Abstract
Objective
To assess anatomical risk factors in patients after lateral patellar dislocation (LPD) and controls using MRI.
Methods
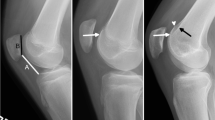
MR images of 186 knees after LPD and of 186 age- and gender-matched controls were analysed. The presence of trochlear dysplasia was assessed by evaluation of trochlear inclination, facet asymmetry, and trochlear depth; patella alta was evaluated by the Insall-Salvati index and Caton-Deschamps index; the lateralised force vector was measured by the tibial tuberosity-trochlear groove (TT-TG) distance.
Results
Compared with controls, dislocators had significantly lower values for all three parameters of trochlear dysplasia (−32 %, −32 %, −44 %) and significantly higher values for patella alta (+14 %,+13 %) and TT-TG (+49 %) (all P < 0.001). Trochlear dysplasia was observed in 112 dislocators (66 %), of whom 61 (36 %) additionally had patella alta and 15 (9 %) an abnormal TT-TG. As isolated risk factors, patella alta (15 %) and abnormal TT-TG (1 %) were rare. Only 25 dislocators (15 %) had no anatomical risk factors. Trochlear dysplasia in conjunction with abnormal TT-TG or patella alta is associated with a 37- and 41-fold higher risk.
Conclusion
Most dislocators have anatomical risk factors, varying in severity and constellation.
Key Points
• Magnetic resonance imaging provides unique information about anatomical variation within the knee.
• Anatomical variants increase the risk for lateral patellar dislocation (LPD)
• Trochlear dysplasia is the main risk factor for LPD.
• Patellar alta and abnormal tibial tuberosity-trochlear groove distance may be additional factors.
• Patient-specific evaluation of risk factors following LPD may help future management.





Similar content being viewed by others
References
Redziniak DE, Diduch DR, Mihalko WM et al (2009) Patellar instability. J Bone Joint Surg Am 91:2264–2275
Fithian DC, Paxton EW, Stone ML et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Vollnberg B, Koehlitz T, Jung T et al (2012) Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Eur Radiol 22:2347–2356
von Engelhardt LV, Raddatz M, Bouillon B et al (2010) How reliable is MRI in diagnosing cartilaginous lesions in patients with first and recurrent lateral patellar dislocations? BMC Musculoskelet Disord 11:149
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90:2751–2762
Mulford JS, Wakeley CJ, Eldridge JD (2007) Assessment and management of chronic patellofemoral instability. J Bone Joint Surg Br 89:709–716
White BJ, Sherman OH (2009) Patellofemoral instability. Bull NYU Hosp Jt Dis 67:22–29
Diederichs G, Issever AS, Scheffler S. MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics 30:961–981
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA (2000) Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 216:582–585
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225:736–743
Escala JS, Mellado JM, Olona M, Gine J, Sauri A, Neyret P (2006) Objective patellar instability: MR-based quantitative assessment of potentially associated anatomical features. Knee Surg Sports Traumatol Arthrosc 14:264–272
Pfirrmann CW, Zanetti M, Romero J, Hodler J (2000) Femoral trochlear dysplasia: MR findings. Radiology 216:858–864
Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB (2011) The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee 18:185–188
Smith TO, Davies L, Toms AP, Hing CB, Donell ST (2011) The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skeletal Radiol 40:399–414
Balcarek P, Jung K, Ammon J et al (2010) Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 38:2320–2327
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Miller TT, Staron RB, Feldman F (1996) Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol 167:339–341
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68:317–325
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Barnett AJ, Prentice M, Mandalia V, Wakeley CJ, Eldridge JD (2009) Patellar height measurement in trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 17:1412–1415
Seil R, Muller B, Georg T, Kohn D, Rupp S (2000) Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc 8:231–236
Insall J, Goldberg V, Salvati E (1972) Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res 88:67–69
Balcarek P, Ammon J, Frosch S et al (2010) Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy 26:926–935
Tsujimoto K, Kurosaka M, Yoshiya S, Mizuno K (2000) Radiographic and computed tomographic analysis of the position of the tibial tubercle in recurrent dislocation and subluxation of the patella. Am J Knee Surg 13:83–88
Pandit S, Frampton C, Stoddart J, Lynskey T (2011) Magnetic resonance imaging assessment of tibial tuberosity-trochlear groove distance: normal values for males and females. Int Orthop 35:1799–1803
Acknowledgements
Edzard Wiener and Gerd Diederichs contributed equally to this article.
Two additional research projects were carried out in subgroups of this cohort: (1) One subgroup of the cohort received additional scans for rotational alignment of the lower limb. The manuscript with the title “MRI analysis of rotational alignment in patients with patellar dislocation” is accepted for publication in the American Journal of Sports Medicine. (2) Another subgroup was analysed for cartilage defects. This article entitled “Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation” was already published in European Radiology (DOI 10.1007/s00330-012-2493-3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Köhlitz, T., Scheffler, S., Jung, T. et al. Prevalence and patterns of anatomical risk factors in patients after patellar dislocation: a case control study using MRI. Eur Radiol 23, 1067–1074 (2013). https://doi.org/10.1007/s00330-012-2696-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2696-7