Abstract
Purpose
To assess the impacts of erythromycin on the pharmacokinetics of voriconazole and its association with CYP2C19 genotypes in healthy Chinese male subjects.
Methods
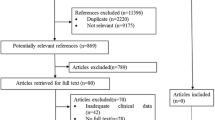
A single-center, open, crossover clinical study with two treatment phases was carried out. Eighteen healthy male volunteers, including 6 CYP2C19 homozygous extensive metabolizers (EMs, *1/*1), 6 heterozygous EMs (HEMs, *1/*2 or *1/*3), and 6 CYP2C19 poor metabolizers (PMs, *2/*2 or *2/*3), were enrolled in this study. A single oral dose of 200 mg voriconazole was administrated to all subjects after 3-day pretreatment with either 500 mg erythromycin or placebo three times daily. Periods were separated by a washout period of 14 days. Serial venous blood samples were collected, and plasma concentrations of voriconazole were determined by HPLC.
Results
Cmax, AUC0–24, and \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) of voriconazole were increased significantly, while oral clearance of voriconazole was decreased significantly by erythromycin administration (p < 0.001, respectively). Compared with individuals with CYP2C19 PM genotypes, individuals with CYP2C19 EM and HEM genotypes showed significantly decreased T½, AUC0–24, \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \), and increased oral clearance of voriconazole (p < 0.05, respectively). In addition, significant increases in AUC0–24 and \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) and decreases in oral clearance of voriconazole after erythromycin treatment were observed in CYP2C19 HEMs and PMs (p < 0.05, respectively), but not in CYP2C19 EMs.
Conclusion
Both CYP2C19 genotypes and CYP3A4 inhibitor erythromycin can influence the plasma concentration of voriconazole, and erythromycin increases plasma concentration of voriconazole in a CYP2C19 genotype-dependent manner.
Similar content being viewed by others
Introduction
Voriconazole is a second-generation triazole antifungal agent that is structurally related to fluconazole. The mechanism of action of voriconazole is similar to that of other azoles, i.e., it inhibits the cytochrome P450-dependent 14-α-lanosterol demethylase and disrupts fungal ergosterol synthesis [1–4]. Voriconazole is used for the treatment of invasive aspergillosis and other serious infections [5–8].
Voriconazole undergoes extensive oxidative metabolism mediated by cytochrome P450 (CYP) isoforms CYP2C19 and CYP3A4, and to a lesser extent, by CYP2C9 [9, 10]. Mutations in the CYP2C19 gene that result in the CYP2C19 poor metabolism (PM) phenotype are common in Asians. About 13–23% of Asians inherit CYP2C19 PM genotypes, which is a much higher prevalence than 3–5% observed in Caucasians [11–14]. Evidence has shown that 49% of the variance in apparent oral clearance of voriconazole can be explained solely by CYP2C19 polymorphisms [15]. It is suggested that the initiation dose of voriconazole dosage should be adjusted according to CYP2C19 genotypes to avoid hepatotoxicity [16]. Preliminary observations also suggest that CYP2C19 genotypes should be evaluated as a factor that may affect the pharmacokinetics of voriconazole and perhaps drug interactions or adverse events related to voriconazole [17–19].
CYP3A4 is a major drug metabolic enzyme in adult humans, and contributes to the metabolism of about 70% clinically important medications [20]. Induction or inhibition of CYP3A4 as a result of drug interactions is common in clinical practice. During the treatment of systemic fungal infection, antifungal agents such as voriconazole are often prescribed concomitantly with other medicines, and some of these latter medicines are CYP3A4 inhibitors [21]. Erythromycin has proven to be a potent CYP3A4 inhibitor that can result in mechanism-based inactivation of CYP3A4 [22–24]. Results from in vitro study indicate that erythromycin affects voriconazole metabolism [10], although the clinic relevance of this drug interaction remains to be explored.
This study was designed to assess the impacts of erythromycin on pharmacokinetics of voriconazole, and to identify the potential role of CYP2C19 variants in the magnitude of this drug–drug interaction in healthy Chinese male subjects. We expect that the results of this study would be helpful in the optimization of voriconazole therapy in the clinic.
Materials and methods
Subjects
Two hundred and ninety-seven unrelated Chinese male healthy volunteers were genotyped for CYP2C19*2 and CYP2C19*3 variations. Six individuals homozygous for the wild-type allele (CYP2C19*1/*1, denoted EM), 6 individuals heterozygous for the CYP2C9*2 or CYP2C9*3 variants (n = 4 for the CYP2C9*1/*2 genotype and n = 2 for the CYP2C9*1/*3 genotype, denoted HEM) , and 6 individuals carrying two variant alleles simultaneously (n = 5 for the CYP2C19*2/*2 genotype and n = 1 for the CYP2C19*2/*3 genotype, denoted PM) were then selected randomly from these subjects. The mean age of the volunteers ranged from 19 to 23 years and the range of body mass index was approximately 18–25 kg/m2. No significant difference in either mean age or body mass index was observed among the three genotyped groups.
All subjects were ascertained to be in good health as identified from medical history, routine physical examination, and clinical laboratory tests. None of the volunteers was a smoker or had received any medication of botanical dietary supplements at least 2 weeks before entry into and during the study. All subjects ate a normal diet during the study. The study protocol was approved by the Ethics committee of Xiangya School of Medicine, Central South University. Written informed consent was obtained from all volunteers.
Study design
The study was carried out as a single-center, randomized, open, crossover design with two treatment phases, separated by a 2-week washout period. The subjects were hospitalized during the investigational treatments (from day 1 to the morning in day 5) in each phase. In each phase, the 18 volunteers received oral administration of either placebo or erythromycin (4 tablets erythromycin enteric-coated 125 mg; Baiyunshan, Guangzhou, China; batch No.1060001) three times daily for 4 days (day 1 to day 4) for 12 doses (the tenth dose being administered 30 min ahead of the voriconazole dose on the morning of day 4). On day 4, each subject was given a single oral dose of 200 mg voriconazole (four tablets of voriconazole 50 mg; GeneTech Pharm, Beijing, China; batch No. 20051001, this dose level is recommended in clinical use) along with 200 mL plain water after overnight fasting and rest. The subjects were asked to be recumbent from 30 min before to 4 h after the administration of drugs. Standardized meals were served at 2 h, 4 h, and 10 h respectively, after morning drug dosing. All subjects were under close surveillance by appropriately qualified staff within 24 h after voriconazole administration.
Venous blood samples for the determination of plasma concentrations of voriconazole were collected immediately before and at 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, and 24 h after the administration of voriconazole. Blood was collected into 4-mL EDTA-containing vacuum blood-collecting tubes. Immediately after blood collection, the samples were centrifuged at 3,000 rpm for 10 min. The plasma was transferred into polypropylene tubes and stored at −40°C until analysis.
CYP2C19 genotyping
Genomic deoxyribonucleic acid (DNA) samples were extracted from venous blood samples by standard phenol/chloroform extraction. Detection of CYP2C19*2 and CYP2C19*3 mutant alleles was performed by PCR/RFLP, as described elsewhere [25–27]. PCR products were digested with the restriction endonucleases Sma I and BamH I to detect the CYP2C19*2 allele and the CYP2C19*3 allele respectively. DNA fragments generated after restriction enzyme digestion were separated on a 2% agarose gel. Restriction fragments were visualized by use of a UV detector.
High performance liquid chromatography determination of the plasma concentration of voriconazole
Plasma concentrations of voriconazole were determined by high performance liquid chromatography (HPLC) as described with optimization [28]. Plasma samples were extracted with chloroform. Chromatographic column was Diamonsil C18 (250 mm × 4.6 mm, 5 μm); the mobile phase was composed of acetonitrile: 10 mM ammonium acetate (pH set at 5.4 with acetic acid) with a v:v of 50:50; the flow rate was 1.0 mL/min; the column temperature was 40°C and the detector wavelength was set at 255 nm. The standard curves of voriconazole were constructed with eight non-zero standards ranging from 0.02 μg/mL to 8.86 μg/mL. The lower limit of quantification was 0.02 μg/mL and the concentrations of QC samples were 0.07, 1.10 and 8.80 μg/mL respectively.
Safety analysis
All adverse events reported spontaneously by the subjects or observed during the subjects’ surveillance were documented, including times of onset and resolution, intensity, and causal relationship to the study drug. Vital signs including blood pressure and pulse rate were surveyed regularly during the hospitalization period.
Pharmacokinetic analysis
The peak concentration (Cmax) and concentration peak time (tmax) were obtained directly from the observed data. The elimination half-life (t½), the area under the plasma concentration–time curve (AUC0–24), AUC from zero to infinity (0-∞) and the apparent oral clearance (CLoral/F) were calculated by DAS 2.0 (Gaosi Data Analysis, Wuhu, China).
Statistical analysis
Statistical analyses were carried out with SPSS software version 11.0 for Windows (SPSS, Chicago, IL, USA). Data were expressed as mean±SD. Differences in pharmacokinetic parameters and ratios in different treated phases within the same genotype and pharmacokinetic parameters among different genotypes were compared using t test or ANOVA respectively. Wilcoxon’s signed-rank test was used to compare difference in tmax between or among different groups. A p value <0.05 was considered to be statistically significant.
Results
Safety of voriconazole after oral administration
Voriconazole was generally well tolerated by all participants, without serious adverse events. One participant with the CYP2C19*2/*2 genotype discontinued the study after the first phase because of a heavy cold.
Erythromycin increased the plasma concentration of voriconazole
Figure 1 showed the plasma concentration–time curves of voriconazole with a 4-day treatment with erythromycin and placebo. Compared with the placebo-treated phase, the Cmax (2.36 ± 0.78 μg/mL vs 3.16 ± 0.76 μg/mL, p < 0.001), AUC0–24 (12.65 ± 10.15 μg·h/mL vs 18.97 ± 13.86 μg·h/mL, p < 0.001), \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) (15.62 ± 15.11 μg·h/mL vs 23.63 ± 20.45 μg·h/mL, p < 0.001) of voriconazole was increased significantly in the erythromycin treated phase, while the CLoral/F of voriconazole was decreased significantly by 4-day erythromycin treatment (381 ± 244 mL/min vs 245 ± 171 mL/min, p < 0.001, Table 1). No significant difference in T½ and Tmax was observed between the placebo- and erythromycin-treated phases (Table 1).
CYP2C19 PM genotype increased the plasma concentration of voriconazole in the placebo-treated phase
Plasma concentration–time curves of voriconazole according to CYP2C19 genotypes in the placebo-treated phase are shown in Fig. 2. Significant differences in T½, AUC0–24, \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \), and oral clearance of voriconazole were observed among CYP2C19 genotypes (p < 0.05, Table 1). Compared with individuals with CYP2C19 PM genotypes, individuals with EM and HEM genotypes showed significantly decreased T½, AUC0–24, \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \), and increased oral clearance of voriconazole (p < 0.05 respectively, Table 1). No significant difference in any of the pharmacokinetics parameters of voriconazole between EM and HEM genotypes was observed in the placebo-treated phase (Table 1).
Effect of erythromycin on voriconazole pharmacokinetics is associated with CYP2C19 genotypes
We then analyzed the effect of erythromycin on the pharmacokinetics of voriconazole according to CYP2C19 genotypes. The pharmacokinetics profile and detailed pharmacokinetic parameters are shown in Fig. 3 and Table 1 respectively. Both AUC0–24 (p < 0.05 for PM, and p < 0.01 for HEM) and \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) (p < 0.01 for both PM and HEM) was increased significantly after erythromycin treatment in CYP2C19 HEM and PM individuals, but not in CYP2C19 EM individuals. CLoral/F of voriconazole was decreased obviously after erythromycin treatment in the CYP2C19 HEM and PM individuals (p < 0.05 for PM, and p < 0.01 for HEM), but not in the CYP2C19 EM individuals. However, the Cmax of voriconazole was increased significantly in individuals with the CYP2C19 EM (p < 0.01) and HEM (p < 0.05) individuals, but not PM individuals after erythromycin treatment. No significant difference in T½ and Tmax of voriconazole was observed between placebo- and erythromycin-treated phases for any of the CYP2C19 genotypes.
Discussion
In the consideration that the antifungal agent voriconazole might be used concomitantly with the erythromycin, a potent CYP3A4 inhibitor, we observed the effect of 4-day erythromycin administration on the pharmacokinetics of voriconazole, and assessed the association of CYP2C19 variants (CYP2C19*2 and CYP2C19*3) with this drug–drug interaction in healthy Chinese male subjects. We observed that both 4-day treatment with erythromycin and CYP2C19 PM genotypes increased the plasma concentration of voriconazole and decreased its oral clearance. We also observed a significant erythromycin–CYP2C19 genotype interaction influencing plasma concentration of voriconazole in these individuals, and erythromycin treatment increased the AUC and decreased oral clearance of voriconazole limited to CYP2C19 HEM and PM, but not CYP2C19 EM individuals.
Our observation that T½, Cmax, AUC0–24, \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) was increased and CLoral/F was decreased in CYP2C19 PMs compared with CYP2C19 EMs in the placebo-treated phase is in agreement with several previous studies [18, 19, 29, 30], which indicates that CYP2C19 genotypes are a key factor in the determination of voriconazole metabolism.
In vitro study indicates that the Michaelis–Menten constant (Km) of voriconazole oxidase activity by CYP2C19 was obviously lower than that by CYP3A4. Therefore, CYP3A4-mediated metabolism may not be the main pathway of voriconazole elimination [9, 10]. Previous in vivo and in vitro studies have also investigated the effect of CYP3A4 inhibitors on metabolism of voriconazole [10, 29]. However, controversial observations are reported [10, 29]. A study by Purkins et al. suggests that erythromycin does not affect the steady-state pharmacokinetics of voriconazole [29]. However, the study design of ours is very different from that of Purkins et al. In their study, voriconazole was given 200 mg twice daily for 14 days, while erythromycin was given twice daily during day 8 to day 14 after initiation of voriconazole administration, and pharmacokinetics of voriconazole was analyzed on days 7 and 14 [29]. However, it is reported that voriconazole can also inhibit CYP3A4 [9, 10] and thus may inhibit its own metabolism after long-term use, while in our study, erythromycin was administered for 3 days before a single oral dose of voriconazole. Our results suggest that erythromycin can obviously affect the pharmacokinetics of voriconazole. As both erythromycin and voriconazole can inhibit CYP3A4, the interactions between erythromycin and voriconazole are more complicated in vivo, if voriconazole has reached its steady-state after repeated doses, the effects of CYP3A4 inhibitors may not change voriconazole metabolism. However, if CYP3A4 inhibitors are given before voriconazole, voriconazole metabolism will be affected. Further research is needed to study the effects of CYP3A4 inhibitors on the pharmacokinetics of voriconazole.
Because CYP2C19 is a major enzyme involved in voriconazole metabolism [9, 10], and CYP2C19 genetic polymorphism can also affect the pharmacokinetics of voriconazole, we hypothesize in our study that the CYP2C19 genetic polymorphism might interact with erythromycin in affecting voriconazole metabolism. We observed that the increases in \( {\hbox{AU}}{{\hbox{C}}_{0 - \infty }} \) and decreases in CLoral/F of voriconazole by erythromycin pretreatment were significantly different among CYP2C19 genotypes. In both the CYP2C19 HEM and PM individuals, AUC of voriconazole increased significantly while oral clearance of voriconazole decreased significantly after erythromycin treatment. However, in individuals with the CYP2C19 EM genotypes, the changes in AUC and oral clearance of voriconazole were not obvious after erythromycin treatment. These findings indicate a drug–gene interaction in the inhibition of voriconazole metabolism by erythromycin, and CYP3A4 might be important for voriconazole metabolism in CYP2C19 HEM and PM individuals.
Because CYP2C19 genetic analysis for this study included only alleles *2 and *3, the two major mutant alleles of CYP2C19, comprising almost 100% of the PMs in oriental populations [12, 26], the occurrence of other defective alleles in the study population and thus misclassification of individuals cannot be ruled out.
In conclusion, this study provides further evidence for the determination of CYP2C19 genotypes in voriconazole metabolism, and find that pretreatment with the CYP3A4 inhibitor erythromycin can increase the plasma concentration of voriconazole in a CYP2C19 genotype-dependent manner. Therefore, combination therapy with erythromycin or other CYP3A4 inhibitors and voriconazole may result in higher antifungal exposure, especially in CYP2C19 PM and HEM individuals. At the same time, attention should be paid to dose-limiting adverse events of voriconazole, such as hepatotoxicity, when CYP2C19 PM and HEM patients undergo concomitant voriconazole and erythromycin therapy. Considering the results of our study and previous findings, we would suggest that the voriconazole dosage might be reduced for CYP2C19 PM and HEM individuals, as lower doses in PM and HEM can meet the required effective therapeutic level and decrease the adverse events of voriconazole.
References
Sheehan DJ, Hitchcock CA, Sibley CM (1999) Current and emerging azole antifungal agents. Clin Microbiol Rev 12(1):40–79
Chandrasekar PH, Manavathu E (2001) Voriconazole: a second-generation triazole. Drugs Today (Barc) 37(2):135–148
Ghannoum MA, Kuhn DM (2002) Voriconazole—better chances for patients with invasive mycoses. Eur J Med Res 7(5):242–256
Hoffman HL, Rathbun RC (2002) Review of the safety and efficacy of voriconazole. Expert Opin Investig Drugs 11(3):409–429
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW et al (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347(6):408–415
Perfect JR, Marr KA, Walsh TJ, Greenberg RN, DuPont B, de la Torre-Cisneros J et al (2003) Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin Infect Dis 36(9):1122–1131
Pfaller MA, Diekema DJ, Rex JH, Espinel-Ingroff A, Johnson EM, Andes D et al (2006) Correlation of MIC with outcome for Candida species tested against voriconazole: analysis and proposal for interpretive breakpoints. J Clin Microbiol 44(3):819–826
Theuretzbacher U, Ihle F, Derendorf H (2006) Pharmacokinetic/pharmacodynamic profile of voriconazole. Clin Pharmacokinet 45(7):649–663
Hyland R, Jones BC, Smith DA (2003) Identification of the cytochrome P450 enzymes involved in the N-oxidation of voriconazole. Drug Metab Dispos 31(5):540–547
Murayama N, Imai N, Nakane T, Shimizu M, Yamazaki H (2007) Roles of CYP3A4 and CYP2C19 in methyl hydroxylated and N-oxidized metabolite formation from voriconazole, a new anti-fungal agent, in human liver microsomes. Biochem Pharmacol 73(12):2020–2026
Wilkinson GR, Guengerich FP, Branch RA (1989) Genetic polymorphism of S-mephenytoin hydroxylation. Pharmacol Ther 43(1):53–76
Xiao ZS, Goldstein JA, Xie HG, Blaisdell J, Wang W, Jiang CH et al (1997) Differences in the incidence of the CYP2C19 polymorphism affecting the S-mephenytoin phenotype in Chinese Han and Bai populations and identification of a new rare CYP2C19 mutant allele. J Pharmacol Exp Ther 281(1):604–609
Qin XP, Xie HG, Wang W, He N, Huang SL, Xu ZH et al (1999) Effect of the gene dosage of CgammaP2C19 on diazepam metabolism in Chinese subjects. Clin Pharmacol Ther 66(6):642–646
Zhou HH (2001) CYP2C19 genotype determines enzyme activity and inducibility of S-mephenytoin hydroxylase. Clin Chim Acta 313(1–2):203–208
Weiss J, Ten Hoevel MM, Burhenne J, Walter-Sack I, Hoffmann MM, Rengelshausen J, Haefeli WE, Mikus G (2009) CYP2C19 genotype is a major factor contributing to the highly variable pharmacokinetics of voriconazole. J Clin Pharmacol 49(2):196–204
Matsumoto K, Ikawa K, Abematsu K, Fukunaga N, Nishida K, Fukamizu T, Shimodozono Y, Morikawa N, Takeda Y, Yamada K (2009) Correlation between voriconazole trough plasma concentration and hepatotoxicity in patients with different CYP2C19 genotypes. Int J Antimicrob Agents 34(1):91–94
Jeu L, Piacenti FJ, Lyakhovetskiy AG, Fung HB (2003) Voriconazole. Clin Ther 25(5):1321–1381
Ikeda Y, Umemura K, Kondo K, Sekiguchi K, Miyoshi S, Nakashima M (2004) Pharmacokinetics of voriconazole and cytochrome P450 2C19 genetic status. Clin Pharmacol Ther 75(6):587–588
Rengelshausen J, Banfield M, Riedel KD, Burhenne J, Weiss J, Thomsen T et al (2005) Opposite effects of short-term and long-term St John's wort intake on voriconazole pharmacokinetics. Clin Pharmacol Ther 78(1):25–33
Zhou S, Yung CS, Cher Goh B, Chan E, Duan W, Huang M et al (2005) Mechanism-based inhibition of cytochrome P450 3A4 by therapeutic drugs. Clin Pharmacokinet 44:279–304
Nierenberg NE, Thompson GR, Lewis JS, Hogan BK, Patterson TF (2010) Voriconazole use and pharmacokinetics in combination with interferon-gamma for refractory cryptococcal meningitis in a patient receiving low-dose ritonavir. Med Mycol 48(3):532–536
Periti P, Mazzei T, Mini E, Novelli A (1992) Pharmacokinetic drug interactions of macrolides. Clin Pharmacokinet 23(2):106–131
Von Rosensteil NA, Adam D (1995) Macrolide antibacterials. Drug interactions of clinical significance. Drug Saf 13(2):105–122
De Mey C, Althaus M, Ezan E, Retzow A (2001) Erythromycin increases plasma concentrations of alpha-dihydroergocryptine in humans. Clin Pharmacol Ther 70(2):142–148
De Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA (1994) The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem 269(22):15419–15422
De Morais SM, Goldstein JA, Xie HG, Huang SL, Lu YQ, Xia H et al (1995) Genetic analysis of the S-mephenytoin polymorphism in a Chinese population. Clin Pharmacol Ther 58(4):404–411
Edeki TI, Goldstein JA, de Morais SM, Hajiloo L, Butler M, Chapdelaine P, Wilkinson GR (1996) Genetic polymorphism of S-mephenytoin 4′-hydroxylation in African-Americans. Pharmacogenetics 6(4):357–360
Gage R, Stopher DA (1998) A rapid HPLC assay for voriconazole in human plasma. J Pharm Biomed Anal 17(8):1449–1453
Purkins L, Wood N, Ghahramani P, Kleinermans D, Layton G, Nichols D (2003) No clinically significant effect of erythromycin or azithromycin on the pharmacokinetics of voriconazole in healthy male volunteers. Br J Clin Pharmacol 56 [Suppl 1]:30–36
Mikus G, Schowel V, Drzewinska M, Rengelshausen J, Ding R, Riedel KD et al (2006) Potent cytochrome P450 2C19 genotype-related interaction between voriconazole and the cytochrome P450 3A4 inhibitor ritonavir. Clin Pharmacol Ther 80(2):126–135
Acknowledgement
This work was supported by National Science Foundation of China grants (C03050205). We are grateful for the excellent technical assistance of Lijun Yang for PCR-RELP and Dong Guo, Liang Peng for HPLC during the study. We are grateful to GeneTech Pharm in Beijing for providing voriconazole.
Conflict of interest
None of the authors has any financial or personal relationships to disclose that could potentially be perceived as influencing the described research.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Shi, HY., Yan, J., Zhu, WH. et al. Effects of erythromycin on voriconazole pharmacokinetics and association with CYP2C19 polymorphism. Eur J Clin Pharmacol 66, 1131–1136 (2010). https://doi.org/10.1007/s00228-010-0869-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0869-3