498–1503
Ogawa H, Isshiki T, Kimura T, Yokoi H, Nanto S, Takayama M, Kitagawa K, Nishikawa M, Miyazaki S, Ikeda Y, Nakamura M, Tanaka Y, Saito S (2016) Effects of CYP2C19 allelic variants on inhibition of platelet aggregation and major adverse cardiovascular events in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. J Cardiol 68:29–36
Kajander OA, Koistinen LS, Eskola M, Huhtala H, Bhindi R, Niemela K, Jolly SS, Sheth T, Total-Oct Substudy Investigators (2015) Feasibility and repeatability of optical coherence tomography measurements of pre-stent thrombus burden in patients with STEMI treated with primary PCI. Eur Heart J Cardiovasc Imaging 16:96–107
Lee T, Yonetsu T, Koura K, Hishikari K, Murai T, Iwai T, Takagi T, Iesaka Y, Fujiwara H, Isobe M, Kakuta T (2011) Impact of coronary plaque morphology assessed by optical coherence tomography on cardiac troponin elevation in patients with elective stent implantation. Circ Cardiovasc Interv 4:378–386
Sugiyama T, Kimura S, Akiyama D, Hishikari K, Kawaguchi N, Kamiishi T, Hikita H, Takahashi A, Isobe M (2014) Quantitative assessment of tissue prolapse on optical coherence tomography and its relation to underlying plaque morphologies and clinical outcome in patients with elective stent implantation. Int J Cardiol 176:182–190
Acknowledgements
The authors thank Heidi N. Bonneau, RN, MS, CCA, for her review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Naito, K., Nakano, Y., Waseda, K. et al. Impact of antiplatelet therapy on tissue prolapse at super acute phase after stenting: serial OCT study in acute coronary syndrome patients. Heart Vessels 36, 200–210 (2021). https://doi.org/10.1007/s00380-020-01686-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-020-01686-x