Abstract
Purpose
The use of epinephrine (EN) or vasopressin (VP) in hemorrhagic shock is well established. Due to its specific neurovascular effects, VP might be superior in concern to brain tissue integrity. The aim of this study was to evaluate cerebral effects of either EN or VP resuscitation after hemorrhagic shock.
Methods
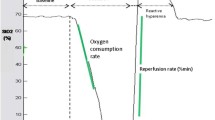
After shock induction fourteen pigs were randomly assigned to two treatment groups. After 60 min of shock, resuscitation with either EN or VP was performed. Hemodynamics, arterial blood gases as well as cerebral perfusion pressure (CPP) and brain tissue oxygenation (PtiO2) were recorded. Interstitial lactate, pyruvate, glycerol and glutamate were assessed by cerebral and subcutaneous microdialysis. Treatment-related effects were compared using one-way ANOVA with post hoc Bonferroni adjustment (p < 0.05) for repeated measures.
Results
Induction of hemorrhagic shock led to a significant (p < 0.05) decrease of mean arterial pressure (MAP), cardiac output (CO) and CPP. Administration of both VP and EN sufficiently restored MAP and CPP and maintained physiological PtiO2 levels. Brain tissue metabolism was not altered significantly during shock and subsequent treatment with VP or EN. Concerning the excess of glycerol and glutamate, we found a significant EN-related release in the subcutaneous tissue, while brain tissue values remained stable during EN treatment. VP treatment resulted in a non-significant increase of cerebral glycerol and glutamate.
Conclusions
Both vasopressors were effective in restoring hemodynamics and CPP and in maintaining brain oxygenation. With regards to the cerebral metabolism, we cannot support beneficial effects of VP in this model of hemorrhagic shock.



Similar content being viewed by others
References
Chen RY, Fan FC, Schuessler GB, Simchon S, Chien S. Regional cerebral blood flow and oxygen consumption of the canine brain during hemorrhagic hypotension. Stroke. 1984;15(2):343–50.
Spahn DR, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care. 2013;17(2):R76.
Sperry JL, Minei JP, Frankel HL, West MA, Harbrecht BG, Moore EE, et al. Early use of vasopressors after injury: caution before constriction. J Trauma. 2008;64(1):9–14.
Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, et al. European Resuscitation Council Guidelines for Resuscitation 2015: section 1. Executive summary. Resuscitation. 2015;95:1–80.
Ditchey RV, Lindenfeld J. Failure of epinephrine to improve the balance between myocardial oxygen supply and demand during closed-chest resuscitation in dogs. Circulation. 1988;78(2):382–9.
Dünser MW, Mayr AJ, Ulmer H, Knotzer H, Sumann G, Pajk W, et al. Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation. 2003;107(18):2313–9.
Morales D, Madigan J, Cullinane S, Chen J, Heath M, Oz M, et al. Reversal by vasopressin of intractable hypotension in the late phase of hemorrhagic shock. Circulation. 1999;3(100):226–9.
Raedler C, Voelckel WG, Wenzel V, Krismer AC, Schmittinger CA, Herff H, et al. Treatment of uncontrolled hemorrhagic shock after liver trauma: fatal effects of fluid resuscitation versus improved outcome after vasopressin. Anesth Analg. 2004;98(6):1759–66.
Stadlbauer KH, Wagner-Berger HG, Raedler C, Voelckel WG, Wenzel V, Krismer AC, et al. Vasopressin, but not fluid resuscitation, enhances survival in a liver trauma model with uncontrolled and otherwise lethal hemorrhagic shock in pigs. Anesthesiology. 2003;98(3):699–704.
Voelckel WG, Raedler C, Wenzel V, Lindner KH, Krismer AC, Schmittinger CA, et al. Arginine vasopressin, but not epinephrine, improves survival in uncontrolled hemorrhagic shock after liver trauma in pigs. Crit Care Med. 2003;31(4):1160–5.
Holmes CL, Patel BM, Russell JA, Walley KR. Physiology of vasopressin relevant to management of septic shock. Chest. 2001;120(3):989–1002.
Sanui M, King DR, Feinstein AJ, Varon AJ, Cohn SM, Proctor KG. Effects of arginine vasopressin during resuscitation from hemorrhagic hypotension after traumatic brain injury. Crit Care Med. 2006;34(2):433–8.
Cavus E, Meybohm P, Doerges V, Hugo HH, Steinfath M, Nordstroem J, et al. Cerebral effects of three resuscitation protocols in uncontrolled haemorrhagic shock: a randomised controlled experimental study. Resuscitation. 2009;80(5):567–72.
Clark JD, Gebhart GF, Gonder JC, Keeling ME, Kohn DF. Special report: the 1996 guide for the care and use of laboratory animals. ILAR J. 1997;38(1):41–8.
Wiggers HC, Inhraham RC, Dille J. Hemorrhagic-hypotension shock in locally anesthetized dogs. Am J Physiol. 1945;143:126–33.
Plurad DS, Talving P, Lam L, Inaba K, Green D, Demetriades D. Early vasopressor use in critical injury is associated with mortality independent from volume status. J Trauma. 2011;71(3):565–70.
Sperry JL, Minei JP, Frankel HL, West MA, Harbrecht BG, Moore EE, et al. Early use of vasopressors after injury: caution before constriction. J Trauma. 2008;64(1):9–14.
Cohn SM, McCarthy J, Stewart RM, Jonas RB, Dent DL, Michalek JE. Impact of low-dose vasopressin on trauma outcome: prospective randomized study. World J Surg. 2011;35(2):430–9.
Beloncle F, Meziani F, Lerolle N, Radermacher P, Asfar P. Does vasopressor therapy have an indication in hemorrhagic shock? Ann Intensive Care. 2013;3(1):13.
Meybohm P, Cavus E, Bein B, Steinfath M, Weber B, Hamann C, et al. Small volume resuscitation: a randomized controlled trial with either norepinephrine or vasopressin during severe hemorrhage. J Trauma. 2007;62(3):640–6.
D’Alessandro A, Moore HB, Moore EE, Wither M, Nemkov T, Gonzalez E, et al. Early hemorrhage triggers metabolic responses that build up during prolonged shock. Am J Physiol Regul Integr Comp Physiol. 2015;308(12):R1034–44.
Peltz ED, D’Alessandro A, Moore EE, Chin T, Silliman CC, Sauaia A, et al. Pathologic metabolism: an exploratory study of the plasma metabolome of critical injury. J Trauma Acute Care Surg. 2015;78(4):742–51.
Clendenen N, Nunns GR, Moore EE, Reisz JA, Gonzalez E, Peltz E, et al. Hemorrhagic shock and tissue injury drive distinct plasma metabolome derangements in swine. J Trauma Acute Care Surg. 2017;83(4):635–42.
Vogt N, Herden C, Roeb E, Roderfeld M, Eschbach D, Steinfeldt T, et al. Cerebral alterations following experimental multiple trauma and hemorrhagic shock. Shock. 2018;49(2):164–73.
Ida KK, Otsuki DA, Sasaki AT, Borges ES, Castro LU, Sanches TR, et al. Effects of terlipressin as early treatment for protection of brain in a model of haemorrhagic shock. Crit Care. 2015;19:107.
Cavus E, Meybohm P, Dörges V, Stadlbauer KH, Wenzel V, Weiss H, et al. Regional and local brain oxygenation during hemorrhagic shock: a prospective experimental study on the effects of small-volume resuscitation with norepinephrine. J Trauma. 2008;64(3):641–8 (discussion 648-9).
Sarrafzadeh AS, Haux D, Lüdemann L, Amthauer H, Plotkin M, Küchler I, et al. Cerebral ischemia in aneurysmal subarachnoid hemorrhage: a correlative microdialysis-PETstudy. Stroke. 2004;35(3):638–43.
Meybohm P, Cavus E, Bein B, Steinfath M, Brand PA, Scholz J, et al. Cerebral metabolism assessed with microdialysis in uncontrolled hemorrhagic shock after penetrating liver trauma. Anesth Analg. 2006;103(4):948–54.
Meybohm P, Cavus E, Bein B, Steinfath M, Weber B, Scholz J, et al. Neurochemical monitoring using intracerebral microdialysis during systemic haemorrhage. Acta Neurochir (Wien). 2007;149(7):691–8.
Larentzakis A, Toutouzas KG, Papalois A, Lapidakis G, Doulgerakis S, Doulami G, et al. Porcine model of hemorrhagic shock with microdialysis monitoring. J Surg Res. 2013;179(1):e177–82.
Berkowitz ID, Gervais H, Schleien CL, Koehler RC, Dean JM, Traystman RJ. Epinephrine dosage effects on cerebral and myocardial blood flow in an infant swine model of cardiopulmonary resuscitation. Anesthesiology. 1991;75(6):1041–50.
Nosrati R, Lin S, Mohindra R, Ramadeen A, Toronov V, Dorian P. Study of the effects of epinephrine on cerebral oxygenation and metabolism during cardiac arrest and resuscitation by hyperspectral near-infrared spectroscopy. Crit Care Med. 2019. https://doi.org/10.1097/ccm.0000000000003640.
Luchette FA, Jenkins WA, Friend LA, Su C, Fischer JE, James JH. Hypoxia is not the sole cause of lactate production during shock. J Trauma. 2002;52(3):415–9.
Levy B, Mansart A, Bollaert PE, Franck P, Mallie JP. Effects of epinephrine and norepinephrine on hemodynamics, oxidative metabolism, and organ energetics in endotoxemic rats. Intensive Care Med. 2003;29(2):292–300.
Di Giantomasso D, Bellomo R, May CN. The haemodynamic and metabolic effects of epinephrine in experimental hyperdynamic septic shock. Intensive Care Med. 2005;31:454–62.
Hutchinson PJ, Jalloh I, Helmy A, Carpenter KL, Rostami E, Bellander BM, et al. Consensus statement from the 2014 International Microdialysis Forum. Intensive Care Med. 2015;41(9):1517–28.
Hillered L, Valtysson J, Enblad P, Persson L. Interstitial glycerol as a marker for membrane phospholipid degradation in the acutely injured human brain. J Neurol Neurosurg Psychiatry. 1998;64(4):486–91.
Nielsen TH, Olsen NV, Toft P, Nordstrom CH. Cerebral energy metabolism during mitochondrial dysfunction induced by cyanide in piglets. Acta Anaesthesiol Scand. 2013;57(6):793–801.
Johnston AJ, Gupta AK. Advanced monitoring in the neurology intensive care unit: microdialysis. Curr Opin Crit Care. 2002;8(2):121–7.
Tisdall MM, Smith M. Cerebral microdialysis: research technique or clinical tool. Br J Anaesth. 2006;97(1):18–25.
Kett-White R, Hutchinson PJ, Al-Rawi PG, Gupta AK, Pickard JD, Kirkpatrick PJ. Adverse cerebral events detected after subarachnoid hemorrhage using brain oxygen and microdialysis probes. Neurosurgery. 2002;50(6):1213–21.
Chamoun R, Suki D, Gopinath SP, Goodman JC, Robertson C. Role of extracellular glutamate measured by cerebral microdialysis in severe traumatic brain injury. J Neurosurg. 2010;113(3):564–70.
Millet L, Barbe P, Lafontan M, Berlan M, Galitzky J. Catecholamine effects on lipolysis and blood flow in human abdominal and femoral adipose tissue. J Appl Physiol. 1998;85(1):181–8.
Wenzel V, Lindner KH, Krismer AC, Miller EA, Voelckel WG, Lingnau W. Repeated administration of vasopressin but not epinephrine maintains coronary perfusion pressure after early and late administration during prolonged cardiopulmonary resuscitation in pigs. Circulation. 1999;99(10):1379–84.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This animal study has been approved by the institutional ethics committee. All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Küchler, J., Klaus, S., Bahlmann, L. et al. Cerebral effects of resuscitation with either epinephrine or vasopressin in an animal model of hemorrhagic shock. Eur J Trauma Emerg Surg 46, 1451–1461 (2020). https://doi.org/10.1007/s00068-019-01158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01158-6