Abstract
Purpose
Osteochondral autologous transplantation (OAT) from the ipsilateral femoral lateral condyle in osteochondritis dissecans (OD) of the talus has shown good clinical results in the past. To further define, indications and limitations of OAT various factors have been discussed which might influence the clinical outcome.
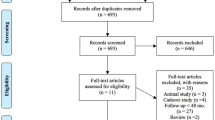
Methods
In this study, the clinical outcome of OAT of 32 patients (mean follow-up 29 months) was evaluated by means of the American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Scale, ankle pain on the visual analogue scale (VAS), and Hospital for Special Surgery (HSS) Patella score. We then analysed the statistical correlation between clinical outcome and various variables such as age, pre-existing osteoarthritis, or size of the lesion.
Results
Median AOFAS score was 86 (range 68–100), median ankle pain on VAS was 2.0 (range 0–5.5), and median HSS Patella score was 95 (range 35–100). Advanced age (above 40 years of age) was associated with a significantly lower HSS Patella score (80 vs. 97.5, p = 0.035). None of the other variables (obesity, pre-existing osteoarthritis, size of the lesion, necessity of malleolar osteotomy, localization of the lesion, and number of previous surgeries) influenced the clinical outcome adversely.
Conclusions
Osteochondral autologous transplantation in OD of the talus is a safe procedure with good clinical results. As advanced age is associated with higher donor-site morbidity, indication for OAT in older patients should be carefully considered. As none of the other variables affected the clinical outcome of OAT adversely, there is no contraindication for OAT, for example, in osteochondral lesions requiring more than one osteochondral grafts, lateral lesions, patients with BMI >25, pre-existing osteoarthritis, or failed previous surgery.
Level of evidence
IV.





Similar content being viewed by others
References
Al-Shaikh RA, Chou LB, Mann JA, Dreeben SM, Prieskorn D (2002) Autologous osteochondral grafting for talar cartilage defects. Foot Ankle Int 23(5):381–389
Assenmacher JA, Kelikian AS, Gottlob C, Kodros S (2001) Arthroscopically assisted autologous osteochondral transplantation for osteochondral lesions of the talar dome: an MRI and clinical follow-up study. Foot Ankle Int 22(7):544–551
Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP (2006) A new patellofemoral scoring system for total knee arthroplasty. Clin Orthop Relat Res 452:150–154
Baltzer AW, Arnold JP (2005) Bone-cartilage transplantation from the ipsilateral knee for chondral lesions of the talus. Arthroscopy 21(2):159–166
Berndt AL, Harty M (1959) Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 41-A:988–1020
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A(Suppl 2):58–69
Gautier E, Kolker D, Jakob RP (2002) Treatment of cartilage defects of the talus by autologous osteochondral grafts. J Bone Joint Surg Br 84(2):237–244
Haasper C, Zelle BA, Knobloch K, Jagodzinski M, Citak M, Lotz J, Krettek C, Zeichen J (2008) No mid-term difference in mosaicplasty in previously treated versus previously untreated patients with osteochondral lesions of the talus. Arch Orthop Trauma Surg 128(5):499–504
Hangody L, Kish G, Modis L, Szerb I, Gaspar L, Dioszegi Z, Kendik Z (2001) Mosaicplasty for the treatment of osteochondritis dissecans of the talus: two to seven year results in 36 patients. Foot Ankle Int 22(7):552–558
Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, Bodo G (2008) Autologous osteochondral grafting–technique and long-term results. Injury 39(Suppl 1):S32–S39
Imhoff AB, Paul J, Ottinger B, Wortler K, Lammle L, Spang J, Hinterwimmer S (2011) Osteochondral transplantation of the talus: long-term clinical and magnetic resonance imaging evaluation. Am J Sports Med 39(7):1487–1493
Kim YS, Park EH, Kim YC, Koh YG, Lee JW (2012) Factors associated with the clinical outcomes of the osteochondral autograft transfer system in osteochondral lesions of the talus: second-look arthroscopic evaluation. Am J Sports Med 40(12):2709–2719
Kokkinakis M, Kafchitsas K, Rajeev A, Mortier J (2008) Is MRI useful in the early follow-up after autologous osteochondral transplantation? Acta Orthop Belg 74(5):636–642
Kreuz PC, Lahm A, Haag M, Kostler W, Konrad G, Zwingmann J, Hauschild O, Niemeyer P, Steinwachs M (2008) Tibial wedge osteotomy for osteochondral transplantation in talar lesions. Int J Sports Med 29(7):584–589
Laffenetre O (2010) Osteochondral lesions of the talus: Current concept. Orthop Traumatol Surg Res 96 (5):554–566
Link TM, Mischung J, Wortler K, Burkart A, Rummeny EJ, Imhoff AB (2006) Normal and pathological MR findings in osteochondral autografts with longitudinal follow-up. Eur Radiol 16(1):88–96
Ollat D, Lebel B, Thaunat M, Jones D, Mainard L, Dubrana F, Versier G (2011) Mosaic osteochondral transplantations in the knee joint, midterm results of the SFA multicenter study. Orthop Traumatol Surg Res 97(8 Suppl):S160–S166
Paul J, Sagstetter A, Kriner M, Imhoff AB, Spang J, Hinterwimmer S (2009) Donor-site morbidity after osteochondral autologous transplantation for lesions of the talus. J Bone Joint Surg Am 91(7):1683–1688
Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E (2007) The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med 35(1):80–85
Sammarco GJ, Makwana NK (2002) Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int 23(8):693–698
Schottle PB, Oettl GM, Agneskirchner JD, Imhoff AB (2001) Operative therapy of osteochondral lesions of the talus with autologous cartilage-bone transplantation. Orthopade 30(1):53–58
Steinhagen J, Niggemeyer O, Bruns J (2001) Etiology and pathogenesis of osteochondrosis dissecans tali. Orthopade 30(1):20–27
Valderrabano V, Leumann A, Rasch H, Egelhof T, Hintermann B, Pagenstert G (2009) Knee-to-ankle mosaicplasty for the treatment of osteochondral lesions of the ankle joint. Am J Sports Med 37(Suppl 1):105S–111S
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woelfle, J.V., Reichel, H. & Nelitz, M. Indications and limitations of osteochondral autologous transplantation in osteochondritis dissecans of the talus. Knee Surg Sports Traumatol Arthrosc 21, 1925–1930 (2013). https://doi.org/10.1007/s00167-013-2483-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2483-2