Abstract
Summary
Bone mass in childhood is highly influenced by puberty. At the same age, bone mass was higher for pubertal than pre-pubertal children. A high level of tracking during 7 years from childhood through puberty was shown, indicating that early levels of bone mass may be important for later bone health.
Introduction
Bone mass development in childhood varies by sex and age, but also by pubertal stage. The objectives of this study were to (1) describe bone mass development in childhood as it relates to pubertal onset and to (2) determine the degree of tracking from childhood to adolescence.
Methods
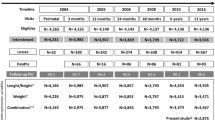
A longitudinal study with 7 years of follow-up was initiated in 2008 to include 831 children (407 boys) aged 8 to 17 years. Participants underwent whole body dual-energy X-ray absorptiometry (DXA) scanning, blood collection to quantify luteinizing hormone levels, and Tanner stage self-assessment three times during the 7-year follow-up. Total body less head bone mineral content, areal bone mineral density, and bone area were used to describe development in bone accrual and to examine tracking over 7 years.
Results
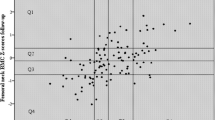
Bone mass in pubertal children is higher than that of pre-pubertal children at the same age. Analysing tracking with quintiles of bone mass Z-scores in 2008 and 2015 showed that more than 80% of participants remained in the same or neighbouring quintile over the study period. Tracking was confirmed by correlation coefficients between Z-scores at baseline and 7-year follow-up (range, 0.80–0.84).
Conclusions
Bone mass is highly influenced by pubertal onset, and pubertal stage should be considered when examining children’s bone health. Because bone mass indices track from childhood into puberty, children with low bone mass may be at risk of developing osteoporosis later in life.



Similar content being viewed by others
References
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O'Karma M, Wallace TC, Zemel BS (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 27(4):1281–1386. https://doi.org/10.1007/s00198-015-3440-3
Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver C (2000) Peak bone mass. Osteoporos Int 11(12):985–1009. https://doi.org/10.1007/s001980070020
Maggioli C, Stagi S (2017) Bone modeling, remodeling, and skeletal health in children and adolescents: mineral accrual, assessment and treatment. Ann Pediatr Endocrinol Metab 22(1):1–5. https://doi.org/10.6065/apem.2017.22.1.1
Hernandez CJ, Beaupre GS, Carter DR (2003) A theoretical analysis of the relative influences of peak BMD, age-related bone loss and menopause on the development of osteoporosis. Osteoporos Int 14(10):843–847. https://doi.org/10.1007/s00198-003-1454-8
McCormack SE, Cousminer DL, Chesi A, Mitchell JA, Roy SM, Kalkwarf HJ, Lappe JM, Gilsanz V, Oberfield SE, Shepherd JA, Winer KK, Kelly A, Grant SFA, Zemel BS (2017) Association between linear growth and bone accrual in a diverse cohort of children and adolescents. JAMA Pediatr 171:e171769. https://doi.org/10.1001/jamapediatrics.2017.1769
Zemel BS, Kalkwarf HJ, Gilsanz V, Lappe JM, Oberfield S, Shepherd JA, Frederick MM, Huang X, Lu M, Mahboubi S, Hangartner T, Winer KK (2011) Revised reference curves for bone mineral content and areal bone mineral density according to age and sex for black and non-black children: results of the bone mineral density in childhood study. J Clin Endocrinol Metab 96(10):3160–3169. https://doi.org/10.1210/jc.2011-1111
Kelly TL, Wilson KE, Heymsfield SB (2009) Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS One 4(9):e7038. https://doi.org/10.1371/journal.pone.0007038
Crabtree NJ, Shaw NJ, Bishop NJ, Adams JE, Mughal MZ, Arundel P, Fewtrell MS, Ahmed SF, Treadgold LA, Hogler W, Bebbington NA, Ward KA (2017) Amalgamated reference data for size-adjusted bone densitometry measurements in 3598 children and young adults—the ALPHABET study. J Bone Miner Res 32(1):172–180. https://doi.org/10.1002/jbmr.2935
Kang MJ, Hong HS, Chung SJ, Lee YA, Shin CH, Yang SW (2016) Body composition and bone density reference data for Korean children, adolescents, and young adults according to age and sex: results of the 2009-2010 Korean National Health and Nutrition Examination Survey (KNHANES). J Bone Miner Metab 34(4):429–439. https://doi.org/10.1007/s00774-015-0686-y
Guo B, Xu Y, Gong J, Tang Y, Xu H (2013) Age trends of bone mineral density and percentile curves in healthy Chinese children and adolescents. J Bone Miner Metab 31(3):304–314. https://doi.org/10.1007/s00774-012-0401-1
Jeddi M, Roosta MJ, Dabbaghmanesh MH, Omrani GR, Ayatollahi SM, Bagheri Z, Showraki AR, Bakhshayeshkaram M (2013) Normative data and percentile curves of bone mineral density in healthy Iranian children aged 9-18 years. Arch Osteoporos 8:114. https://doi.org/10.1007/s11657-012-0114-z
Kalkwarf HJ, Gilsanz V, Lappe JM, Oberfield S, Shepherd JA, Hangartner TN, Huang X, Frederick MM, Winer KK, Zemel BS (2010) Tracking of bone mass and density during childhood and adolescence. J Clin Endocrinol Metab 95(4):1690–1698. https://doi.org/10.1210/jc.2009-2319
Wren TA, Kalkwarf HJ, Zemel BS, Lappe JM, Oberfield S, Shepherd JA, Winer KK, Gilsanz V (2014) Longitudinal tracking of dual-energy X-ray absorptiometry bone measures over 6 years in children and adolescents: persistence of low bone mass to maturity. J Pediatr 164(6):1280–1285.e1282. https://doi.org/10.1016/j.jpeds.2013.12.040
Budek AZ, Mark T, Michaelsen KF, Molgaard C (2010) Tracking of size-adjusted bone mineral content and bone area in boys and girls from 10 to 17 years of age. Osteoporos Int 21(1):179–182. https://doi.org/10.1007/s00198-009-0932-z
Fujita Y, Iki M, Ikeda Y, Morita A, Matsukura T, Nishino H, Yamagami T, Kagamimori S, Kagawa Y, Yoneshima H (2011) Tracking of appendicular bone mineral density for 6 years including the pubertal growth spurt: Japanese Population-based Osteoporosis Kids Cohort Study. J Bone Miner Metab 29(2):208–216. https://doi.org/10.1007/s00774-010-0213-0
Foley S, Quinn S, Jones G (2009) Tracking of bone mass from childhood to adolescence and factors that predict deviation from tracking. Bone 44(5):752–757. https://doi.org/10.1016/j.bone.2008.11.009
Buttazzoni C, Rosengren BE, Tveit M, Landin L, Nilsson JA, Karlsson MK (2014) A pediatric bone mass scan has poor ability to predict adult bone mass: a 28-year prospective study in 214 children. Calcif Tissue Int 94(2):232–239. https://doi.org/10.1007/s00223-013-9802-y
Tinggaard J, Aksglaede L, Sorensen K, Mouritsen A, Wohlfahrt-Veje C, Hagen CP, Mieritz MG, Jorgensen N, Wolthers OD, Heuck C, Petersen JH, Main KM, Juul A (2014) The 2014 Danish references from birth to 20 years for height, weight and body mass index. Acta Paediatr 103(2):214–224. https://doi.org/10.1111/apa.12468
Wedderkopp N, Jespersen E, Franz C, Klakk H, Heidemann M, Christiansen C, Moller NC, Leboeuf-Yde C (2012) Study protocol. The Childhood Health, Activity, and Motor Performance School Study Denmark (The CHAMPS-study DK). BMC Pediatr 12:128. https://doi.org/10.1186/1471-2431-12-128
Roche Diagnostics GmbH M, Germany (2016) Method sheet, ms_11732234122V19.0, LH (Luteiniserende hormone), 2016-11, V 19.0 Dansk
Rasmussen AR, Wohlfahrt-Veje C, Tefre de Renzy-Martin K, Hagen CP, Tinggaard J, Mouritsen A, Mieritz MG, Main KM (2015) Validity of self-assessment of pubertal maturation. Pediatrics 135(1):86–93. https://doi.org/10.1542/peds.2014-0793
WHO (2010) WHO Anthro for personal computers, version 322, 2011: software for assessing growth and development of the world’s children Geneva: WHO, 2010. http://wwwwhoint/childgrowth/software/en/. Accessed 21 Dec 2016
Chevalley T, Bonjour JP, Ferrari S, Rizzoli R (2009) The influence of pubertal timing on bone mass acquisition: a predetermined trajectory detectable five years before menarche. J Clin Endocrinol Metab 94(9):3424–3431. https://doi.org/10.1210/jc.2009-0241
Kalkwarf HJ, Zemel BS, Gilsanz V, Lappe JM, Horlick M, Oberfield S, Mahboubi S, Fan B, Frederick MM, Winer K, Shepherd JA (2007) The bone mineral density in childhood study: bone mineral content and density according to age, sex, and race. J Clin Endocrinol Metab 92(6):2087–2099. https://doi.org/10.1210/jc.2006-2553
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, Jaworski M, Gordon CM (2014) Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom 17(2):225–242. https://doi.org/10.1016/j.jocd.2014.01.003
Buttazzoni C, Rosengren BE, Karlsson C, Dencker M, Nilsson JA, Karlsson MK (2015) A pediatric bone mass scan has poor ability to predict peak bone mass: an 11-year prospective study in 121 children. Calcif Tissue Int 96(5):379–388. https://doi.org/10.1007/s00223-015-9965-9
Nilsen OA, Ahmed LA, Winther A, Christoffersen T, Furberg AS, Grimnes G, Dennison E, Emaus N (2017) Changes and tracking of bone mineral density in late adolescence: the Tromso Study, Fit Futures. Arch Osteoporos 12(1):37. https://doi.org/10.1007/s11657-017-0328-1
Cheng S, Volgyi E, Tylavsky FA, Lyytikainen A, Tormakangas T, Xu L, Cheng SM, Kroger H, Alen M, Kujala UM (2009) Trait-specific tracking and determinants of body composition: a 7-year follow-up study of pubertal growth in girls. BMC Med 7:5. https://doi.org/10.1186/1741-7015-7-5
Heidemann M, Holst R, Schou AJ, Klakk H, Husby S, Wedderkopp N, Molgaard C (2015) The influence of anthropometry and body composition on children's bone health: the childhood health, activity and motor performance school (the CHAMPS) study, Denmark. Calcif Tissue Int 96(2):97–104. https://doi.org/10.1007/s00223-014-9941-9
Acknowledgements
We thank participants and schools for their participation in the Childhood Health Activity and Motor Performance School study.
Funding
The study was supported by The Danish foundation “Tryg-fonden”, the Region of Southern Denmark, Hospital of Southern Jutland, and “Kirsten og Freddy Johansens Fond”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Children and parents have received information both at school meetings and additional written information about the study. The parents signed informed consent forms before examination. Participation was at any time voluntary. Permission to conduct the CHAMPS-study DK was granted by the Regional Scientific Ethical Committee of Southern Denmark (Project ID: S2008-0047, S-20140105) and were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Rønne, M.S., Heidemann, M., Schou, A. et al. Tracking of bone mass from childhood to puberty: a 7-year follow-up. The CHAMPS study DK. Osteoporos Int 29, 1843–1852 (2018). https://doi.org/10.1007/s00198-018-4556-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4556-z