Abstract
Purpose
Radiographic indications for primary splenectomy (PS) in blunt splenic injury (BSI) after radiographic diagnosis are unknown. Improved understanding of radiographic characteristics of patients requiring splenectomy will help to appropriately triage patients to PS or non-operative management (NOM).
Methods
A retrospective, single-center review was performed of BSI diagnosed with computerized tomography (CT). Patients undergoing splenectomy prior to CT diagnosis were excluded.
Results
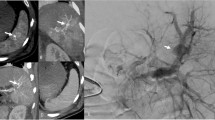
BSI was identified in 195 patients. On logistic regression, only subcapsular hematoma presence (OR 7.521, p = 0.002) and left upper quadrant hemoperitoneum (OR 6.146, p = 0.03) were associated with need for PS, while splenic laceration length, number of pseudoaneurysms (PSA), and active contrast extravasation (NS for all) were not.
Conclusions
Need for PS is predicted by extra-parenchymal pathology in subcapsular hematoma and hemoperitoneum. Splenic vascular injuries through PSA and active contrast extravasation do not predict the need for PS and can be considered for NOM.


Similar content being viewed by others
References
Moore EE, Cogbill TH, Jurkovich GJ, et al. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38(3):323–4.
Bee TK, Croce MA, Miller PR, et al. Failures of splenic nonoperative management: is the glass half empty or half full? J Trauma. 2001;50(2):230–6.
Duchesne JC, Simmons JD, Schmieg RE Jr, et al. Proximal splenic angioembolization does not improve outcomes in treating blunt splenic injuries compared with splenectomy: a cohort analysis. J Trauma. 2008;65(6):1346–51 (discussion 1351–3).
Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma. 2005;58(3):492–8.
Peitzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: multi-institutional study of the Eastern Association for the Surgery of Trauma. J Trauma. 2000;49(2):177–87 (discussion 187–9).
Harbrecht BG, Peitzman AB, Rivera L, et al. Contribution of age and gender to outcome of blunt splenic injury in adults: multicenter study of the eastern association for the surgery of trauma. J Trauma. 2001;51(5):887–95.
Marmery H, Shanmuganathan K, Mirvis SE, et al. Correlation of multidetector CT findings with splenic arteriography and surgery: prospective study in 392 patients. J Am Coll Surg. 2008;206(4):685–693.
Nix JA, Costanza M, Daley BJ, et al. Outcome of the current management of splenic injuries. J Trauma. 2001;50(5):835–42.
Renzulli P, Gross T, Schnuriger B, et al. Management of blunt injuries to the spleen. Br J Surg. 2010;97(11):1696–703.
Velmahos GC, Chan LS, Kamel E, et al. Nonoperative management of splenic injuries: have we gone too far? Arch Surg. 2000;135(6):674–9 (discussion 679–81).
Federle MP, Courcoulas AP, Powell M, et al. Blunt splenic injury in adults: clinical and CT criteria for management, with emphasis on active extravasation. Radiology. 1998;206(1):137–42.
Fu CY, Wu SC, Chen RJ, et al. Evaluation of need for operative intervention in blunt splenic injury: intraperitoneal contrast extravasation has an increased probability of requiring operative intervention. World J Surg. 2010;34(11):2745–51.
Omert LA, Salyer D, Dunham CM, et al. Implications of the “contrast blush” finding on computed tomographic scan of the spleen in trauma. J Trauma. 2001;51(2):272–7 (discussion 277–8).
Davis KA, Fabian TC, Croce MA, et al. Improved success in nonoperative management of blunt splenic injuries: embolization of splenic artery pseudoaneurysms. J Trauma. 1998;44(6):1008–13 (discussion 1013–5).
Harbrecht BG, Ko SH, Watson GA, et al. Angiography for blunt splenic trauma does not improve the success rate of nonoperative management. J Trauma. 2007;63(1):44–9.
Dehqanzada ZA, Meisinger Q, Doucet J, et al. Complete ultrasonography of trauma in screening blunt abdominal trauma patients is equivalent to computed tomographic scanning while reducing radiation exposure and cost. J Trauma Acute Care Surg. 2015;79(2):199–205.
Mebert RV, Schnuriger B, Candinas D, Haltmeier T. Follow-up imaging in patients with blunt splenic or hepatic injury managed nonoperatively. Am Surg. 2018;84(2):208–14.
Funding
None for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Brenner is on the clinical advisory board of Prytime Medical Inc.
Rights and permissions
About this article
Cite this article
Lauerman, M., Brenner, M., Simpson, N. et al. Extra-parenchymal splenic abnormalities not vascular injury predict need for primary splenectomy. Eur J Trauma Emerg Surg 46, 1063–1069 (2020). https://doi.org/10.1007/s00068-019-01085-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01085-6