Abstract
Purpose
Serious thoracic injuries are associated with high mortality, morbidity, and costs. We compared patient populations, treatment, and survival of serious thoracic injuries in southern Finland and Germany.
Methods
Mortality, patient characteristics and treatment modalities were compared over time (2006–2015) in all patients with Abbreviated Injury Scale (AIS) thorax ≥ 3, Injury Severity Score (ISS) > 15, age > 15 years, blunt trauma mechanism, and treatment in Intensive Care Unit (ICU) in Level 1 hospitals included in the Helsinki Trauma Registry (HTR) and the TraumaRegister DGU® (TR-DGU).
Results
We included 934 patients from HTR and 25 448 patients from TR-DGU. Pre-hospital differences were seen between HTR and TR-DGU; transportation in the presence of a physician in 61% vs. 97%, helicopter use in 2% vs. 42%, intubation in 31% vs. 55%, and thoracostomy in 6% vs. 10% of cases, respectively. The mean hospital length of stay (LOS) and ICU LOS was shorter in HTR vs. TR-DGU (13 vs. 25 days and 9 vs. 12 days, respectively). Our main outcome measure, standardised mortality ratio, was not statistically significantly different [1.01, 95% confidence interval (CI) 0.84–1.18; HTR and 0.97, 95% CI 0.94–1.00; TR-DGU].
Conclusions
Major differences were seen in pre-hospital resources and use of pre-hospital intubation and thoracostomy. In Germany, pre-hospital intubation, tube thoracostomy, and on-scene physicians were more prevalent, while patients stayed longer in ICU and in hospital compared to Finland. Despite these differences in resources and treatment modalities, the standardised mortality of these patients was not statistically different.
Similar content being viewed by others
Introduction
Blunt thoracic injuries can cause severe morbidity and mortality [1,2,3]. Most patients with serious thoracic injuries are treated in intensive care units (ICU) and the length of stay (LOS) in hospital is often long. These patients are a heterogeneous group with whom it is difficult to compare different treatment options or perform randomised controlled studies [4].
A previous trauma registry comparison of severely injured patients (including all injuries in different body regions) between southern Finland and Germany [5] showed distinct differences in outcome in patients with severe traumatic brain injury. Because of this finding, another comparison was performed to determine the possible reasons for that particular difference [6]. After this analysis, it was feasible to also look closely at other injuries to determine whether differences exist in, e.g., patients with severe thoracic injuries if isolated from all other severely injured patients. This would also be a way to benchmark the treatment of patients with severe thoracic injuries in the Helsinki Trauma Registry (HTR). The study by Brinck in 2015 [5] revealed thoracic injuries to be common in both Finnish and German trauma registries; 47% of Finnish patients and 58% of German patients had at least a moderate chest injury (Abbreviated Injury Scale Thorax (AISTHORAX) ≥ 2). The basic profile and characteristics of all trauma patients were quite similar between the registries. There were also interesting differences in resourcing the patient care; a pre-hospital physician was on scene almost every time, a helicopter was used to transport patients more often, and the intubation rate was higher in Germany. ICU treatment time, ventilation time, and total hospital LOS were also longer in Germany.
The aim of this study was to evaluate if there are also differences in resource allocations, as presented above, in this subgroup of patients with serious thoracic injuries (AISTHORAX ≥3) and if so, to determine if these differences affect the outcome of these patients. Our hypothesis was that the outcome would be similar between the two countries, even though more resources are available to treat seriously injured patients in Germany.
Materials and methods
Trauma registries
The HTR is the trauma registry of the Helsinki University Hospital Trauma Unit. There is no national trauma registry in Finland. The HTR was established in 2006 and now includes all New Injury Severity Score (NISS) > 15 trauma patients admitted to the resuscitation bay (until the end of 2011, the inclusion criterion was Injury Severity Score [ISS] > 15 instead of NISS).
Since 2012, HTR data have been sent annually to Germany to be included in to the TraumaRegister DGU® (TR-DGU) for data comparison and completeness analysis. Both data coverage and accuracy of the HTR have been found to be excellent [7].
The TR-DGU was founded in 1993 and is run by the AUC—Academy for Trauma Surgery (AUC—Akademie der Unfallchirurgie GmbH), a company affiliated to the German Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU). The aim of this multi-center database is a pseudonymised and standardised documentation of severely injured patients. The inclusion criterion is patient admission to hospital via emergency room with subsequent ICU care or if the patient reaches the hospital with vital signs and die before admission to ICU.
The participating hospitals submit their data pseudonymised into a central database via a web-based application. The participating hospitals are primarily located in Germany (90%), but an increasing number of hospitals from other countries contribute data as well (currently Austria, Belgium, China, Finland, Luxembourg, Slovenia, Switzerland, The Netherlands, and the United Arab Emirates). Approximately 30 000 cases from more than 600 hospitals are currently entered into the database per year.
Participation in the TraumaRegister DGU® is voluntary. For hospitals associated with the TraumaRegister DGU®, however, the entry of at least a basic data set is obligatory for reasons of quality assurance. The number of participating hospitals is increasing every year; at the end of 2016, there were 645 hospitals sending in data.
Trauma systems in Finland and Germany
Treatment of serious blunt injuries in southern Finland is centralised to the Helsinki University Hospital Trauma Unit. The Helsinki University Hospital (HUH) is a tertiary trauma centre with a catchment area of about 1.8 million. The trauma unit annually treats about 400 ISS > 15 patients. In Finland, seriously injured patients are treated in publicly financed, community-owned hospitals only. Pre-hospital treatment is usually given first by paramedics. In serious cases, there is either an emergency medical service (EMS) physician or a helicopter emergency medical services (HEMS) physician available. The physicians in pre-hospital work are mainly anaesthesiologists specialised in emergency care.
The health-care system in Germany is somewhat different than in Finland. There are two main types of health insurance, namely, statutory health insurance and private health insurance [8]. Acute care is provided in public hospitals (approximately 50% of acute care hospital beds), private not-for-profit hospitals (40%), and private for-profit hospitals (10%). In Germany, physician-operated emergency medical services manage nearly all traumas in the pre-hospital setting. The use of rescue helicopters is also very common [9]. Most pre-hospital physicians are anaesthesiologists and trauma surgeons and all are required to have had post-graduate emergency medicine training [10].
Comparison and outcome measures
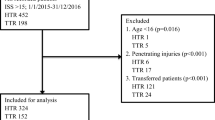
Prospectively collected data from the HTR were retrospectively compared to similar data from the TR-DGU. The study period was 1.1.2006–31.12.2015. We used the same inclusion criteria for both registries, namely, all patients receiving ICU treatment with serious thoracic injury (AISTHORAX ≥3), ISS > 15, age > 15 years, and blunt trauma mechanism treated within 24 h of the initial trauma in reporting hospital were included. From the final outcome analysis, we excluded all patients that were transferred in from another hospital or transferred out soon after arrival to the emergency department due to missing data needed for the Revised Injury Severity Classification II (RISC II) calculations [11].
For this comparison, from the TR-DGU database, we included only German Level 1 trauma hospitals with data from a minimum of 6 consecutive years (102 hospitals met the criteria).
Both trauma registries (HTR and TR-DGU) collect the data prospectively at the following four consecutive time phases from the site of the accident until discharge from hospital: (a) pre-hospital phase; (b) emergency room and initial surgery; (c) ICU; and (d) discharge. The documentation includes detailed information on demographics, injury pattern, co-morbidities, pre-hospital and in-hospital management, course in ICU, relevant laboratory findings (including transfusion data), and outcome of each individual.
We compared age, gender, ISS, NISS, mechanism of injury, injury distribution (injuries that had AIS score ≥ 2), pre-hospital times, intubation rates, tube thoracostomy frequency, transport methods, ICU LOS, ventilation days, total hospital LOS, discharge destination, and in-hospital mortality. Our main outcome measure was the standardised mortality ratio (SMR), which was calculated by dividing observed mortality by expected mortality. The expected mortality was calculated using RISC II, which is a second version of a prognostic score developed originally from TR-DGU data [11]. If the SMR value is < 1, then the outcome defined by in-hospital mortality is better than expected by the RISC II score.
We also compared changes in patient population and treatment methods during the study period.
Statistics
All comparisons were calculated using only the information available; no imputations were done.
For descriptive analysis, we used mean, median, and standard deviation (SD) for metric variables and percentages for categorical variables.
Outcome (mortality) was compared to the prognosis derived from the RISC II score. The relationship between observed-to-expected ratios was calculated as SMR, and a 95% confidence interval (CI) was derived using the respective interval for the observed mortality. Comparison and statistical analysis were performed with the Statistical Package for the Social Sciences (SPSS, version 23, IBM Inc., Armonk NY, USA).
Ethical standards statement
The review board of the Helsinki University Hospital approved this study. The study was also registered and approved according to the publication guideline of the TR-DGU (Project ID: 2015-039).
Results
Patients
We included 934 patients from the HTR (data from 1 hospital) and 25 448 patients from the TR-DGU (data from 102 hospitals) for comparison. The study flowchart is shown in Fig. 1. Patient characteristics are shown in Table 1. The mean age of patients with serious thoracic injuries increased in both registries during the study period. Compared with HTR, the patients in TR-DGU were older at the time of injury, particularly towards the end of the study period.
Mechanism of injury (MOI) and injury distribution
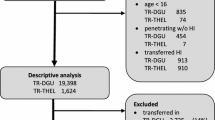
[Descriptive analysis: TR-DGU 25,448 patients (pts.), HTR 934 pts.]
The profile of the mechanism of injury (MOI) was similar between southern Finland and Germany. However, some differences were also observed. There were fewer traffic-related injuries in HTR (58%) than in TR-DGU (64%). High fall was the leading MOI in HTR, while the leading MOI in TR-DGU was car accident. A more detailed description of MOIs is shown in Table 2.
In HTR, there were more injuries in the abdomen, spine, and pelvis: there were more head injuries in TR-DGU. A detailed distribution of injuries in different body regions is shown in Fig. 2.
The most common thorax injuries in both registries are shown in Table 3.
Pre-hospital treatment
(First outcome analysis: TR-DGU 22,576 pts., HTR 781 pts.)
For analysis of pre-hospital treatment, we included only primary admitted cases due to missing data on patients transferred in from another hospital. The total pre-hospital time (time from dispatch to hospital) was almost equal in both registries (HTR, mean 71 min; TR-DGU, mean 70 min). On-scene time was also similar in both registries (HTR, mean 32 min; TR-DGU, mean 33 min). A physician was on scene in 61% (HTR) and in 97% of cases in TR-DGU. Pre-hospital intubation was considerably less frequent in HTR (31%) than in TR-DGU (55%). For unconscious patients [Glasgow Coma Scale (GCS) 3–8], the difference was smaller (HTR, 88%; TR-DGU, 95%). When focusing on the last 3 years in HTR, the intubation frequency for unconscious patients rose to 97%. Thoracostomy was also performed less frequently in southern Finland than in Germany. Details of pre-hospital times, transportation methods, and intubation and thoracostomy frequency are shown in Table 4.
Treatment in hospital
(First outcome analysis: TR-DGU 22,576 pts., HTR 781 pts.)
Primary admitted patients were intubated less frequently during emergency room (ER) treatment in HTR than in TR-DGU (Table 5).
Total LOS, ICU LOS, and ventilation days are shown in Table 6. The mean length of both ICU treatment and hospital treatment was shorter in HTR than in TR-DGU (9 days vs. 13 days and 14 days vs. 25 days, respectively). The ventilation duration was on average 3 days shorter in Finland (HTR, 8 days; TR-DGU, 11 days); the median was the same in both registries (6 days; Table 6). Fewer patients were discharged home or to a rehabilitation facility in HTR (21%) than in TR-DGU (69%). In HTR, 57% of patients were discharged to a step-down hospital but only 11% in TR-DGU.
Depending on the discharge destination in German hospitals, the LOS was shortest (mean 23 days) when discharged to another hospital and longest (mean 35 days) when discharged to a rehabilitation centre. In HTR, the shortest LOS was 12 days when discharged home and longest (mean 38 days) when discharged to a rehabilitation centre (all of these 25 patients had a spinal cord injury and were sent to a special centre for spinal cord injury rehabilitation). Detailed information on the correlation between LOS and discharge destination is shown in Table 7.
In-hospital mortality and RISC II analysis
(Final outcome analysis: RISC II. TR-DGU 22,418 pts., HTR 759 pts.)
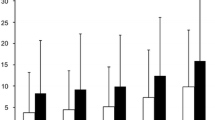
The observed in-hospital mortality was 14.8% (HTR) and 18.5% (TR-DGU). The expected mortality was 14.6% (HTR) and 19.1% (TR-DGU) (Fig. 3).
The SMR was comparable in both registries (HTR, 1.01, 95% CI 0.84–1.18; TR-DGU, 0.97 95% CI 0.94–1.00).
Discussion
In this study, we showed that the profile of patients (age, gender, NISS, and ISS) with serious thoracic injury was nearly similar in southern Finland (HTR) and in German (TR-DGU) registries. However, in Germany, more resources were utilised for treatment, namely, nearly twice as many pre-hospital intubations and thoracostomies. In addition, emergency physicians accompanied patients to hospital in 97% of cases in Germany compared to 61% in southern Finland. Helicopters were used 22 times more often in Germany. Of note, both intensive care and primary hospital LOS were notably longer in Germany than in southern Finland. Despite these differences in treatment, SMR was not statistically significantly different (HTR, 1.01; TR-DGU, 0.97).
Trauma registries are an important data source in evaluating severe injuries and those seriously injured. These data can also be used to compare different treatment options within one hospital over time, between one hospital and another or even between different countries and trauma systems [5, 6, 12,13,14]. International comparison is possible if the collected data are similar or can be adjusted [15, 16]. An international trauma registry comparison provides more options than comparing the results only within a national system. Accordingly, quality control and registry comparisons should be an integral part of trauma patient treatment in modern trauma hospital organisations [6]. Although HTR data came from one large trauma center and TR-DGU data for this comparison came from 102 Level 1 hospitals (that are mostly smaller), the patients were comparable as shown in a previous study [5]. In that study, patient age was similar between the two registries as was the percentage of patients over 60 years of age. This is not the case in patients with severe thoracic injury; HTR patients are on average 5 years younger than in TR-DGU and the proportion of patients over 60 years of age is greater in TR-DGU (24% in HTR vs. 30% in TR-DGU).
There were more pre-injury ASA 3 or 4 patients among TR-DGU patients than in HTR. This could be associated with the fact that patients were older in the TR-DGU database and, therefore, were more likely to have more co-morbidities than the younger patients in HTR.
The intubation rate was different between the registries. The overall intubation frequency was twice as high in TR-DGU as in HTR. When dividing the results between the patients with GCS 9–15 and GCS 3–8, we could determine where the difference mostly came from; in the first group, the intubation frequency was almost six times higher in TR-DGU, but in unconscious patients, the frequencies were much closer. In HTR data, the intubation frequency in unconscious patients rose towards the end of the study period; in the last 3 years the frequency was 97%, which is a result of system improvements and improved following of guidelines. It has been shown that the intubation success rate among paramedics can be relatively low [17]. In HTR, no patient with GCS 9–15 was intubated by paramedics; in TR-DGU, 7.3% of the patients were. We could argue that this is potentially harmful for patients if performed only ‘just in case’. The reason for the high overall intubation rates in the German data can be explained at least partly by the transportation method. Since more than 40% of patients are transported by helicopter, it might be reasonable to intubate all those in need and also all those that might need intubation during transportation, as this procedure is quite difficult or even impossible to perform in a flying helicopter. We could also argue that patients in Germany are more likely to be intubated, because they are older and have more head injuries. There could be a difference in local intubation protocols between different paramedics and hospital regions.
In the German data, thoracostomy was performed almost twice as often in the pre-hospital setting when counting all patients (TR-DGU, 10%; HTR 6%). However, when considering the cases, where a physician was on scene, the frequency in HTR rose to 8%. The difference in thoracostomy (performed either in a pre-hospital setting or ER) frequency disappeared when patients that received thoracostomy in ER were taken into account (TR-DGU, 27%; HTR, 38%).
Another major difference was noted in hospital LOS and ICU LOS. In Germany, patients were treated nearly double the time in the primary treating hospital than in southern Finland. The reason for this is multifactorial and described in more detail in the article by Brinck et al. In brief, the reasons are local policy in Finland to transfer patients to a step-down hospital, as early as medically possible, and in Germany, there is usually a well-developed rehabilitation system within the admitting hospital [5]. A new finding in the current study was that regardless of the discharge destination, German hospitals keep these patients on average at least 23 days in the admitting hospital. In southern Finland, the shortest LOS was 12 days for those who were discharged home (in Germany those patients discharged home spent nearly 24 days in hospital). In addition, the 10% of patients, which in Germany are transported to another hospital after primary treatment, spent 23 days in the admitting hospital. In southern Finland, the patients (57%) that go to another hospital spent only 15 days in the admitting hospital.
The mean ICU LOS difference was 4 days (HTR, 9 days; TR-DGU, 13 days). However, when considering median values, the difference was only 2 days (6 days vs. 8 days). The same was noted in ventilation days (mean 8 days vs. 11 days); the median was the same (6 days). We can, therefore, say that in German hospitals, patients are treated longer both in ICU and on ventilator. The cause for ICU LOS difference might be the difference in the size of the hospitals. Helsinki University Hospital Trauma Unit is treating more than 300 patients with ISS over 15 per year, but only a handful of hospitals in Germany was the same size. Therefore, the experience in ICU might be different with trauma patients, especially with severe thoracic injury. In addition, in Helsinki, we lack the ICU beds most of the time, so we need to transfer the patients to the normal ward as soon as possible, and this might not be the case in all German hospitals.
The observed mortality in Germany (18.5%) was higher than in southern Finland (14.8%). This can be explained by differences in age, ASA classification, and the number of head injuries (all of these parameters were higher in Germany). The expected mortality by RISC II was also higher in Germany; the explanation is the same as mentioned above.
The most interesting finding was that even though in Germany, patients are treated more actively both in the pre-hospital phase and the in-hospital phase and stayed for a longer time in hospital, the SMR results are not really better than in southern Finland, where patients are treated more conservatively in the pre-hospital phase and spent less time in the ICU and in hospital overall.
In both registries, the SMR was almost equal to one, which suggests good treatment both in pre-hospital care and in in-hospital care. This study shows that despite large differences in resource allocation between German and southern Finland trauma systems, there is no statistical difference in results when considering SMR as main outcome measure. Therefore, the German system could be considered as less cost effective. In Finland, the public health-care system is also ‘fighting’ for more resources from government, but in Germany, it could be that insurance companies regulate hospital economy.
To our knowledge, there are no previous reports of resource allocation affecting the outcome of patients with serious thoracic injuries.
The strength of this study is the large number of patients in both registries. A similar comparison has been done before and has also been found to be feasible [5]. The limitations of such a comparison are known from a previous study [6] and have been acknowledged. The study period consisted of 10 years and both registries are accurate and have good data coverage [7, 18].
The study has some limitations.
First, this was a retrospective register study and we did not follow up the patients after discharge. We are thus unaware of any deaths occurring after discharge. There may be some differences in mortality explained by the fact that in Finland, patients leave the hospital on average on day 14 and in Germany on day 25. There could be bias in mortality, since patients’ deaths after discharge from the admitting hospital are not recorded. We know from the previous TR-DGU and TARN (Trauma Audit and Research Network, UK) data that approximately 18% of trauma deaths occur between days 7 and 30 and 4% after day 30 [19]. This means that possibly, more deaths are not recorded in the HTR, because patients are discharged 11 days earlier than in TR-DGU.
Second, most of the Level 1 hospitals in Germany are smaller than the Helsinki University Hospital and treat on average 57 (median 51) seriously injured patients (defined by ISS > 15) per year. This might influence the hospitals’ treatment protocols and could lead to, e.g., prolonged treatment.
Third, the data collection method is different in these compared registries, but we could carefully transform the data into properly comparable variables. This set of data was used for the analysis.
Descriptive analysis was performed using mean, median, and SD for metric variables and percentages for categorical variables. The additional median value allows estimating the skewness of the distribution. Formal statistical testing was avoided here, since the sample size was rather large. In such a case, clinically relevant differences will also be statistically significant. On the other hand, with large samples, even minor differences could become statistically significant and may lead to misinterpretations. The actual sample size of 1000 vs. 25 000 cases would allow detecting differences of 2–3% (for categorical variables) or the tenth part of a SD (for continuous variables).
Our main outcome was in-hospital mortality and especially the SMR. Results could have been different if the outcome had been quality of life.
In the present study, we compared the care of patients with serious thoracic injuries between the TR-DGU and the HTR. We discovered some major differences that would not have been discovered with any other research method. These differences should be taken into consideration both in Germany and Finland. There might be ways to make treatments better and more efficient in both countries. We will continue to evaluate these data also among different subgroups of patients to determine if similar differences exist.
Conclusions
In Germany, patients with serious thoracic injuries are treated with more resources than in southern Finland, but our results suggest that it is possible to achieve nearly as good results with fewer resources. In southern Finland, the way of treating similar patients with fewer pre-hospital and in-hospital resources yields a good adjusted outcome when measured by SMR. Further studies are needed to evaluate whether the quality of life is also similar with these differences in resource allocation when treating severely injured patients.
References
Huber S, Biberthaler P, Delhey P, et al. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU). Scand J Trauma Resusc Emerg Med. 2014;22:52.
Soderlund T, Ikonen A, Pyhalto T, Handolin L. Factors associated with in-hospital outcomes in 594 consecutive patients suffering from severe blunt chest trauma. Scand.J.Surg. 2015;104:115–20.
Bayer J, Lefering R, Reinhardt S, et al., Thoracic trauma severity contributes to differences in intensive care therapy and mortality of severely injured patients: analysis based on the TraumaRegister DGU. World J.Emerg.Surg. 2017;12:43.
Lefering R. Using data from registries like the TraumaRegister DGU® for effectiveness evaluations. Z. Evid Fortbild. Qual Gesundh wes. 2016;112:11-5.
Brinck T, Handolin L, Paffrath T, Lefering R. Trauma registry comparison: six-year results in trauma care in Southern Finland and Germany. Eur J Trauma Emerg Surg 2015;41:509–16.
Brinck T, Raj R, Skrifvars MB, et al., Unconscious trauma patients: outcome differences between southern Finland and Germany-lesson learned from trauma-registry comparisons. Eur J Trauma Emerg Surg. 2016;42:445–51.
Heinänen M, Brinck T, Handolin L, et al., Accuracy and coverage of diagnosis and procedural coding of severely injured patients in the Finnish Hospital discharge register: Comparison to patient files and the Helsinki trauma Registry. Scand J Surg. 2017;106:269–77.
Worz M, Busse R. Analysing the impact of health-care system change in the EU member states–Germany. Health Econ. 2005;14:133-49.
Andruszkow H, Hildebrand F, Lefering R, et al. Ten years of helicopter emergency medical services in Germany: do we still need the helicopter rescue in multiple traumatised patients? Injury. 2014;45:53-8.
Westhoff J, Hildebrand F, Grotz M, et al., Trauma care in Germany. Injury 2003;34:674–83.
Lefering R, Huber-Wagner S, Nienaber U, et al. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: the Revised Injury Severity Classification, version II. Crit Care. 2014;18:476.
Moore L, Clark DE. The value of trauma registries. Injury 2008; 39:686–95.
Engel DC, Mikocka-Walus A, Cameron PA, Maegele M. Pre-hospital and in-hospital parameters and outcomes in patients with traumatic brain injury: a comparison between German and Australian trauma registries. Injury. 2010;41:901–6.
Lefering R, Ruchholtz S. Trauma registries in Europe. Eur J Trauma Emerg Surg. 2012;38:1–2.
Ringdal KG, Coats TJ, Lefering R, et al. The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16:7.
Ringdal KG, Lossius HM, Jones JM, et al. Collecting core data in severely injured patients using a consensus trauma template: an international multicentre study. Crit Care. 2011;15:R237.
Raatiniemi L, Lankimaki S, Martikainen M. Pre-hospital airway management by non-physicians in Northern Finland—a cross-sectional survey. Acta Anaesthesiol Scand. 2013;57:654–9.
Lefering R, Waydhas C, Huber-Wagner S, Nienaber U, TraumaRegister DGUR Annual Report 2017
Lefering R, Paffrath T, Bouamra O, et al. Epidemiology of in-hospital trauma deaths. Eurjtraumaemergsurg. 2012;38:3–9.
Acknowledgements
We thank Satu Tirkkonen, Pirkko Tonder, Markku Kytönen, Iiu Laitinen and Marja Bergman for excellent work in accurately recording the data for the Helsinki Trauma Registry. We also thank Kirsi Willa for managing the data bank of the Helsinki Trauma Registry. We thank DGU for the possibility to perform this comparison.
Author information
Authors and Affiliations
Contributions
MH: design of study, interpretation of data, and writing the manuscript. TB and LH: design of study, interpretation of data, and critical revision of manuscript. RL: design of study, statistics, interpretation of data, and critical revision of manuscript. TS: design of study, interpretation of data, critical revision of manuscript, and supervision of study. All authors read and accepted the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Mikko Heinänen, Tuomas Brinck, Rolf Lefering, Lauri Handolin, and Tim Söderlund declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Heinänen, M., Brinck, T., Lefering, R. et al. Resource use and clinical outcomes in blunt thoracic injury: a 10-year trauma registry comparison between southern Finland and Germany. Eur J Trauma Emerg Surg 45, 585–595 (2019). https://doi.org/10.1007/s00068-018-1004-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-1004-x