Abstract
Introduction
Postoperative delirium (POD) is a common complication in elderly surgical patients. Patients undergoing hip fractures surgery who are often characterized by advanced age could be particularly prone to suffering POD. We performed a meta-analysis to assess the association between POD and mortality in elderly patients undergoing hip fractures surgery.
Summary
This meta-analysis included twenty-one cohort studies, and the pooled outcomes demonstrated that approximated one-fourth of patients undergoing hipfracture surgery would develop POD, and delirium increased the mortality in these patients.
Methods
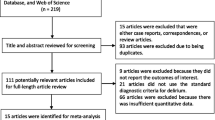
We searched PubMed, Embase, Web of Science, and Scopus for studies that investigated the effect of POD on mortality in elderly patients undergoing hip fracture surgery. Two reviewers independently selected studies, assessed quality, and extracted data. Statistical analyses were performed by STATA 14.0 and RevMan 5.3. Risk ratios (RRs) with 95% confidence intervals (CIs) were derived using random or fixed-effects model.
Results
Twenty-one cohort studies enrolling a total of 6288 patients were included, and the pooled prevalence (95% CI) of POD was 28% (23–34%). POD was associated with an increase in perioperative mortality (30-day or in-hospital mortality) [12 studies, 3123 patients, relative risk (RR) (95% CI) 2.79 (1.97–3.93)], 6-month mortality [6 studies, 1673 patients, 2.51 (1.99–3.16)], 1-year mortality [6 studies, 1896 patients, 1.98 (1.62–2.41)], and more than 1-year mortality [8 studies, 1926 patients, 2.06 (1.60–2.64)].
Conclusions
Our meta-analysis demonstrated that approximated one-fourth of patients undergoing hip fracture surgery would develop POD, and delirium increased the short-term and long-term mortality in these patients.




Similar content being viewed by others
Abbreviations
- POD:
-
Postoperative delirium
- RR:
-
Relative risk
- CI:
-
Confidence interval
References
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383(9920):911–922. https://doi.org/10.1016/s0140-6736(13)60688-1
Zenilman ME (2017) Delirium: an important postoperative complication. JAMA 317:77–78. https://doi.org/10.1001/jama.2016.18174
Zywiel MG, Hurley RT, Perruccio AV, Hancock-Howard RL, Coyte PC, Rampersaud YR (2015) Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. J Bone Joint Surg Am 97(10):829–836. https://doi.org/10.2106/jbjs.N.00724
Marcantonio ER, Flacker JM, Michaels M, Resnick NM (2000) Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 48(6):618–624
Hamilton GM, Wheeler K, Di Michele J, Lalu MM, McIsaac DI (2017) A systematic review and meta-analysis examining the impact of incident postoperative delirium on mortality. Anesthesiology 127(1):78–88. https://doi.org/10.1097/aln.0000000000001660
Salluh JI, Wang H, Schneider EB, Nagaraja N, Yenokyan G, Damluji A, Serafim RB, Stevens RD (2015) Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ 350:h2538. https://doi.org/10.1136/bmj.h2538
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
G. A. Wells, B. Shea, D. O'Connell et al. (2017) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses,” http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Schneck A (2017) Examining publication bias-a simulation-based evaluation of statistical tests on publication bias. PeerJ 5:e4115. https://doi.org/10.7717/peerj.4115
Olofsson B, Persson M, Bellelli G, Morandi A, Gustafson Y, Stenvall M (2018) Development of dementia in patients with femoral neck fracture who experience postoperative delirium-a three-year follow-up study. Int J Geriatr Psychiatry 33(4):623–632. https://doi.org/10.1002/gps.4832
Bellelli G, Carnevali L, Corsi M, Morandi A, Zambon A, Mazzola P, Galeazzi M, Bonfanti A, Massariello F, Szabo H, Oliveri G, Haas J, d'Oro LC, Annoni G (2018) The impact of psychomotor subtypes and duration of delirium on 6-month mortality in hip-fractured elderly patients. Int J Geriatr Psychiatry. https://doi.org/10.1002/gps.4914
Ruggiero C, Bonamassa L, Pelini L, Prioletta I, Cianferotti L, Metozzi A, Benvenuti E, Brandi G, Guazzini A, Santoro GC, Mecocci P, Black D, Brandi ML (2017) Early post-surgical cognitive dysfunction is a risk factor for mortality among hip fracture hospitalized older persons. Osteoporos Int 28(2):667–675. https://doi.org/10.1007/s00198-016-3784-3
Lee HB, Oldham MA, Sieber FE, Oh ES (2017) Impact of delirium after hip fracture surgery on one-year mortality in patients with or without dementia: a case of effect modification. Am J Geriatr Psychiatry 25(3):308–315. https://doi.org/10.1016/j.jagp.2016.10.008
Kim JY, Yoo JH, Kim E, Kwon KB, Han BR, Cho Y, Park JH (2017) Risk factors and clinical outcomes of delirium in osteoporotic hip fractures. J Orthop Surg 25(3):2309499017739485. https://doi.org/10.1177/2309499017739485
Radinovic K, Markovic-Denic L, Dubljanin-Raspopovic E, Marinkovic J, Milan Z, Bumbasirevic V (2015) Estimating the effect of incident delirium on short-term outcomes in aged hip fracture patients through propensity score analysis. Geriatr Gerontol Int 15(7):848–855. https://doi.org/10.1111/ggi.12358
González L, Puerta R, Fernández F, Lamas JL, Valle L, De La Fuente J (2013) What is the role of delirium in patients with hip fracture? Eur J Intern Med 24:e257–e258. https://doi.org/10.1016/j.ejim.2013.08.663
Lee KH, Ha YC, Lee YK, Kang H, Koo KH (2011) Frequency, risk factors, and prognosis of prolonged delirium in elderly patients after hip fracture surgery. Clin Orthop Relat Res 469(9):2612–2620. https://doi.org/10.1007/s11999-011-1806-1
Kat MG, de Jonghe JF, Vreeswijk R, van der Ploeg T, van Gool WA, Eikelenboom P, Kalisvaart KJ (2011) Mortality associated with delirium after hip-surgery: a 2-year follow-up study. Age Ageing 40(3):312–318. https://doi.org/10.1093/ageing/afr014
Juliebo V, Krogseth M, Skovlund E, Engedal K, Ranhoff AH, Wyller TB (2010) Delirium is not associated with mortality in elderly hip fracture patients. Dement Geriatr Cogn Disord 30(2):112–120. https://doi.org/10.1159/000318819
Bickel H, Gradinger R, Kochs E, Forstl H (2008) High risk of cognitive and functional decline after postoperative delirium. A three-year prospective study. Dement Geriatr Cogn Disord 26(1):26–31. https://doi.org/10.1159/000140804
Furlaneto ME, Garcez-Leme LE (2007) Impact of delirium on mortality and cognitive and functional performance among elderly people with femoral fractures. Clinics 62(5):545–552. https://doi.org/10.1590/S1807-59322007000500003
Zakriya K, Sieber FE, Christmas C, Wenz JF Sr, Franckowiak S (2004) Brief postoperative delirium in hip fracture patients affects functional outcome at three months. Anesth Analg 98(6):1798–1802 table of contents
Lundstrom M, Edlund A, Bucht G, Karlsson S, Gustafson Y (2003) Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc 51(7):1002–1006
Holmes J, House A (2000) Psychiatric illness predicts poor outcome after surgery for hip fracture: a prospective cohort study. Psychol Med 30(4):921–929. https://doi.org/10.1017/S0033291799002548
Edlund A, Lundstrom M, Lundstrom G, Hedqvist B, Gustafson Y (1999) Clinical profile of delirium in patients treated for femoral neck fractures. Dement Geriatr Cogn Disord 10(5):325–329. https://doi.org/10.1159/000017163
Brannstrom B, Gustafson Y, Norberg A, Winblad B (1989) Problems of basic nursing care in acutely confused and non-confused hip-fracture patients. Scand J Caring Sci 3(1):27–34
de Jong L, Vajim v R, Raats JW, Tmal K, Kuijper TM, Ret RG (2019) Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: risk factors and clinical outcomes. Clin Interv Aging 14:427–435. https://doi.org/10.2147/CIA.S189760
Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, van der Laan L (2017) Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging 12:421–430. https://doi.org/10.2147/cia.s115945
Luger MF, Müller S, Kammerlander C, Gosch M, Luger TJ (2014) Predictors of postoperative cognitive decline in very old patients with hip fracture: a retrospective analysis. Geriatr Orthop Surg Rehabil 5(4):165–172. https://doi.org/10.1177/2151458514548577
Wilson PT, Spitzer RL (1968) Major changes in psychiatric nomenclature. Reconciling existing psychiatric medical records with the new American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. Hosp Community Psychiatry 19(6):169–174
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113(12):941–948. https://doi.org/10.7326/0003-4819-113-12-941
Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304(4):443–451. https://doi.org/10.1001/jama.2010.1013
Yang Y, Zhao X, Dong T, Yang Z, Zhang Q, Zhang Y (2017) Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res 29(2):115–126. https://doi.org/10.1007/s40520-016-0541-6
Zhu Y, Wang G, Liu S, Zhou S, Lian Y, Zhang C, Yang W (2017) Risk factors for postoperative delirium in patients undergoing major head and neck cancer surgery: a meta-analysis. Jpn J Clin Oncol 47(6):505–511. https://doi.org/10.1093/jjco/hyx029
Watt J, Tricco AC, Talbot-Hamon C, Pham B, Rios P, Grudniewicz A, Wong C, Sinclair D, Straus SE (2018) Identifying older adults at risk of delirium following elective surgery: a systematic review and meta-analysis. J Gen Intern Med 33(4):500–509. https://doi.org/10.1007/s11606-017-4204-x
American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults (2015) J Am Geriatr Soc 63 (1):142-150. doi:https://doi.org/10.1111/jgs.13281
Guo Y, Jia P, Zhang J, Wang X, Jiang H, Jiang W (2016) Prevalence and risk factors of postoperative delirium in elderly hip fracture patients. J Int Med Res 44(2):317–327. https://doi.org/10.1177/0300060515624936
Mason SE, Noel-Storr A, Ritchie CW (2010) The impact of general and regional anesthesia on the incidence of post-operative cognitive dysfunction and post-operative delirium: a systematic review with meta-analysis. J Alzheimers Dis 22(Suppl 3):67–79. https://doi.org/10.3233/jad-2010-101086
Sharma PT, Sieber FE, Zakriya KJ, Pauldine RW, Gerold KB, Hang J, Smith TH (2005) Recovery room delirium predicts postoperative delirium after hip-fracture repair. Anesth Analg 101(4):1215–1220, table of contents. https://doi.org/10.1213/01.ane.0000167383.44984.e5
Akunne A, Davis S, Westby M, Young J (2014) The cost-effectiveness of multi-component interventions to prevent delirium in older people undergoing surgical repair of hip fracture. Eur J Orthop Surg Traumatol 24(2):187–195. https://doi.org/10.1007/s00590-013-1170-9
Maldonado JR (2008) Pathoetiological model of delirium: a comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit Care Clin 24(4):789–856, ix. https://doi.org/10.1016/j.ccc.2008.06.004
Vardy ER, Teodorczuk A, Yarnall AJ (2015) Review of delirium in patients with Parkinson’s disease. J Neurol 262(11):2401–2410. https://doi.org/10.1007/s00415-015-7760-1
Tomasi CD, Salluh J, Soares M, Vuolo F, Zanatta F, Constantino Lde S, Zugno AI, Ritter C, Dal-Pizzol F (2015) Baseline acetylcholinesterase activity and serotonin plasma levels are not associated with delirium in critically ill patients. Rev Bras Ter Intensiva 27(2):170–177. https://doi.org/10.5935/0103-507x.20150029
Acknowledgments
We thank the authors of the included studies for their helping.
Funding
This study was supported by National Natural Science Foundation of China: (81772332); Natural Science Foundation of Jiangsu Province (BK20141281), Special Foundation Project on the Prospective Study of Social Development in Jiangsu Province (BE2013911), Jiangsu Six Categories of Talent Summit Fund (WSW-133), Social Development of Science and Technology Research Project in Yangzhou (YZ2011082), and Jiangsu Province 333 talent Project (BRA2016159).
Author information
Authors and Affiliations
Contributions
JC Wang, YX Wang, and JZ Bai conceived of the design of the study. P Zhang and Y Liang participated in the literature search and study selection. JS He and JZ Bai participated in data extraction and quality assessment. XY Liang and Y Liang performed the statistical analysis. JZ Bai finished the manuscript. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jianzhong Bai and Yuan Liang are Co-first author.
Electronic supplementary material
Appendix S1
. The details of the search strategy from PubMed, Embase, Web of Science, and Scopus (DOCX 29 kb).
Rights and permissions
About this article
Cite this article
Bai, J., Liang, Y., Zhang, P. et al. Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos Int 31, 317–326 (2020). https://doi.org/10.1007/s00198-019-05172-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05172-7