Abstract
Purpose
The purpose of this study was to assess the variations in tibial tubercle–trochlear groove distance and angle as a function of age and gender in a population of children without patellar instability (PI) compared with those with PI.
Methods
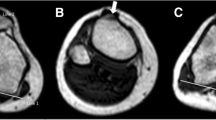
A retrospective review of 869 children’s knee MRIs, ages 5 to 15 years, were evaluated using a control group (792 children) without evidence of PI and a group with PI (77 children). Tibial tubercle–trochlear groove distance (TT–TGd) and angle (TT–TGa) were measured twice by two readers to assess intra- and inter-observer reliability and compared between PI and control groups. In both groups, functions of age and gender on TT–TGd and TT–TGa values were evaluated.
Results
Both TT–TGd and TT–TGa measurements showed excellent intra- and inter-observer reliability. The mean TT–TGd for the PI group was 17.2 mm (SD 6.6) and significantly higher than the mean TT–TGd for the control group (10.4 SD 3.8 mm, P = 0.001). The mean TT–TGa for the PI was 20.8° (SD 8.3°), which was also significantly higher than the mean TT–TGa for the control group (12.5° SD 4.6°, P < 0.001). Control group revealed a positive correlation between age and TT–TGd measurements (r = 0.243, P < 0.001). The mean TT–TGa for girls (13.3° SD 4.7°) was higher than the mean TT–TGa for boys (11.9° SD 4.4°) in the control group (P < 0.001).
Conclusion
TT–TGa and TT–TGd are reliable and can be used for the evaluation of the extansor mechanism alignment in children with and without PI. However, it must be considered that TT–TGd is increasing in growing patients. Soft-tissue procedures may be prone to failure, since bony procedures for patellar alignment cannot be done until skeletal maturity.
Level of evidence
III.




Similar content being viewed by others
References
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med 45:50–58
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15:39–46
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dickens AJ, Morrell NT, Doering A, Tandberg D, Treme G (2014) Tibial tubercle–trochlear groove distance: defining normal in a pediatric population. J Bone Joint Surg Am 96:318–324
Duppe K, Gustavsson N, Edmonds EW (2016) Developmental morphology in childhood patellar instability: age-dependent differences on magnetic resonance imaging. J Pediatr Orthop 36:870–876
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Gordon JE, Schoenecker PL (1999) Surgical treatment of congenital dislocation of the patella. J Pediatr Orthop 19:260–264
Goutallier D, Bernageau J, Lecudonnec B (1978) [The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl)]. Rev Chir Orthop Reparatrice Appar Mot 64:423–428
Hennrikus W, Pylawka T (2013) Patellofemoral instability in skeletally immature athletes. Instr Course Lect 62:445–453
Hinckel BB, Gobbi RG, Kihara Filho EN, Demange MK, Pecora JR, Camanho GL (2015) Patellar tendon-trochlear groove angle measurement: a new method for patellofemoral rotational analyses. Orthop J Sports Med 3:2325967115601031
Kuroda R, Nagai K, Matsushita T, Araki D, Matsumoto T, Takayama K et al (2017) A new quantitative radiographic measurement of patella for patellar instability using the lateral plain radiograph: ‘patellar width ratio’. Knee Surg Sports Traumatol Arthrosc 25:123–128
Muneta T, Yamamoto H, Ishibashi T, Asahina S, Furuya K (1994) Computerized tomographic analysis of tibial tubercle position in the painful female patellofemoral joint. Am J Sports Med 22:67–71
Nagamine R, Miura H, Inoue Y, Tanaka K, Urabe K, Okamoto Y et al (1997) Malposition of the tibial tubercle during flexion in knees with patellofemoral arthritis. Skeletal Radiol 26:597–601
Nelitz M, Theile M, Dornacher D, Wolfle J, Reichel H, Lippacher S (2012) Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc 20:822–828
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14:513–515
Novacheck TF, Stout JL, Gage JR, Schwartz MH (2009) Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. Surgical technique. J Bone Joint Surg Am 91(Suppl 2):271–286
Pennock AT, Alam M, Bastrom T (2014) Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med 42:389–393
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Tsujimoto K, Kurosaka M, Yoshiya S, Mizuno K (2000) Radiographic and computed tomographic analysis of the position of the tibial tubercle in recurrent dislocation and subluxation of the patella. Am J Knee Surg 13:83–88
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
This study was approved by Baltalimani Bone Diseases Education and Research Hospital Institutional Review Board (03.08.2017/12).
Informed consent
Informed consent was waived, because the study was a retrospective cross-sectional review.
Rights and permissions
About this article
Cite this article
Bayhan, I.A., Kirat, A., Alpay, Y. et al. Tibial tubercle–trochlear groove distance and angle are higher in children with patellar instability. Knee Surg Sports Traumatol Arthrosc 26, 3566–3571 (2018). https://doi.org/10.1007/s00167-018-4997-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4997-0