Abstract
Introduction and hypothesis
There is a widely held, but untested, belief that certain exercises and activities generate intraabdominal pressure (IAP) that may compromise the function of the pelvic floor muscles. Women with, or at risk of, pelvic floor disorders are advised therefore to refrain from these exercises and activities in order to theoretically protect their pelvic floor. The aim of this study was to compare IAPs generated during exercises of different types that are recommended to women as pelvic floor “safe” with those generated during the corresponding conventional exercises that women are typically cautioned against.
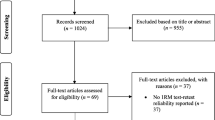
Methods
This was a cross-sectional cohort study. All participants were guided by a trained exercise practitioner through a series of ten exercise pairs, one version recommended to women as pelvic floor “safe” and one conventional version which women are cautioned against. IAP components were extracted from the pressure traces from a wireless intravaginal pressure sensor and used in multivariate linear regression modelling, canonical discriminant analysis, and linear mixed modelling.
Results
A total of 53 participants were recruited. After adjusting for age, body mass index and parity, there was an exercise type–version effect (p < 0.01). After taking into account all pressure components of the IAP trace, there was a significant difference in IAP between the recommended and discouraged versions of the same exercise for five of the ten exercise types. Coughing and the Valsalva manoeuvre generated IAPs that were distinct from those generated by the exercises.
Conclusions
No differences in IAPs were found between the recommended and discouraged versions of the same exercise for all exercise types. In particular, the IAPs generated during the two versions of ball rotations, lunges, core, push-ups and squats did not differ significantly. Performing the recommended pelvic floor “safe” version instead of the discouraged conventional version of these exercises may not necessarily protect the pelvic floor and vice versa.



Similar content being viewed by others
References
Dumoulin C, Hay-Smith EC, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2014;(5):CD005654. https://doi.org/10.1007/10.1002/14651858.CD005654.pub3.
Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2011;(12):CD003882. https://doi.org/10.1002/14651858.CD003882.pub4.
Jundt K, Peschers U, Kentenich H. The investigation and treatment of female pelvic floor dysfunction. Dtsch Arztebl Int. 2015;112(33-34):564–74.
Uustal Fornell E, Wingren G, Kjølhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83(4):383–9.
Abrams P, Cardozo L, Khoury S, Wein A. Incontinence: 5th International Consultation on Incontinence, Paris, February 2012. Paris: ICUD-EAU; 2013.
Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev, 2010;(1):CD005654. https://doi.org/10.1002/14651858.CD005654.pub2.
Imamura M, Williams K, Wells M, McGrother C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database Syst Rev. 2015;(12):CD003505. https://doi.org/10.1002/14651858.CD003505.pub5.
International Urogynecological Association. Recovery following vaginal repair surgery/vaginal hysterectomy: a guide for women. Lakeville, MN: International Urogynecological Association; 2011.
Pelvic Floor First - Promoting pelvic floor safe exercises, C. Foundation, Editor. 2011, Continence Foundation of Australia. http://www.pelvicfloorfirst.org.au/
Royal College of Obstetricians and Gynaecologists. Recovering well: information for you after a pelvic floor repair operation. London: Royal College of Obstetricians and Gynaecologists; 2015.
Brown WJ, Bauman A, Bull FC, Burton NW. Development of evidence-based physical activity recommendations for adults (18–64 years). Canberra: Australian Government Department of Health; 2012.
Ministry of Health. Eating and activity guidelines for New Zealand adults. Wellington, New Zealand: Ministry of Health; 2015.
Thompson WR. Worldwide survey of fitness trends for 2017. ACSMs Health Fit J. 2016;20(6):8–17.
Coleman TJ, Hamad NM, Shaw JM, Egger MJ, Hsu Y, Hitchcock R, Jin H, Choi CK, Nygaard IE. Effects of walking speeds and carrying techniques on intra-abdominal pressure in women. Int Urogynecol J. 2015;26(7):967–74.
Guttormson R, Tschirhart J, Boysen D, Martinson K. Are postoperative activity restrictions evidence-based? Am J Surg. 2008;195(3):401–4.
Hamad NM, Shaw JM, Nygaard IE, Coleman TJ, Hsu Y, Egger M, Hitchcock RW. More complicated than it looks: the vagaries of calculating intra-abdominal pressure. J Strength Cond Res. 2013;27(11):3204–15.
Kruger J, Hayward L, Nielsen P, Loiselle D, Kirton R. Design and development of a novel intra-vaginal pressure sensor. Int Urogynecol J. 2013;24(10):1715–21.
O'Dell K, Morse AN, Crawford SL, Howard A. Vaginal pressure during lifting, floor exercises, jogging, and use of hydraulic exercise machines. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(12):1481–9.
Shaw JM, Hamad NM, Coleman TJ, Egger MJ, Hsu Y, Hitchcock R, Nygaard IE. Intra-abdominal pressures during activity in women using an intra-vaginal pressure transducer. J Sports Sci. 2014;32(12):1176–85.
Kuncharapu I, Majeroni BA, Johnson DW. Pelvic organ prolapse. Am Fam Physician. 2010;81(9):1111–7.
Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci. 2007;1101:266–96.
Bo K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(2):76–84.
Schell A, Budgett D, Nielsen P, Smalldridge J, Hayward L, Dumoulin C, Kruger J. Design and development of a novel intra-vaginal sensor array. Neurourol Urodyn. 2016;35(4):S355–6.
Noblett K, Jensen J, Ostergard D. The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. Int Urogynecol J. 1997;8(6):323–6.
Wilson A, Longhi J, Goldman C, McNatt S. Intra-abdominal pressure and the morbidly obese patients: the effect of body mass index. J Trauma. 2010;69(1):78–83.
Acknowledgements
We acknowledge Daniel Quach, Helen Li and Duncan Cunninghame for collecting and processing the IAP data. We are also grateful to the University of Auckland’s Department of Exercise Sciences for kindly allowing us to use their facilities as well as to all the exercise practitioners who volunteered their time for this project. A special acknowledgement to Sally Jo for her fantastic illustrations of the exercises that added clarity to the project methodology. Lastly we thank the study participants who volunteered their time and made this project possible.
Funding
Funding and financial support was provided by the Aotearoa Foundation Bioengineering Postdoctoral Fellowship (J.A. Kruger) and Jean Heywood Postgraduate Scholarship (T.Y. Tian).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 278 kb)
Rights and permissions
About this article
Cite this article
Tian, T., Budgett, S., Smalldridge, J. et al. Assessing exercises recommended for women at risk of pelvic floor disorders using multivariate statistical techniques. Int Urogynecol J 29, 1447–1454 (2018). https://doi.org/10.1007/s00192-017-3473-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3473-6