Abstract
Objectives
Pulmonary parametric response map (PRM) was proposed for quantitative densitometric phenotypization of chronic obstructive pulmonary disease. However, little is known about this technique in healthy subjects. The purpose of this study was to describe the normal spectrum of densitometric classification of pulmonary PRM in a group of healthy adults.
Methods
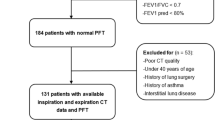
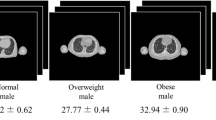
15 healthy volunteers underwent spirometrically monitored chest CT at total lung capacity (TLC) and functional residual capacity (FRC). The paired CT scans were analyzed by PRM for voxel-by-voxel characterization of lung parenchyma according to 4 densitometric classifications: normal lung (TLC ≥ -950 HU, FRC ≥ -856 HU); expiratory low attenuation area (LAA) (TLC ≥ -950 HU, FRC < -856 HU); dual LAA (TLC<-950 HU, FRC < -856 HU); uncharacterized (TLC < -950 HU, FRC ≥ -856 HU).
Results
PRM spectrum was 78 % ± 10 % normal lung, 20 % ± 8 % expiratory LAA, and 1 % ± 1 % dual LAA. PRM was similar between genders, there was moderate correlation between dual LAA and spirometrically assessed TLC (R = 0.531; p = 0.042), and between expiratory LAA and VolExp/Insp ratio (R = -0.572; p = 0.026).
Conclusions
PRM reflects the predominance of normal lung parenchyma in a group of healthy volunteers. However, PRM also confirms the presence of physiological expiratory LAA seemingly related to air trapping and a minimal amount of dual LAA likely reflecting emphysema.
Key points
• Co-registration of inspiratory and expiratory computed tomography allows dual-phase densitometry.
• Dual-phase co-registered densitometry reflects heterogeneous regional changes in lung function.
• Quantification of lung in healthy subjects is needed to set reference values.
• Expiratory low attenuation areas <30 % could be considered within normal range.





Similar content being viewed by others
Abbreviations
- ATS:
-
American Thoracic Society
- BMI:
-
body mass index
- COPD:
-
chronic obstructive pulmonary disease
- ERS:
-
European Respiratory Society
- FRC:
-
functional residual capacity
- LAA:
-
low attenuation area
- PRM:
-
parametric response map
- QCT:
-
quantitative computed tomography
- SD:
-
standard deviation
- TLC:
-
total lung capacity
- VolExp/Insp ratio:
-
ratio between expiratory and inspiratory lung volume
References
Moffat BA, Chenevert TL, Lawrence TS et al (2005) Functional diffusion map: a noninvasive MRI biomarker for early stratification of clinical brain tumor response. Proc Natl Acad Sci U S A 102:5524–5529
Galban CJ, Han MK, Boes JL et al (2012) Computed tomography-based biomarker provides unique signature for diagnosis of COPD phenotypes and disease progression. Nat Med 18:1711–1715
Dufresne V, Knoop C, Van Muylem A et al (2009) Effect of systemic inflammation on inspiratory and limb muscle strength and bulk in cystic fibrosis. Am J Respir Crit Care Med 180:153–158
Nemec SF, Molinari F, Dufresne V, Gosset N, Silva M, Bankier AA (2015) Comparison of four software packages for CT lung volumetry in healthy individuals. Eur Radiol. doi:10.1007/s00330-014-3557-3
Pellegrino R, Viegi G, Brusasco V et al (2005) Interpretative strategies for lung function tests. Eur Respir J 26:948–968
Wanger J, Clausen JL, Coates A et al (2005) Standardisation of the measurement of lung volumes. Eur Respir J 26:511–522
Bankier AA, O'Donnell CR, Boiselle PM (2008) Quality initiatives. Respiratory instructions for CT examinations of the lungs: a hands-on guide. Radiographics 28:919–931
Mets OM, Zanen P, Lammers JW et al (2012) Early identification of small airways disease on lung cancer screening CT: comparison of current air trapping measures. Lung 190:629–633
Schroeder JD, McKenzie AS, Zach JA et al (2013) Relationships between airflow obstruction and quantitative CT measurements of emphysema, air trapping, and airways in subjects with and without chronic obstructive pulmonary disease. AJR Am J Roentgenol 201:W460–W470
Bankier AA, De Maertelaer V, Keyzer C, Gevenois PA (1999) Pulmonary emphysema: subjective visual grading versus objective quantification with macroscopic morphometry and thin-section CT densitometry. Radiology 211:851–858
Irion KL, Marchiori E, Hochhegger B et al (2009) CT quantification of emphysema in young subjects with no recognizable chest disease. AJR Am J Roentgenol 192:W90–W96
Mets OM, van Hulst RA, Jacobs C, van Ginneken B, de Jong PA (2012) Normal range of emphysema and air trapping on CT in young men. AJR Am J Roentgenol 199:336–340
Zach JA, Newell JD Jr, Schroeder J et al (2012) Quantitative computed tomography of the lungs and airways in healthy nonsmoking adults. Investig Radiol 47:596–602
Bankier AA, Van Muylem A, Knoop C, Estenne M, Gevenois PA (2001) Bronchiolitis obliterans syndrome in heart-lung transplant recipients: diagnosis with expiratory CT. Radiology 218:533–539
Wan ES, Hokanson JE, Murphy JR et al (2011) Clinical and radiographic predictors of GOLD-unclassified smokers in the COPDGene study. Am J Respir Crit Care Med 184:57–63
Copley SJ, Wells AU, Hawtin KE et al (2009) Lung morphology in the elderly: comparative CT study of subjects over 75 years old versus those under 55 years old. Radiology 251:566–573
Lee KW, Chung SY, Yang I, Lee Y, Ko EY, Park MJ (2000) Correlation of aging and smoking with air trapping at thin-section CT of the lung in asymptomatic subjects. Radiology 214:831–836
Acknowledgments
The scientific guarantor of this publication is Dr Mario Silva. The authors of this manuscript declare relationships with the following companies: A. A. Bankier is consultant for Spiration (Olympus Medical Systems) and has received authorship honoraria from Elsevier. R. Chamberlain is employed at Imbio, LLC (Minneapolis, MN). Imbio received NIH grant for validation of parametric response map (NIH R44HL118837).
The authors state that this work has not received any funding. Professor Dr. Alexander A. Bankier has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Our study population has been previously reported in “Dufresne V. et al. Effect of systemic inflammation on inspiratory and limb muscle strength and bulk in cystic fibrosis. Am J Respir Crit Care Med 2009” and “Nemec SF et al. Comparison of four software packages for CT lung volumetry in healthy individuals. Eur Radiol 2015”. Methodology: retrospective, experimental, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva, M., Nemec, S.F., Dufresne, V. et al. Normal spectrum of pulmonary parametric response map to differentiate lung collapsibility: distribution of densitometric classifications in healthy adult volunteers. Eur Radiol 26, 3063–3070 (2016). https://doi.org/10.1007/s00330-015-4133-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4133-1