Abstract
Purpose
We evaluated the safety and efficacy of biweekly capecitabine in combination with oxaliplatin in previously untreated patients with locally advanced or metastatic gastric cancer.
Methods
Patients received oral capecitabine 1,000 mg/m2 twice daily on days 1–10 plus oxaliplatin 85 mg/m2 as a 2-h intravenous infusion on day 1, every 2 weeks (XELOX). The primary endpoint was overall response rate. Secondary endpoints included progression-free survival, overall survival, and toxicity.
Results
From March 2007 to October 2010, 46 patients were enrolled in this phase II study. The median age was 64 years (range 32–85). A total of 391 (median 7.5, range 1–29) cycles were delivered. Among the 41 patients evaluable for tumor response, 9 showed partial response and 25 had stable disease. The overall response rates of the evaluable and intent-to-treat (ITT) populations were 22 % (95 % CI 10–42 %) and 20 % (95 % CI 9–34 %), respectively. In the ITT analysis, the progression-free survival and overall survival were 5.6 months (95 % CI 4.1–6.3 months) and 8.0 months (95 % CI 6.3–10.1 months), respectively. The most common hematological toxicities were thrombocytopenia (35 %) and leucopenia (34 %), whereas the most common non-hematological toxicities were neuropathy (35 %), fatigue (33 %), diarrhea (27 %), vomiting (26 %), and hand-foot syndrome (25 %). Major grade 3–4 toxicities were anemia (11 %), diarrhea (9 %), and hand-foot syndrome (7 %). No patient died of treatment-related toxicities.
Conclusions
Although the biweekly XELOX regimen failed its primary response rate endpoint, it showed modest efficacy and an acceptable safety profile in the treatment of advanced gastric cancer.
Similar content being viewed by others
Introduction
Gastric cancer is the fourth most common and the second leading cause of cancer deaths in the world. According to global estimates, gastric cancer was newly diagnosed in approximately 989,600 people and caused approximately 738,000 deaths in 2008, with the highest rates occurring in Eastern Asia [1]. Although early diagnosis of gastric cancer has improved, most patients still show locally advanced or metastatic disease upon diagnosis. Even if surgery is performed with a curative intent, 60 % of patients with resectable tumors will ultimately relapse [2].
It has been demonstrated that combination chemotherapy regimens in advanced gastric cancer improve overall survival and progression-free survival of patients and maintain quality of life [3]. 5-Fluorouracil (5-FU) in combination with cisplatin is a generally accepted standard treatment option for advanced gastric cancer patients [4–8]. The combination regimen of 5-FU and cisplatin achieves overall response rates of 20–51 %, median progression-free survival of 3.3–6.5 months, and median overall survival of 7–11 months [4–8]. Nevertheless, the required weekly 24-h intravenous infusion of 5-FU is inconvenient, cumbersome, and associated with the risk of infection and thrombosis.
Capecitabine, a novel oral fluoropyrimidine designed to mimic the continuous infusion of 5-FU, is administered orally. After oral administration, it is efficiently absorbed from the gastrointestinal tract and metabolized primarily in the liver. Capecitabine is then sequentially converted to the cytotoxic 5-FU moiety in tumor tissues by the enzyme thymidine phosphorylase, which shows significantly higher activities in tumors than in normal tissues [9, 10]. In several phase II studies, capecitabine has shown good response rates in advanced gastric cancer patients when provided as monotherapy or in combination with cisplatin, achieving response rates of 19–34 and 55 %, respectively [11–14]. Oral fluoropyrimidine administration can eliminate the inconvenience and the risks (i.e., venous thrombosis and sepsis) associated with the infusion of 5-FU. Furthermore, capecitabine showed non-inferior effects compared with 5-FU in gastric cancer patients [15].
Oxaliplatin, initially developed to treat colorectal cancer, is an alkylating agent that forms adducts between two adjacent guanines or a guanine and an adenine residue, leading to the inhibition of DNA replication [16]. Compared with cisplatin, oxaliplatin appears to have a more favorable tolerability profile. In particular, renal toxicity and ototoxicity are not associated with oxaliplatin, but are commonly encountered during cisplatin therapy [17]. The dose-limiting toxicity of oxaliplatin is a cumulative sensory peripheral neuropathy. In randomized phase III trials, oxaliplatin was non-inferior to cisplatin in the treatment of esophagogastric cancer [18, 19].
Triweekly oxaliplatin plus oral capecitabine has become a new standard for the treatment of advanced gastric cancer [20–25], achieving response rates of 42–63 % in published phase II studies [20–24]. These results warrant further investigation into this drug combination in patients with gastrointestinal malignancies. A biweekly regimen of the same chemotherapy combination has been shown to be effective in metastatic colorectal cancer [26], but biweekly data are currently not available for advanced gastric cancer. The aim of this study was to demonstrate the efficacy and safety of a biweekly regimen of capecitabine in combination with oxaliplatin in previously untreated patients with locally advanced or metastatic gastric cancer.
Patients and methods
Study design
This is a multicenter study to investigate the safety and efficacy profiles of biweekly capecitabine (Xeloda®) in combination with oxaliplatin (Eloxatin®) as first-line therapy in patients with locally advanced or metastatic gastric cancer. The primary objective was to investigate the objective response rate of capecitabine plus oxaliplatin treatment in previously untreated locally advanced or metastatic gastric cancer patients. Secondary objectives included progression-free survival, duration of response, overall survival (OS), and safety profiles. The study protocol was approved by the medical ethics committees of all participating centers and was registered as ClinicalTrial.gov (NCT00436241). Signed informed consents were obtained from all patients.
Patients
Inclusion criteria for this study were as follows: histologically confirmed gastric adenocarcinoma with unresectable locally advanced or metastatic disease; at least one, non-irradiated, measurable lesion according to the Response Evaluation Criteria in Solid Tumors (RECIST) [27]; 18 years of age or older; calculated creatinine clearance ≥50 ml/min using the Cockroft–Gault formula; and Eastern Cooperative Oncology Group (ECOG) performance status ≤1.
Patients who fell under any of the following criteria were excluded from the study: previous cytotoxic chemotherapy (except given as adjuvant or neoadjuvant treatment completed at least 6 months prior to enrollment); organ allografts; clinically significant cardiac disease or myocardial infarction within the last 12 months; evidence of CNS metastases; history of another malignancy within the last five years except for cured basal cell carcinoma of the skin or cured carcinoma in situ of the uterine cervix; radiotherapy within 4 weeks of treatment start; major surgery within 4 weeks of the start of the treatment, without complete recovery; serious uncontrolled intercurrent infections; lack of physical integrity of the upper gastrointestinal tract or malabsorption syndrome; abnormal audiogram or auditory abnormality; significant or uncontrolled gastrointestinal bleeding; the following laboratory values: neutrophils ≤1.5 × 109/L; platelet count <100 × 109/L; serum bilirubin ≥1.5 × upper normal limit; alanine aminotransferase or aspartate aminotransferase >2.5 × upper normal limit or >5 × upper normal limit in the case of liver metastases; alkaline phosphatase >2.5 × upper normal limit or >5 × upper normal limit in the case of liver metastases or >10 × upper normal limit in the case of bone disease.
Treatment schedule
Capecitabine (1,000 mg/m2 twice daily, days 1–10, followed by four days of rest period) plus oxaliplatin (85 mg/m2 as a 2-h intravenous infusion on day 1) were administered in two-week cycles. Protocol treatment was discontinued for patients with clearly documented progressive disease (PD) at any time due to insufficient therapeutic response. Patients who tolerated treatment and showed either complete response (CR), partial response (PR), or stable disease (SD) continued to be treated and followed until disease progression.
Dose modification for adverse events
The intensity of clinical adverse events was graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events v3.0 (CTCAE). Dose modifications were based on hematological and non-hematological toxicities.
For hematological toxicities, dose modifications were based on hematological parameters at the start of a treatment cycle. Administration of capecitabine was interrupted during a treatment cycle if a grade 3 or 4 hematological toxicity developed. The next treatment cycle could only start if hematological toxicity has recovered to grade ≤1. No dose reduction or interruption was required for anemia (non-hemolytic) as it could be satisfactorily managed by transfusions.
For non-hematological toxicities of capecitabine, if a grade 2 or 3 adverse event occurred, capecitabine was interrupted immediately; if a grade 4 non-hematological toxicity occurred, treatment was discontinued unless the investigator considered it to be in the best interest of the patient to continue at 50 % of the original dose, once toxicity has resolved to grade 0–1. The next treatment cycle could only start if non-hematological toxicity has recovered to grade ≤1. Capecitabine dose was reduced by 25 % for patients experiencing a second occurrence of a given grade 2 or any grade 3 event. The capecitabine dose was reduced by 50 % for patients who experienced a third occurrence of a given grade 2 or a second occurrence of a given grade 3 event. If the same toxicity occurred for a fourth time at grade 2 or a third time at grade 3, treatment was discontinued.
For grade <3 non-hematological toxicities of oxaliplatin, management was symptomatic, if possible. For grade ≥3 non-hematological adverse events, oxaliplatin was withheld for a maximum of 4 weeks until toxicities were resolved. After patients recovered from toxicity grade 3–2 or less, the dose of oxaliplatin was reduced to 65 mg/m2 in subsequent cycles. In case of no resolution to grade 2 or less after a maximum of 4 weeks from the planned date of the next cycle, oxaliplatin treatment was discontinued. In case of grade 4 toxicity, patients were removed from oxaliplatin treatment and followed until the resolution of the adverse event.
Evaluation of efficacy and toxicities
Evaluations, including the patient’s medical history, physical examination, complete blood count, blood chemistry, abdominal–pelvic computed tomography (CT) scan, and chest X-ray, were performed before chemotherapy. After starting the protocol treatment, blood chemistry and complete blood count were assessed prior to the start of each cycle. Tumor measurements were carried out after every 3 cycles of treatment or when progression was suspected. Confirmation of overall response (complete or partial response), when applicable, was done at a minimum of 4 weeks after the first response had been recorded. Tumor response was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) [27]. Toxicities were recorded according to the National Cancer Institute Common Terminology Criteria grading system version 3, starting at the time of study entry and ending 28 days after the last dose of medication was administered.
Statistical methods
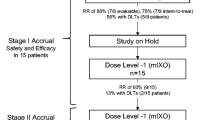
Simon’s two-stage optimal design was applied to calculate the sample size, assuming that the minimum response rate of capecitabine plus oxaliplatin in the study was 29 % and the expected overall response rate was at least 50 %. Under α = 0.05 and 80 % power, the estimated total evaluable patient number was 38 to detect more than 15 patients having partial response. Considering a 10 % drop-out rate, the estimated enrolled patient number was 42. Progression-free survival was measured as the duration from the date of starting protocol treatment to the date of first recording disease progression or the date of death, whichever occurred first. Overall survival was measured as the duration from the date of starting protocol treatment to the date of death. Duration of response was measured from the first date when measurement criteria were met for CR/PR to the first date when recurrent or progressive disease or death was objectively documented. Survival was estimated by the Kaplan–Meier analysis. All statistics were two-sided and performed using SAS software (version 9.2, SAS Inc., Cary, NC, USA).
Results
Patient’s characteristics
Between March 2007 and November 2008, forty-six patients (ITT population) from ten medical centers in Taiwan were enrolled in this study. The clinical and pathologic characteristics of patients are listed in Table 1.
Efficacy
The tumor response rates are shown in Table 2. Five patients could not be evaluated for response due to failure to return for tumor measurements. Among the 41 evaluable patients, the best tumor response was partial response (PR) in 9 patients, whereas 25 patients showed stable disease and 7 patients progressive disease. The overall response rates of the evaluable and intent-to-treat (ITT) populations were 22 % (95 % CI 10–42 %) and 20 % (95 % CI 9–34 %), respectively, whereas the disease control rates in the corresponding populations were 83 % (95 % CI 68–93 %) and 74 % (95 % CI 59–86 %), respectively. Median time to tumor response was 1.4 months (range 1.2–2.8 months). The median duration of response was 5.1 months (95 % CI 2.8–9.7 months). Of the 46 patients, 26 received second-line and subsequent therapies, with a total of 47 additional regimens received. Among them, six patients received monotherapy (2 UFUR, 1 capecitabine, 1 everolimus, 1 irinotecan, and 1 paclitaxel), 9 patients received cisplatin plus fluoropyrimidine-based therapy, 4 patients received anthracycline-based therapy with various combinations of 5-FU, cisplatin, and cyclophosphamide, 4 patients received taxane-based therapy, 3 patients received oxaliplatin-based therapy, 4 patients received irinotecan-based therapy, and 2 patients received 5-FU plus cyclophosphamide or cetuximab. Three additional patients also received mainly fluoropyrimidine-based subsequent therapy.
Median follow-up time was 7.8 months (range 0.7–35.9 months). Median progression-free survival and overall survival were 5.6 months (95 % CI 4.1–6.3 months) and 8.0 months (95 % CI 6.3–10.1 months), respectively. The Kaplan–Meier estimated progression-free survival and overall survival curves are shown in Figs. 1 and 2, respectively. Overall survival at 1 year was 26.9 % and at 2 years was 13.4 %.
Safety
A total of 391 (median 7.5, range 1–29) cycles of chemotherapy were given. The median relative dose intensity was 88.5 % (range 51.4–103.2 %) for capecitabine and 99.3 % (range 43.6–103.9 %) for oxaliplatin. In total, 82.6 % of the patients received more than 80 % of the intended dose of capecitabine, and 95.7 % received more than 80 % of the intended dose of oxaliplatin.
All patients were evaluated for toxicities (Table 3). The most common hematological toxicity was thrombocytopenia (33 %), but without grade 3 or 4 events. Grade 3 leucopenia was observed in 2 % of the patients. Grade 3–4 anemia developed in five patients (11 %). The most common non-hematological toxicities were neuropathy (35 %), fatigue (31 %), diarrhea (26 %), vomiting (26 %), and hand-foot syndrome (22 %). Major grade 3 toxicities were diarrhea (9 %) and hand-foot syndrome (7 %). Treatment was delayed in 82 cycles (21 %), and dose modifications were implemented in 13 cycles (3 %). The most frequent cause of treatment delays was thrombocytopenia (31/82; 38 %), and the major reason for dose modification was hand-foot syndrome (6/13; 46 %). There were no treatment-related deaths.
Discussion
A combination chemotherapy regimen of 5-FU plus cisplatin has been widely used for the treatment of advanced gastric cancer patients [4–8]. However, this regimen is inconvenient, cumbersome, and associated with the risk of infection and thrombosis due to the continuous 5-FU infusion. In addition, cisplatin has a poor tolerability, due mostly to its renal toxicity.
Triweekly oxaliplatin plus oral capecitabine has been used for treating advanced gastric cancer, with response rates of 42–63 % and overall survival of 10.0–11.9 months [20–24]. In the treatment of metastatic colorectal cancer, biweekly oxaliplatin plus oral capecitabine has been shown to be as active as oxaliplatin plus intravenous 5-FU/leucovorin, with similar quality of life for patients [26]. However, the efficacy and toxicities of biweekly oxaliplatin plus oral capecitabine in treating advanced gastric cancer have not been investigated so far. This is the first phase II trial of using biweekly oxaliplatin plus oral capecitabine in advanced gastric cancer.
In a multicenter open-label phase II study, oral capecitabine has been shown to be an active and well-tolerated treatment in gastric cancer patients [13]. In a phase III trial of capecitabine in advanced gastric cancer, it has shown a non-inferior effect and similar safety profile to 5-FU [15]. In two published phase III studies, oxaliplatin was non-inferior to cisplatin and resulted in reduced toxicity compared with cisplatin in the treatment of esophagogastric cancer patients [18, 19]. Based on these published articles, capecitabine and oxaliplatin are considered as effective as 5-FU and cisplatin, respectively. In addition, administration of capecitabine is more convenient for patients than infusion of 5-FU, whereas oxaliplatin is more tolerable than cisplatin. Therefore, capecitabine and oxaliplatin are able to replace 5-FU and cisplatin, respectively.
The aim of this phase II study was to demonstrate the efficacy and safety of biweekly capecitabine in combination with oxaliplatin in previously untreated patients with locally advanced or metastatic gastric cancer. In our study, the overall response rate of ITT patients was 20 %. Median progression-free survival was 5.6 months, and median overall survival was 8.0 months. Although this biweekly XELOX study failed to meet its primary response rate endpoint, it still showed modest efficacy in the treatment of advanced gastric cancer.
An important conclusion from our phase II multicenter study was that the biweekly combination regimen of capecitabine and oxaliplatin had a good safety profile. Only 2 patients withdrew from the study because of treatment-related toxicities, and there were no treatment-related deaths. Grade 3 and 4 hematological and non-hematological adverse events were infrequent, and all toxicities were generally of mild to moderate intensity. The most common adverse events were thrombocytopenia (33 %), neuropathy (35 %), leucopenia (35 %), neutropenia (31 %), fatigue (31 %), diarrhea (26 %), vomiting (26 %), anemia (24 %), and hand-foot syndrome (22 %). The safety profile reported in our trial compared favorably with other phase II clinical studies with triweekly combination regimens of capecitabine/oxaliplatin [20–24]. Neuropathy, the major distressing toxicity of oxaliplatin, occurred in 35 % of our patients, which is relatively low compared to percentages reported in other studies (22–70 %) [20–24]. Hand-foot syndrome was also infrequent relative to other triweekly capecitabine/oxaliplatin studies (22 vs. 20–39 %) [20–24]. Neutropenia also occurred in a lower percentage of patients in this study than in other reports (31 vs. 35–56 %) [20–24].
In conclusion, the combination of biweekly capecitabine and oxaliplatin shows modest activity and an acceptable safety profile. The therapeutic index of the current regimen, which can be helpful to advanced gastric cancer patients, should be further explored.
References
Crew KD, Neugut AI (2006) Epidemiology of gastric cancer. World J Gastroenterol 12(3):354–362
Chiang CY, Huang KH, Fang WL, Wu CW, Chen JH, Lo SS, Hsieh MC, Shen KH, Li AF, Niu DM, Chiou SH (2011) Factors associated with recurrence within 2 years after curative surgery for gastric adenocarcinoma. World J Surg 35(11):2472–2478
Benson AB (2008) Advanced gastric cancer: an update and future directions. Gastrointest Cancer Res 2(4 Suppl):S47–S53
Ychou M, Astre C, Rouanet P, Fabre JM, Saint-Aubert B, Domergue J, Ribard D, Ciurana AJ, Janbon C, Pujol H (1996) A phase II study of 5-fluorouracil, leucovorin and cisplatin (FLP) for metastatic gastric cancer. Eur J Cancer 32A(11):1933–1937
Lin YC, Chen JS, Wang CH, Wang HM, Chang HK, Liaul CT, Yang TS, Liaw CC, Liu HE (2001) Weekly high-dose 5-fluorouracil (5-FU), leucovorin (LV) and bimonthly cisplatin in patients with advanced gastric cancer. Jpn J Clin Oncol 31(12):605–609
Ohtsu A, Shimada Y, Shirao K, Boku N, Hyodo I, Saito H, Yamamichi N, Miyata Y, Ikeda N, Yamamoto S, Fukuda H, Yoshida S, Japan Clinical Oncology Group Study (JCOG9205) (2003) Randomized phase III trial of fluorouracil alone versus fluorouracil plus cisplatin versus uracil and tegafur plus mitomycin in patients with unresectable, advanced gastric cancer: the Japan Clinical Oncology Group Study (JCOG9205). J Clin Oncol 21(1):54–59
Vanhoefer U, Rougier P, Wilke H, Ducreux MP, Lacave AJ, Van Cutsem E, Planker M, Santos JG, Piedbois P, Paillot B, Bodenstein H, Schmoll HJ, Bleiberg H, Nordlinger B, Couvreur ML, Baron B, Wils JA (2000) Final results of a randomized phase III trial of sequential high-dose methotrexate, fluorouracil, and doxorubicin versus etoposide, leucovorin, and fluorouracil versus infusional fluorouracil and cisplatin in advanced gastric cancer: a trial of the European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. J Clin Oncol 18(14):2648–2657
Kim NK, Park YS, Heo DS, Suh C, Kim SY, Park KC, Kang YK, Shin DB, Kim HT, Kim HJ et al (1993) A phase III randomized study of 5-fluorouracil and cisplatin versus 5-fluorouracil, doxorubicin, and mitomycin C versus 5-fluorouracil alone in the treatment of advanced gastric cancer. Cancer 71(12):3813–3818
Budman DR, Meropol NJ, Reigner B, Creaven PJ, Lichtman SM, Berghorn E, Behr J, Gordon RJ, Osterwalder B, Griffin T (1998) Preliminary studies of a novel oral fluoropyrimidine carbamate: capecitabine. J Clin Oncol 16(5):1795–1802
Ishitsuka H (2000) Capecitabine: preclinical pharmacology studies. Invest New Drugs 18(4):343–354
Koizumi W, Saigenji K, Ujiie S, Terashima M, Sakata Y, Taguchi T, Clinical Study Group of Capecitabine (2003) A pilot phase II study of capecitabine in advanced or recurrent gastric cancer. Oncology 64(3):232–236
Sakamoto J, Chin K, Kondo K, Kojima H, Terashima M, Yamamura Y, Tsujinaka T, Hyodo I, Koizumi W, Clinical Study Group of Capecitabine (2006) Phase II study of a 4-week capecitabine regimen in advanced or recurrent gastric cancer. Anticancer Drugs 17(2):231–236
Hong YS, Song SY, Lee SI, Chung HC, Choi SH, Noh SH, Park JN, Han JY, Kang JH, Lee KS, Cho JY (2004) A phase II trial of capecitabine in previously untreated patients with advanced and/or metastatic gastric cancer. Ann Oncol 15(9):1344–1347
Kim TW, Kang YK, Ahn JH, Chang HM, Yook JH, Oh ST, Kim BS, Lee JS (2002) Phase II study of capecitabine plus cisplatin as first-line chemotherapy in advanced gastric cancer. Ann Oncol 13(12):1893–1898
Kang YK, Kang WK, Shin DB, Chen J, Xiong J, Wang J, Lichinitser M, Guan Z, Khasanov R, Zheng L, Philco-Salas M, Suarez T, Santamaria J, Forster G, McCloud PI (2009) Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III noninferiority trial. Ann Oncol 20(4):666–673
Woynarowski JM, Faivre S, Herzig MC, Arnett B, Chapman WG, Trevino AV, Raymond E, Chaney SG, Vaisman A, Varchenko M, Juniewicz PE (2000) Oxaliplatin-induced damage of cellular DNA. Mol Pharmacol 58(5):920–927
Extra JM, Espie M, Calvo F, Ferme C, Mignot L, Marty M (1990) Phase I study of oxaliplatin in patients with advanced cancer. Cancer Chemother Pharmacol 25(4):299–303
Al-Batran SE, Hartmann JT, Probst S, Schmalenberg H, Hollerbach S, Hofheinz R, Rethwisch V, Seipelt G, Homann N, Wilhelm G, Schuch G, Stoehlmacher J, Derigs HG, Hegewisch-Becker S, Grossmann J, Pauligk C, Atmaca A, Bokemeyer C, Knuth A, Jäger E, Arbeitsgemeinschaft Internistische Onkologie (2008) Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol 26(9):1435–1442
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR, Upper Gastrointestinal Clinical Studies Group of the National Cancer Research Institute of the United Kingdom (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358(1):36–46
Park YH, Lee JL, Ryoo BY, Ryu MH, Yang SH, Kim BS, Shin DB, Chang HM, Kim TW, Yuh YJ, Kang YK (2008) Capecitabine in combination with Oxaliplatin (XELOX) as a first-line therapy for advanced gastric cancer. Cancer Chemother Pharmacol 61(4):623–629
Xiang XJ, Zhang L, Qiu F, Yu F, Zhan ZY, Feng M, Yan J, Zhao JG, Xiong JP (2012) A phase ii study of capecitabine plus oxaliplatin as first-line chemotherapy in elderly patients with advanced gastric cancer. Chemotherapy 58(1):1–7
Luo HY, Xu RH, Wang F, Qiu MZ, Li YH, Li FH, Zhou ZW, Chen XQ (2010) Phase II trial of XELOX as first-line treatment for patients with advanced gastric cancer. Chemotherapy 56(2):94–100
Yang T, Shen X, Tang X, Wei G, Zhang H, Du C, Xue X, Ma L, Nie M, Bi J (2011) Phase II trial of oxaliplatin plus oral capecitabine as first-line chemotherapy for patients with advanced gastric cancer. Tumori 97(4):466–472
Dong NN, Wang MY, Zhang Q, Liu ZF (2009) Oxaliplatin combined with capecitabine as first-line chemotherapy for patients with advanced gastric cancer. Aizheng 28(4):412–415 (article in Chinese)
Park YH, Kim BS, Ryoo BY, Yang SH (2006) A phase II study of capecitabine plus 3-weekly oxaliplatin as first-line therapy for patients with advanced gastric cancer. Br J Cancer 94(7):959–963
Comella P, Massidda B, Filippelli G, Farris A, Natale D, Barberis G, Maiorino L, Palmeri S, Cannone M, Condemi G, Southern Italy Cooperative Oncology Group (2009) Randomised trial comparing biweekly oxaliplatin plus oral capecitabine versus oxaliplatin plus i.v. bolus fluorouracil/leucovorin in metastatic colorectal cancer patients: results of the Southern Italy Cooperative Oncology study 0401. J Cancer Res Clin Oncol 135(2):217–226
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Acknowledgments
This work was supported by F. Hoffmann-La Roche Ltd. and grants from the Taipei Veterans General Hospital (V101C-178), the National Science Council (NSC 98-2314-B-075-029), and the National Research Program for Biopharmaceutics of Taiwan (100CT202).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov number: NCT00436241.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Chao, Y., Hsieh, JS., Yeh, HT. et al. A multicenter phase II study of biweekly capecitabine in combination with oxaliplatin as first-line chemotherapy in patients with locally advanced or metastatic gastric cancer. Cancer Chemother Pharmacol 73, 799–806 (2014). https://doi.org/10.1007/s00280-014-2407-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-014-2407-y