Abstract
Purpose
To assess the impact of performance status (PS) impairment 1 week before hospital admission on the outcomes in patients admitted to intensive care units (ICU).
Methods
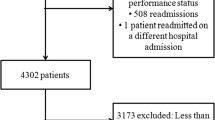
Retrospective cohort study in 59,693 patients (medical admissions, 67 %) admitted to 78 ICUs during 2013. We classified PS impairment according to the Eastern Cooperative Oncology Group (ECOG) scale in absent/minor (PS = 0–1), moderate (PS = 2) or severe (PS = 3–4). We used univariate and multivariate logistic regression analyses to investigate the association between PS impairment and hospital mortality.
Results
PS impairment was moderate in 17.3 % and severe in 6.9 % of patients. The hospital mortality was 14.4 %. Overall, the worse the PS, the higher the ICU and hospital mortality and length of stay. In addition, patients with worse PS were less frequently discharged home. PS impairment was associated with worse outcomes in all SAPS 3, Charlson Comorbidity Index and age quartiles as well as according to the admission type. Adjusting for other relevant clinical characteristics, PS impairment was associated with higher hospital mortality (odds-ratio (OR) = 1.96 (95 % CI 1.63–2.35), for moderate and OR = 4.22 (3.32–5.35), for severe impairment). The effects of PS on the outcome were particularly relevant in the medium range of severity-of-illness. These results were consistent in the subgroup analyses. However, adding PS impairment to the SAPS 3 score improved only slightly its discriminative capability.
Conclusion
PS impairment was associated with worse outcomes independently of other markers of chronic health status, particularly for patients in the medium range of severity of illness.




Similar content being viewed by others
References
Moreno RP, Metnitz PGH, Almeida E et al (2005) SAPS 3–from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 31:1345–1355. doi:10.1007/s00134-005-2763-5
Salluh JIF, Soares M (2014) ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care 20:557–565. doi:10.1097/MCC.0000000000000135
Zimmerman JE, Kramer AA, McNair DS, Malila FM (2006) Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med 34:1297–1310. doi:10.1097/01.CCM.0000215112.84523.F0
Higgins TL, Teres D, Copes WS et al (2007) Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III). Crit Care Med 35:827–835. doi:10.1097/01.CCM.0000257337.63529.9F
Zampieri FG, Colombari F (2014) The impact of performance status and comorbidities on the short-term prognosis of very elderly patients admitted to the ICU. BMC Anesthesiol 14:59. doi:10.1186/1471-2253-14-59
Rosolem MM, Rabello LSCF, Lisboa T et al (2012) Critically ill patients with cancer and sepsis: clinical course and prognostic factors. J Crit Care 27:301–307. doi:10.1016/j.jcrc.2011.06.014
Torres VBL, Azevedo LCP, Silva UVA et al (2015) Sepsis-associated outcomes in critically ill patients with malignancies. Ann Am Thorac Soc 12:1185–1192. doi:10.1513/AnnalsATS.201501-046OC
Bagshaw SM, Stelfox HT, McDermid RC et al (2014) Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ 186:E95–E102. doi:10.1503/cmaj.130639
Park C-M, Koh Y, Jeon K et al (2014) Impact of Eastern Cooperative Oncology Group Performance Status on hospital mortality in critically ill patients. J Crit Care 29:409–413. doi:10.1016/j.jcrc.2014.01.016
Azoulay E, Mokart D, Pène F et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium–a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol 31:2810–2818. doi:10.1200/JCO.2012.47.2365
Dolgin NH, Martins PNA, Movahedi B et al (2016) Functional status predicts postoperative mortality after liver transplantation. Clin Transplant. doi:10.1111/ctr.12808
Soares M, Bozza FA, Angus DC et al (2015) Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med 41:2149–2160. doi:10.1007/s00134-015-4076-7
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Stekhoven DJ, Bühlmann P (2012) MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics 28:112–118. doi:10.1093/bioinformatics/btr597
Vesin A, Azoulay E, Ruckly S et al (2013) Reporting and handling missing values in clinical studies in intensive care units. Intensive Care Med 39:1396–1404. doi:10.1007/s00134-013-2949-1
Pencina MJ, D’Agostino RB, Demler OV (2012) Novel metrics for evaluating improvement in discrimination: net reclassification and integrated discrimination improvement for normal variables and nested models. Stat Med 31:101–113. doi:10.1002/sim.4348
Chirag R, Parikh HT (2014) Key concepts and limitations of statistical methods for evaluating biomarkers of kidney disease. J Am Soc Nephrol 25:1621
Steyerberg EW, Vickers AJ, Cook NR et al (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138. doi:10.1097/EDE.0b013e3181c30fb2
Kerr KF, Wang Z, Janes H et al (2014) Net reclassification indices for evaluating risk prediction instruments: a critical review. Epidemiology 25:114–121. doi:10.1097/EDE.0000000000000018
R Core Team (2015) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Harrell FE Jr (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer-Verlag, New York. doi:10.1007/978-1-4757-3462-1
Wickham H (2009) ggplot2: elegant graphics for data analysis. Springer, New York
Prigerson HG, Bao Y, Shah MA et al (2015) Chemotherapy use, performance status, and quality of life at the end of life. JAMA Oncol 1:778–784. doi:10.1001/jamaoncol.2015.2378
Soares M, Toffart A-C, Timsit J-F et al (2014) Intensive care in patients with lung cancer: a multinational study. Ann Oncol 25:1829–1835. doi:10.1093/annonc/mdu234
Soares M, Caruso P, Silva E et al (2010) Characteristics and outcomes of patients with cancer requiring admission to intensive care units: a prospective multicenter study. Crit Care Med 38:9–15. doi:10.1097/CCM.0b013e3181c0349e
Cook NR (2007) Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation 115:928–935. doi:10.1161/CIRCULATIONAHA.106.672402
Vickers AJ, Cronin AM, Begg CB (2011) One statistical test is sufficient for assessing new predictive markers. BMC Med Res Methodol 11:13. doi:10.1186/1471-2288-11-13
Buccheri G, Ferrigno D, Tamburini M (1996) Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer 32A:1135–1141
Soares M, Salluh JIF, Spector N, Rocco JR (2005) Characteristics and outcomes of cancer patients requiring mechanical ventilatory support for >24 hrs. Crit Care Med 33:520–526
Forte DN, Vincent JL, Velasco IT, Park M (2012) Association between education in EOL care and variability in EOL practice: a survey of ICU physicians. Intensive Care Med 38:404–412. doi:10.1007/s00134-011-2400-4
Acknowledgments
This study was supported by the National Council for Scientific and Technological Development (CNPq) (Grant No 304240/2014-1), Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ) and by departmental funds from the D’Or Institute for Research and Education.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Soares and Dr. Salluh are founders and equity shareholders of Epimed Solutions®, which markets the Epimed Monitor System®, a cloud-based software for ICU management and benchmarking. The other authors declare that they have no conflict of interest.
Additional information
We dedicate this work to the memory of our colleague, Dr. Marcelo Lugarinho, who recently passed away.
Take-home message: Impaired performance status at 1 week prior to hospital admission is associated with worse outcomes independently of other markers of baseline health status, such as comorbidities and age. This association is more distinguishable in the mid-range severity of illness scores.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zampieri, F.G., Bozza, F.A., Moralez, G.M. et al. The effects of performance status one week before hospital admission on the outcomes of critically ill patients. Intensive Care Med 43, 39–47 (2017). https://doi.org/10.1007/s00134-016-4563-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4563-5