Abstract
Background
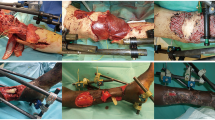
In a high conflict region, war injuries to the distal lower extremity are a major source of large composite defects involving bone and soft tissues. These defects are at the edge between using a single free flap [osteo-(+/-myo) cutaneous] vs double free flap reconstruction (bone and soft tissue). In this paper, we present our experience and outcomes in treating patients with leg war injury reconstructed using a single free fibula flap.
Methods
Fifteen patients with distal leg composite defects secondary to war injuries were treated between January 2015 and March 2016. All patients were reconstructed using single barrel free fibula osteo-(+/-myo)cutaneous flap where single or double skin paddles were used according to the soft tissue defect requiring coverage.
Results
There were no cases of total or partial flap loss. Complications were limited to three cases including traumatic fibula fracture, venous congestion with negative findings, and residual soft tissue defect requiring coverage. There were no cases of wound dehiscence or infection. Mean follow-up time was 418.8 days. Mean bone healing time was nine months after which patients were allowed full weight bearing.
Conclusion
A single barrel free fibula osteo-(+/-myo)cutaneous flap is a valid and reliable tool for reconstruction composite lower extremity defects post-war injury. Adequate planning of fibula flap soft tissue components (skin, muscle) rearrangement is essential for success in such challenging reconstructions.



Similar content being viewed by others
References
Holcomb JB, Stansbury LG, Champion HR, Wade C, Bellamy RF (2006) Understanding combat casualty care statistics. J Trauma 60(2):397–401. https://doi.org/10.1097/01.ta.0000203581.75241.f1
Dougherty AL, Mohrle CR, Galarneau MR, Woodruff SI, Dye JL, Quinn KH (2009) Battlefield extremity injuries in Operation Iraqi Freedom. Injury 40(7):772–777. https://doi.org/10.1016/j.injury.2009.02.014
Duramaz A, Bilgili MG, Bayram B, Ziroğlu N, Bayrak A, Avkan MC (2017) Orthopedic trauma surgery and hospital cost analysis in refugees; the effect of the Syrian civil War. Int Orthop 41(5):877–884. https://doi.org/10.1007/s00264-016-3378-x
Bosse MJ, Mackenzie EJ, Kellam JF et al (2002) An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med 347(24):1924–1931. https://doi.org/10.1056/nejmoa012604
Casey K, Sabino J, Jessie E, Martin BD, Valerio I (2015) Flap coverage outcomes following vascular injury and repair. Plast Reconstr Surg 135(1):301–308. https://doi.org/10.1097/prs.0000000000000769
Hernigou P, Pariat J (2017) History of internal fixation (part 1): early developments with wires and plates before World War II. Int Orthop 41(6):1273–1283. https://doi.org/10.1007/s00264-016-3347-4
Hernigou P, Pariat J (2017) History of internal fixation with plates (part 2): new developments after World War II; compressing plates and locked plates. Int Orthop 41(7):1489–1500. https://doi.org/10.1007/s00264-016-3379-9
Owens BD, Kragh JF Jr, Macaitis J, Svoboda SJ, Wenke JC (2007) Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma 21(4):254–257. https://doi.org/10.1097/BOT.0b013e31802f78fb
Murray CK, Hsu JR, Solomkin JS, Keeling JJ, Andersen RC, Ficke JR, Calhoun JH (2008) Prevention and management of infections associated with combat-related extremity injuries. J Trauma 64(Supplement). https://doi.org/10.1097/ta.0b013e318163cd14
Theodorakopoulou E, Mason KA, Pafitanis G, Ghanem AM, Myers S, Iwuagwu FC (2016) Free-tissue transfer for the reconstruction of war-related extremity injuries: a systematic review of current practice. Mil Med 181(1):27–34. https://doi.org/10.7205/milmed-d-15-00059
Tajsic NB, Husum H (2008) Reconstructive surgery including free flap transfers can be performed in low-resource settings: experiences from a wartime scenario. J Trauma 65(6):1463–1467. https://doi.org/10.1097/ta.0b013e318173f803
Grosset A, Pfister G, de l'Escalopier N, Plang S, Russo AP, Murison JC, Mathieu L, Rigal S. (2019) Risk factors and failures in the management of limb injuries in combat casualties. Int Orthop. https://doi.org/10.1007/s00264-019-04329-7
Fakhri RM, Herard P, Liswi MI, Boulart AL, Al Ani AMK (2019) Decision-making algorithm for sequential treatment of diaphyseal bone gaps in war-wounded patients in the Middle East. Int Orthop. https://doi.org/10.1007/s00264-019-04317-x
Pollak AN, Ficke JR, Injuries EW (2008) Extremity war injuries: challenges in definitive reconstruction. J Am Acad Orthop Surg 16(11):628–634. https://doi.org/10.5435/00124635-200811000-00003
Yaremchuk MJ, Brumback RJ, Manson PN, Burgess AR, Poka A, Weiland AJ (1987) Acute and definitive management of traumatic osteocutaneous defects of the lower extremity. Plast Reconstr Surg 80(1):13–14. https://doi.org/10.1097/00006534-198707000-00002
Taylor GI, Miller GD, Ham FJ (1975) The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg 55(5):533–544. https://doi.org/10.1097/00006534-197505000-00002
Tu Y, Yen C, Yeh W, Wang I, Wang K, Ueng SW (2001) Reconstruction of posttraumatic long bone defect with free vascularized bone graft: good outcome in 48 patients with 6 years follow-up. Acta Orthop 72(4):359–364. https://doi.org/10.1080/000164701753542014
Shpitzer T, Neligan P, Boyd B, Gullane P, Gur E, Freeman J (1997) Leg morbidity and function following fibular free flap harvest. Ann Plast Surg 38(5):460–464. https://doi.org/10.1097/00000637-199705000-00005
Maghari A, Forootan KS, Emami SA, Melow C (1992) Microvascular reconstruction of soft tissue and bone in war wounds. Scand J Plast Reconstr Surg Hand Surg 26(1):91–96. https://doi.org/10.3109/02844319209035189
Hariri A, Mascard E, Atlan F et al (2010) Free vascularised fibular graft for reconstruction of defects of the lower limb after resection of tumour. J Bone Joint Surg Br Vol 92-B(11):1574–1579. https://doi.org/10.1302/0301-620x.92b11.23832
Pollock R, Stalley P, Lee K, Pennington D (2005) Free vascularized fibula grafts in limb-salvage surgery. J Reconstr Microsurg 21(02):79–84. https://doi.org/10.1055/s-2005-864839
Fox CJ, Kreishman P (2010) High-energy trauma and damage control in the lower limb. Semin Plast Surg 24(1):5–10. https://doi.org/10.21236/ada554076
Mathieu L, Bertani A, Gaillard C, Chaudier P, Ollat D, Bauer B, Rigal S (2014) Combat-related upper extremity injuries: surgical management specificities on the theatres of operations. Chirurgie de la Main 33(3):174–182. https://doi.org/10.1016/j.main.2014.02.003
Kumar AR, Harshbarger R, Martin B (2010) Plastic surgery challenges in war wounded. Adv Wound Care 1:65–70. https://doi.org/10.1089/awc.2009.0087
Godina M (2006) Early microsurgical reconstruction of complex trauma of the extremities. Orthop Trauma Direct 4(5):29–35. https://doi.org/10.1055/s-2006-944324
Hérard P, Boillot F, Fakhri RM (2017) Bone cultures from war-wounded civilians in the Middle East: a surgical prospective. Int Orthop 41(7):1291–1294. https://doi.org/10.1007/s00264-016-3382-1
Kumar AR, Grewal NS, Chung TL, Bradley JP (2009) Lessons from the modern battlefield: successful upper extremity injury reconstruction in the subacute period. J Trauma 67(4):752–757. https://doi.org/10.1097/ta.0b013e3181808115
Kumar AR, Grewal NS, Chung TL, Bradley JP (2009) Lessons from Operation Iraqi Freedom: Successful Subacute Reconstruction of Complex Lower Extremity Battle Injuries. Plast Reconstr Surg 123(1):218–229. https://doi.org/10.1097/prs.0b013e3181904da9
Holmgaard R, Duffy J, Warburg FE, Jensen L, Bonde C (n.d.) Danish experience with free flaps in war wounds. Dan Med J 63(1):A5180
Sabino J, Polfer E, Tintle S et al (2015) A decade of conflict: flap coverage options and outcomes in traumatic war-related extremity reconstruction. Plast Reconstr Surg 135(3):895–902. https://doi.org/10.1097/prs.0000000000001025
Fleming ME, Watson TJ, Gaines RJ, O’Toole RV (2012) Evolution of orthopaedic reconstructive care. J Am Acad Orthop Surg 20. https://doi.org/10.5435/jaaos-20-08-s74
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures. J Trauma 24(8):742–746. https://doi.org/10.1097/00005373-198408000-00009
Lin C, Wei F, Chen H, Chuang DC (1999) Outcome comparison in traumatic lower-extremity reconstruction by using various composite vascularized bone transplantation. Plast Reconstr Surg 104(4):984–992. https://doi.org/10.1097/00006534-199909020-00013
Cutting CB, Mccarthy JG (1983) Comparison of residual osseous mass between vascularized and nonvascularized onlay bone transfers. Plast Reconstr Surg 72(5):672–675. https://doi.org/10.1097/00006534-198311000-00016
García-Cimbrelo E, Olsen B, Ruiz-Yagüe M, Fernandez-Baíllo N, Munuera-Martínez L (1992) Ilizarov technique. Results and difficulties. Clin Orthop Relat Res 283:116–123
Yazar S, Lin C, Wei F (2004) One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg:1457–1466. https://doi.org/10.1097/01.prs.0000138811.88807.65
Author information
Authors and Affiliations
Contributions
All authors significantly contributed to the drafting and revision of the manuscript and approve its final form.
Corresponding author
Ethics declarations
Ethical approval
The research was approved by the Institutional Review Board of the American University of Beirut Medical Center.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
This paper adheres to the STROBE guidelines.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Video 1
Raising the propeller flap from the fibula flap skin paddle based on the distal perforator then checking the pulse with doppler. (MP4 68720 kb)
Rights and permissions
About this article
Cite this article
Karami, R.A., Ghieh, F.M., Chalhoub, R.S. et al. Reconstruction of composite leg defects post-war injury. International Orthopaedics (SICOT) 43, 2681–2690 (2019). https://doi.org/10.1007/s00264-019-04423-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04423-w