Abstract
Purpose
Multiphasic CT or MRI and serum alpha-fetoprotein (AFP) are widely used for posttreatment surveillance of hepatocellular carcinoma (HCC). This study aimed to investigate the clinical outcomes of patients with high posttreatment AFP but without evident recurrence on CT or MRI after curative-intent treatment of HCC.
Methods
We retrospectively analyzed 121 patients presenting with high posttreatment AFP (> 20 ng/mL) without evident recurrence on multiphasic CT or MRI during surveillance after curative-intent surgical resection or radiofrequency ablation (RFA) for HCC. The time interval from the first event of high posttreatment AFP to imaging-evident recurrence (TimeAFP-Imaging recurrence) was estimated using the Kaplan–Meier method. Cox regression analyses were performed to assess the associated factors with TimeAFP-Imaging recurrence.
Results
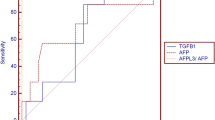
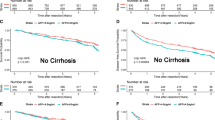
The median TimeAFP-Imaging recurrence was 20.0 months (95% CI 13.0–28.0 months), and the estimated 6-month and 1-year cumulative incidences of imaging-evident recurrence were 24.4% and 40.1%, respectively. In multivariate Cox analyses, late onset of AFP elevation (> 3 months after treatment) was an independent predictor of shorter TimeAFP-Imaging recurrence (HR 2.11, P = 0.015) if using variables available at the first event of AFP elevation, while non-normalization of AFP at the next follow-up was an independent predictor of shorter TimeAFP-Imaging recurrence (HR 3.65, P < 0.001) if using variables including the follow-up data.
Conclusion
In the surveillance setting after curative-intent treatment of HCC, patients presenting with high posttreatment AFP without evident recurrence on CT or MRI may frequently progress to imaging-evident recurrence. In high-risk patients, an extensive diagnostic workup or close monitoring is needed to detect HCC recurrence earlier.



Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- HCC:
-
Hepatocellular carcinoma
- IDR:
-
Intrahepatic distant recurrence
- LI-RADS:
-
Liver imaging reporting and data system
- LTP:
-
Local tumor progression
- RFA:
-
Radiofrequency ablation
- TimeAFP-Imaging recurrence :
-
Time interval from the first event of high posttreatment AFP to imaging-evident recurrence
References
Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, Gores G (2016) Hepatocellular carcinoma Nat Rev Dis Primers 2:16018. https://doi.org/10.1038/nrdp.2016.18
Pompili M, Saviano A, de Matthaeis N, Cucchetti A, Ardito F, Federico B, Brunello F, Pinna AD, Giorgio A, Giulini SM, De Sio I, Torzilli G, Fornari F, Capussotti L, Guglielmi A, Piscaglia F, Aldrighetti L, Caturelli E, Calise F, Nuzzo G, Rapaccini GL, Giuliante F (2013) Long-term effectiveness of resection and radiofrequency ablation for single hepatocellular carcinoma </=3 cm. Results of a multicenter Italian survey. J Hepatol 59 (1):89-97. https://doi.org/10.1016/j.jhep.2013.03.009
Lee DH, Lee JM, Lee JY, Kim SH, Yoon JH, Kim YJ, Han JK, Choi BI (2014) Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: long-term results and prognostic factors in 162 patients with cirrhosis. Radiology 270(3):900-909. https://doi.org/10.1148/radiol.13130940
Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, Taylor BR, Grant DR, Vollmer CM (2006) Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg 202(2):275-283. https://doi.org/10.1016/j.jamcollsurg.2005.10.005
European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L (2018) EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69(1):182-236. https://doi.org/10.1016/j.jhep.2018.03.019
Trevisani F, Garuti F, Neri A (2019) Alpha-fetoprotein for Diagnosis, Prognosis, and Transplant Selection. Semin Liver Dis 39(2):163-177. https://doi.org/10.1055/s-0039-1677768
NCCN Clinical Practice Guidelines in Oncology (NCCN guidelines), Hepatobiliary Cancers, version 5.2020. https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf
Kew M (1974) Alpha-fetoprotein in primary liver cancer and other diseases. Gut 15(10):814-821. https://doi.org/10.1136/gut.15.10.814
Silver HK, Gold P, Shuster J, Javitt NB, Freedman SO, Finlayson ND (1974) Alpha(1)-fetoprotein in chronic liver disease. N Engl J Med 291(10):506-508. https://doi.org/10.1056/NEJM197409052911006
Liu YR, Lin BB, Zeng DW, Zhu YY, Chen J, Zheng Q, Dong J, Jiang JJ (2014) Alpha-fetoprotein level as a biomarker of liver fibrosis status: a cross-sectional study of 619 consecutive patients with chronic hepatitis B. BMC Gastroenterol 14:145. https://doi.org/10.1186/1471-230X-14-145
He C, Peng W, Liu X, Li C, Li X, Wen TF (2019) Post-treatment alpha-fetoprotein response predicts prognosis of patients with hepatocellular carcinoma: A meta-analysis. Medicine (Baltimore) 98(31):e16557. https://doi.org/10.1097/MD.0000000000016557
Ezaki T, Yukaya H, Ogawa Y, Chang YC, Nagasue N (1988) Elevation of alpha-fetoprotein level without evidence of recurrence after hepatectomy for hepatocellular carcinoma. Cancer 61(9):1880-1883. https://doi.org/10.1002/1097-0142(19880501)61:9<1880:aid-cncr2820610926>3.0.co;2-s
American Colledge of Radiology (2018) Liver Imaging Reporting and Data System version 2018 Manual. https://www.acr.org/-/media/ACR/Files/Clinical-Resources/LIRADS/LI-RADS-2018-Manual-5Dec18.pdf?la=en.
Abdel Razek AAK, El-Serougy LG, Saleh GA, Abd El-Wahab R, Shabana W (2020) Interobserver Agreement of Magnetic Resonance Imaging of Liver Imaging Reporting and Data System Version 2018. J Comput Assist Tomogr 44(1):118-123. https://doi.org/10.1097/RCT.0000000000000945
Abdel Razek AAK, El-Serougy LG, Saleh GA, Shabana W, Abd El-Wahab R (2020) Liver Imaging Reporting and Data System Version 2018: What Radiologists Need to Know. J Comput Assist Tomogr 44(2):168-177. https://doi.org/10.1097/RCT.0000000000000995
Abdel Razek AAK, El-Serougy LG, Saleh GA, Shabana W, Abd El-Wahab R (2020) Reproducibility of LI-RADS treatment response algorithm for hepatocellular carcinoma after locoregional therapy. Diagn Interv Imaging. https://doi.org/10.1016/j.diii.2020.03.008
Chernyak V, Fowler KJ, Kamaya A, Kielar AZ, Elsayes KM, Bashir MR, Kono Y, Do RK, Mitchell DG, Singal AG, Tang A, Sirlin CB (2018) Liver Imaging Reporting and Data System (LI-RADS) Version 2018: Imaging of Hepatocellular Carcinoma in At-Risk Patients. Radiology 289(3):816-830. https://doi.org/10.1148/radiol.2018181494
Kielar A, Fowler KJ, Lewis S, Yaghmai V, Miller FH, Yarmohammadi H, Kim C, Chernyak V, Yokoo T, Meyer J, Newton I, Do RK (2018) Locoregional therapies for hepatocellular carcinoma and the new LI-RADS treatment response algorithm. Abdom Radiol (NY) 43(1):218-230. https://doi.org/10.1007/s00261-017-1281-6
Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, Chen MH, Choi BI, de Baere T, Dodd GD, 3rd, Dupuy DE, Gervais DA, Gianfelice D, Gillams AR, Lee FT, Jr., Leen E, Lencioni R, Littrup PJ, Livraghi T, Lu DS, McGahan JP, Meloni MF, Nikolic B, Pereira PL, Liang P, Rhim H, Rose SC, Salem R, Sofocleous CT, Solomon SB, Soulen MC, Tanaka M, Vogl TJ, Wood BJ, Goldberg SN, International Working Group on Image-guided Tumor A, Interventional Oncology Sans Frontieres Expert P, Technology Assessment Committee of the Society of Interventional R, Standard of Practice Committee of the C, Interventional Radiological Society of E (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria–a 10-year update. Radiology 273(1):241-260. https://doi.org/10.1148/radiol.14132958
Sharma S (2009) Tumor markers in clinical practice: General principles and guidelines. Indian J Med Paediatr Oncol 30(1):1-8. https://doi.org/10.4103/0971-5851.56328
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S (2015) Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg 261(5):947-955. https://doi.org/10.1097/SLA.0000000000000710
Gao J, Wang SH, Ding XM, Sun WB, Li XL, Xin ZH, Ning CM, Guo SG (2015) Radiofrequency ablation for single hepatocellular carcinoma 3 cm or less as first-line treatment. World J Gastroenterol 21(17):5287-5294. https://doi.org/10.3748/wjg.v21.i17.5287
Yagi R, Midorikawa Y, Moriguchi M, Nakayama H, Aramaki O, Yamazaki S, Higaki T, Takayama T (2018) Liver resection for recurrent hepatocellular carcinoma to improve survivability: a proposal of indication criteria. Surgery 163(6):1250-1256. https://doi.org/10.1016/j.surg.2017.12.022
Wattanasatesiri T, Kim HC, Choi JW, Lee JH, Joo I, Hur S, Lee M, Jae HJ, Chung JW (2019) Cone-Beam CT-Guided Chemoembolization in Patients with Complete Response after Previous Chemoembolization but Subsequent Elevated alpha-Fetoprotein without Overt Hepatocellular Carcinoma. J Vasc Interv Radiol 30(8):1273-1280. https://doi.org/10.1016/j.jvir.2019.03.020
Imai Y, Katayama K, Hori M, Yakushijin T, Fujimoto K, Itoh T, Igura T, Sakakibara M, Takamura M, Tsurusaki M, Takahashi H, Nakanishi K, Usuki N, Tsuji K, Ohashi H, Kim T, Takehara T, Murakami T (2017) Prospective Comparison of Gd-EOB-DTPA-Enhanced MRI with Dynamic CT for Detecting Recurrence of HCC after Radiofrequency Ablation. Liver Cancer 6(4):349-359. https://doi.org/10.1159/000481416
Kim KA, Kim MJ, Choi JY, Park MS, Lim JS, Chung YE, Kim KW (2014) Detection of recurrent hepatocellular carcinoma on post-operative surveillance: comparison of MDCT and gadoxetic acid-enhanced MRI. Abdom Imaging 39(2):291-299. https://doi.org/10.1007/s00261-013-0064-y
Shi JH, Line PD (2014) Effect of liver regeneration on malignant hepatic tumors. World J Gastroenterol 20(43):16167-16177. https://doi.org/10.3748/wjg.v20.i43.16167
Siripongsakun S, Wei SH, Lin S, Chen J, Raman SS, Sayre J, Tong MJ, Lu DS (2014) Evaluation of alpha-fetoprotein in detecting hepatocellular carcinoma recurrence after radiofrequency ablation. J Gastroenterol Hepatol 29(1):157-164. https://doi.org/10.1111/jgh.12438
Yang JD, Dai J, Singal AG, Gopal P, Addissie BD, Nguyen MH, Befeler AS, Reddy KR, Schwartz M, Harnois DM, Yamada H, Gores GJ, Feng Z, Marrero JA, Roberts LR (2017) Improved Performance of Serum Alpha-Fetoprotein for Hepatocellular Carcinoma Diagnosis in HCV Cirrhosis with Normal Alanine Transaminase. Cancer Epidemiol Biomarkers Prev 26(7):1085-1092. https://doi.org/10.1158/1055-9965.EPI-16-0747
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
This retrospective study was approved by our institutional review board and the requirement for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, J., Joo, I., Lee, D.H. et al. Clinical outcomes of patients with a high alpha-fetoprotein level but without evident recurrence on CT or MRI in surveillance after curative-intent treatment for hepatocellular carcinoma. Abdom Radiol 46, 597–606 (2021). https://doi.org/10.1007/s00261-020-02707-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02707-z