Abstract
Background
To obtain forensic evidence of blunt trauma injury, physical examination (PE) is necessary but is only valid when an injury is visible. Identification of previously invisible injuries through the application of ultraviolet (UV) radiation is a phenomenon that has been known for decades, but to date has only drawn little attention in German legal medicine.
Objectives
To analyze at what point in time UV examination (UVE) can be used as an additional noninvasive tool to identify potential blunt trauma injuries, especially when visual signs are absent.
Materials and methods
Retrospective analysis of reports from 28 individuals who underwent forensic examination for blunt trauma injury, including the use of UV-induced fluorescence.
Results
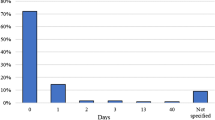
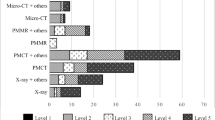
In all, 28 subjects presented with 294 claimed injuries of which 205 were forensically verified to correspond with the mechanism of injury. Injuries were visible longer with an increasing intensity of violence. UVE identified 62 % of these potential injuries in a time span of up to 31 weeks after blunt trauma, whereas PE alone identified only 19 %.
Conclusion
UVE seems to be an essential aid for blunt trauma identification from the first moment of injury and is superior to using PE alone. Therefore, UVE should be used as an additional tool with every PE, especially if the suspected injuries are older than 1 week, to obtain complete evidence of blunt trauma injuries.
Zusammenfassung
Hintergrund
Zur forensischen Dokumentation stumpfer Gewalteinwirkungen ist eine körperliche Untersuchung (PE) erforderlich, aber meist nur aussagekräftig, wenn Verletzungen sichtbar sind. Durch den Einsatz von Ultraviolettstrahlung (UV) lassen sich äußerlich nicht abzugrenzende Verletzungen sichtbar machen. Obwohl dieses Phänomen seit Jahrzehnten bekannt ist, findet es in den deutschen Instituten bisher wenig Beachtung.
Fragestellung
Ab welchem Zeitpunkt und bis zu welchem Verletzungsalter kann eine UV-Untersuchung (UVE) als ergänzende, nichtinvasive Methode zur PE angewandt werden, um mit bloßem Auge nicht (mehr) zu erkennende Verletzungen nachzuweisen?
Material und Methoden
Retrospektive Auswertung der rechtsmedizinischen Gutachten zu 28 körperlichen Untersuchungen nach stumpfen Gewalteinwirkungen, bei denen die Probanden jeweils auch mittels UV-induzierter Fluoreszenz untersucht wurden.
Ergebnisse
Die 28 Personen präsentierten sich mit 294 möglichen Verletzungen, von denen 205 Hämatome hinsichtlich ihrer Entstehungsart/ihres Entstehungszeitraums mit den anamestischen Angaben übereinstimmten. Die festgestellten Verletzungen waren umso länger sichtbar, je intensiver die Gewalteinwirkung erfolgte. Mittels UVE konnten 62 % der Hämatome bis 31 Wochen nach deren Entstehung nachgewiesen werden, während eine alleinige PE nur 19 % der Hämatome erfassen konnte.
Diskussion
Eine zusätzliche UVE scheint bereits zeitnah nach Verletzungsentstehung ergänzende Befunde zur Routine-PE beim Nachweis von Hämatomen zu liefern. Wir empfehlen eine standardisierte UVE nach allen PE, insbesondere wenn die potenziellen Verletzungen älter als eine Woche gewesen sein sollen. So können auch ältere Verletzungen dokumentiert werden.


Similar content being viewed by others
References
Barsley RE, West MH, Fair JA (1990) Forensic photography—ultraviolet imaging of wounds on skin. Am J Forensic Med Pathol 11:300–308
Carter-Snell C, Soltys K (2005) Forensic ultraviolet lights in clinical practice: evidence for the evidence. Can J Police Secur Serv 3:79–85
Diffey BL (2002) Sources and measurement of ultraviolet radiation. Methods 28:4–13
Dyer AG, Muir LL, Muntz WRA (2004) A calibrated gray scale for forensic ultraviolet photography. J Forensic Sci 49:1056–1058
Gillies R, Zonios G, Anderson RR, Kollias N (2000) Fluorescence excitation spectroscopy provides information about human skin in vivo. J Invest Dermatol 115:704–707
Hempling SM (1981) The applications of ultraviolet photography in clinical forensic medicine. Med Sci Law 21:215–222
Hughes VK, Langlois NEI (2010) Use of reflectance spectrophotometry and colorimetry in a general linear model for the determination of the age of bruises. Forensic Sci Med Pathol 6:275–281
Hughes VK, Ellis PS, Burt T, Langlois NEI (2004) The practical application of reflectance spectrophotometry for the demonstration of haemoglobin and its degradation in bruises. J Clin Pathol 57:355–359
Krauss TC (1984) Photographic techniques of concern in metric bite mark analysis. J Forensic Sci 29:633–638
Lee W, Khoo B (2010) Forensic light sources for detection of biological evidences in crime scene investigation: a review. Malaysian J Forensic Sci 1:17–27
Limmen RM, Ceelen M, Reijnders UJL et al (2012) Enhancing the visibility of injuries with narrow-banded beams of light within the visible light spectrum. J Forensic Sci 58:518–522
Lombardi M, Canter J, Patrick PA, Altman R (2015) Is fluorescence under an alternate light source sufficient to accurately diagnose subclinical bruising? J Forensic Sci 60:444–449
Lynnerup N, Hjalgrim H, Eriksen B (1995) Routine use of ultraviolet light in medicolegal examinations to evaluate stains and skin trauma. Med Sci Law 35:165–168
Maguire S, Mann M (2013) Systematic reviews of bruising in relation to child abuse-what have we learnt: an overview of review updates. Evid Based Child Heal 8:255–263
Maguire S, Mann MK, Sibert J, Kemp A (2005) Can you age bruises accurately in children? A systematic review. Arch Dis Child 90:187–189
McCullough EC (1977) Optical Radiations in Medicine. https://www.aapm.org/pubs/reports/rpt_03.pdf. Accessed 10 April 2015
Rowan P, Practitioner G, Hill M et al (2010) The use of infrared aided photography in identification of sites of bruises after evidence of the bruise is absent to the naked eye. J Forensic Leg Med 17:293–297
Scafide KRN, Sheridan DJ, Hayat MJ (2013) Evaluating change in bruise colorimetry and the effect of subject characteristics over time. Forensic Sci Med Pathol 9:367–376
Stephenson T, Bialas Y (1996) Estimation of the age of bruising. Arch Dis Child 74:53–55
Tetley C (2005) The photography of bruises. J Vis Commun Med 28:72–77
Thavarajah D, Vanezis P, Perrett D (2012) Assessment of bruise age on dark-skinned individuals using tristimulus colorimetry. Med Sci Law 52:6–11
Vogeley E, Pierce MC, Bertocci G (2002) Experience with wood lamp illumination and digital photography in the documentation of bruises on human skin. Arch Pediatr Adolesc Med 156:265–268
Wawryk J, Odell M (2005) Fluorescent identification of biological and other stains on skin by the use of alternative light sources. J Clin Forensic Med 12:296–301
West M, Barsley RE, Frair J, Stewart W (1992) Ultraviolet radiation and its role in wound pattern documentation. J Forensic Sci 37:1466–1479
West MH, Billings JD, Frair J (1987) Ultraviolet photography: bite marks on human skin and suggested technique for the exposure and development of reflective ultraviolet photography. J Forensic Sci 32:1204–1213
Wright FD, Golden GS (2010) The use of full spectrum digital photography for evidence collection and preservation in cases involving forensic odontology. Forensic Sci Int 201:59–67
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Glauche, B. Ondruschka, V. Wenzel, J. Dreßler, and C. Hädrich state that they have no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
Benjamin Ondruschka and Carsten Hädrich have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Glauche, J., Ondruschka, B., Wenzel, V. et al. Examination of invisible injuries. Rechtsmedizin 25, 543–547 (2015). https://doi.org/10.1007/s00194-015-0053-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00194-015-0053-2