Abstract
Aim
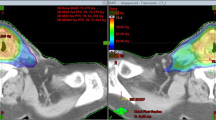
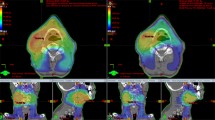
To compare simultaneous integrated boost plans for intensity-modulated proton therapy (IMPT), helical tomotherapy (HT), and RapidArc therapy (RA) for patients with head and neck cancer.
Patients and methods
A total of 20 patients with squamous cell carcinoma of the head and neck received definitive chemoradiation with bilateral (n = 14) or unilateral (n = 6) neck irradiation and were planned using IMPT, HT, and RA with 54.4, 60.8, and 70.4 GyE/Gy in 32 fractions. Dose distributions, coverage, conformity, homogeneity to planning target volumes (PTV)s and sparing of organs at risk and normal tissue were compared.
Results
All unilateral and bilateral plans showed excellent PTV coverage and acceptable dose conformity. For unilateral treatment, IMPT delivered substantially lower mean doses to contralateral salivary glands (< 0.001–1.1 Gy) than both rotational techniques did (parotid gland: 6–10 Gy; submandibular gland: 15–20 Gy). Regarding the sparing of classical organs at risk for bilateral treatment, IMPT and HT were similarly excellent and RA was satisfactory.
Conclusion
For unilateral neck irradiation, IMPT may minimize the dry mouth risk in this subgroup but showed no advantage over HT for bilateral neck treatment regarding classical organ–at-risk sparing. All methods satisfied modern standards regarding toxicity and excellent target coverage for unilateral and bilateral treatment of head and neck cancer at the planning level.
Zusammenfassung
Hintergrund
Planvergleich von intensitätsmodulierter Protonentherapie (IMPT), Tomotherapie (HT) und RapidArc-Therapie (RA) für Patienten mit Plattenepithelkarzinomen der Kopf-Hals-Region unter Anwendung des simultan integrierten Boost-Konzepts (SIB).
Patienten und Methodik
Für 20 Patienten mit Plattenepithelkarzinomen der Kopf-Hals-Region und bilateraler (n = 14) oder unilateraler (n = 6) zervikaler primärer Radiochemotherapie erfolgte eine IMPT-, HT- und RA-Planung mit 54,4, 60,8 und 70,4 GyE/Gy in 32 Fraktionen. Die Dosisverteilung, Abdeckung, Konformität und Homogenität der PTVs sowie die Risikoorgan- und Normalgewebeschonung wurden verglichen.
Ergebnisse
Alle uni- und bilateralen Pläne zeigten eine exzellente PTV-Abdeckung bei akzeptabler Konformität. IMPT erreichte in der unilateralen Bestrahlungssituation eine wesentlich geringere mittlere Dosis an den kontralateralen Speicheldrüsen (< 0,001–1,1 Gy) als beide Photonentechniken (Glandula parotidea: 6–10 Gy; Glandula submandibularis: 15–20 Gy). In der bilateralen Behandlungssituation scheint die IMPT im Vergleich zur HT keine Vorteile für die klassische Risikoorganschonung zu haben. RA erreichte eine zufriedenstellend gute Risikoorganschonung.
Schlussfolgerung
Durch IMPT konnte in der Patientensubgruppe mit unilateraler Bestrahlung das potentielle Risiko für eine permanente Xerostomie wesentlich reduziert werden. Bei bilateraler Bestrahlung erscheint die Schonung von klassischen Risikoorganen durch die HT vergleichbar gut. Alle untersuchten Bestrahlungsmethoden konnten sowohl für die unilaterale als auch die bilaterale Bestrahlung von Patienten mit Kopf-Hals-Tumoren moderne Bestrahlungsplanungsvorgaben im Sinne einer Limitierung von Nebenwirkungen bei gleichzeitig exzellenter Zielvolumenabdeckung erreichen.

Similar content being viewed by others
References
Blanchard P, Baujat B, Holostenco V et al (2011) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): a comprehensive analysis by tumour site. Radiother Oncol 100:33–40
Eisbruch A, Ten Haken RK, Kim HM et al (1999) Dose, volume, and function relationships in parotid salivary glands following conformal and intensity-modulated irradiation of head and neck cancer. Int J Radiat Oncol Biol Phys 45:577–587
Eisbruch A, Kim HM, Terrell JE et al (2001) Xerostomia and its predictors following parotid-sparing irradiation of head-and-neck cancer. Int J Radiat Oncol Biol Phys 50:695–704
Maes A, Weltens C, Flamen P et al (2002) Preservation of parotid function with uncomplicated conformal radiotherapy. Radiother Oncol 63:203–211
Dijkema T, Raaijmakers CP, Ten Haken RK et al (2010) Parotid gland function after radiotherapy: the combined michigan and utrecht experience. Int J Radiat Oncol Biol Phys 78:449–453
Tribius S, Sommer J, Prosch C et al (2013) Xerostomia after radiotherapy. What matters–mean total dose or dose to each parotid gland? Strahlenther Onkol 189:216–222
Levendag PC, Teguh DN, Voet P et al (2007) Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiation therapy dose to the superior and middle constrictor muscle: a dose-effect relationship. Radiother Oncol 85:64–73
Eisbruch A, Schwartz M, Rasch C et al (2004) Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys 60:1425–1439
Laurell G, Kraepelien T, Mavroidis P et al (2003) Stricture of the proximal esophagus in head and neck carcinoma patients after radiotherapy. Cancer 97:1693–1700
Rancati T, Schwarz M, Allen AM et al (2010) Radiation dose-volume effects in the larynx and pharynx. Int J Radiat Oncol Biol Phys 76:64–69
Teh BS, Woo SY, Butler EB (1999) Intensity modulated radiation therapy (IMRT): a new promising technology in radiation oncology. Oncologist 4:433–442
Mohan R, Wu Q, Manning M et al (2000) Radiobiological considerations in the design of fractionation strategies for intensity-modulated radiation therapy of head and neck cancers. Int J Radiat Oncol Biol Phys 46:619–630
Stromberger C, Ghadjar P, Marnitz S et al (2015) Comparative treatment planning study on sequential vs. simultaneous integrated boost in head and neck cancer patients: Differences in dose distributions and potential implications for clinical practice. Strahlenther Onkol
Dandekar V, Morgan T, Turian J et al (2014) Patterns-of-failure after helical tomotherapy-based chemoradiotherapy for head and neck cancer: implications for CTV margin, elective nodal dose and bilateral parotid sparing. Oral Oncol 50:520–526
Lauve A, Morris M, Schmidt-Ullrich R et al (2004) Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas: II–clinical results. Int J Radiat Oncol Biol Phys 60:374–387
Leclerc M, Maingon P, Hamoir M et al (2013) A dose escalation study with intensity modulated radiation therapy (IMRT) in T2N0, T2N1, T3N0 squamous cell carcinomas (SCC) of the oropharynx, larynx and hypopharynx using a simultaneous integrated boost (SIB) approach. Radiother Oncol 106:333–340
Chen AM, Daly ME, Cui J et al (2014) Helical tomotherapy with simultaneous integrated boost dose painting for the treatment of synchronous primary cancers involving the head and neck. Br J Radiol 87:20130697
Thomson DJ, Ho KF, Ashcroft L et al (2015) Dose intensified hypofractionated intensity-modulated radiotherapy with synchronous cetuximab for intermediate stage head and neck squamous cell carcinoma. Acta Oncol 54:88–98
Scorsetti M, Fogliata A, Castiglioni S et al (2010) Early clinical experience with volumetric modulated arc therapy in head and neck cancer patients. Radiat Oncol 5:93
Alongi F, Bignardi M, Garassino I et al (2012) Prospective phase II trial of cetuximab plus VMAT-SIB in locally advanced head and neck squamous cell carcinoma. Feasibility and tolerability in elderly and chemotherapy-ineligible patients. Strahlenther Onkol 188:49–55
Gomez-Millan Barrachina J, Jerez Sainz I, Perez Rozos A et al (2015) Potential advantages of volumetric arc therapy in head and neck cancer. Head Neck 37:909–914
Smet S, Lambrecht M, Vanstraelen B et al (2015) Clinical and dosimetric evaluation of RapidArc versus standard sliding window IMRT in the treatment of head and neck cancer. Strahlenther Onkol 191:43–50
Cozzi L, Bolsi A, Nicolini G et al (2004) The simultaneous integrated boost with proton beams in head and neck patients. Z Med Phys 14:180–188
Slater JD, Yonemoto LT, Mantik DW et al (2005) Proton radiation for treatment of cancer of the oropharynx: early experience at Loma Linda University Medical Center using a concomitant boost technique. Int J Radiat Oncol Biol Phys 62:494–500
Frank SJ, Cox JD, Gillin M et al (2014) Multifield optimization intensity modulated proton therapy for head and neck tumors: a translation to practice. Int J Radiat Oncol Biol Phys 89:846–853
van de Water TA, Lomax AJ, Bijl HP et al (2011) Potential benefits of scanned intensity-modulated proton therapy versus advanced photon therapy with regard to sparing of the salivary glands in oropharyngeal cancer. Int J Radiat Oncol Biol Phys 79:1216–1224
Jakobi A, Bandurska-Luque A, Stutzer K et al (2015) Identification of patient benefit from proton therapy for advanced head and neck cancer patients based on individual and subgroup normal tissue complication probability analysis. Int J Radiat Oncol Biol Phys 92:1165–1174
Stromberger C, Wlodarczyk W, Marnitz S et al (2015) Simultaneous Integrated Boost (SIB): rapidArc and tomotherapy plan comparison for unilateral and bilateral neck irradiation. Anticancer Res 35:2991–2997
Gregoire V, Levendag P, Ang KK et al (2003) CT-based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC, RTOG consensus guidelines. Radiother Oncol 69:227–236
Gillin MT, Sahoo N, Bues M et al (2010) Commissioning of the discrete spot scanning proton beam delivery system at the University of Texas M.D. Anderson Cancer Center, Proton Therapy Center, Houston. Med Phys 37:154–163
Otto K (2008) Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys 35:310–317
Feuvret L, Noel G, Mazeron JJ et al (2006) Conformity index: a review. Int J Radiat Oncol Biol Phys 64:333–342
Tribius S, Raguse M, Voigt C et al (2015) Residual deficits in quality of life one year after intensity-modulated radiotherapy for patients with locally advanced head and neck cancer: results of a prospective study. Strahlenther Onkol 191:501–510
Greco C, Wolden S (2007) Current status of radiotherapy with proton and light ion beams. Cancer 109:1227–1238
Liu W, Frank SJ, Li X et al (2013) Effectiveness of robust optimization in intensity-modulated proton therapy planning for head and neck cancers. Med Phys 40:051711
Muller BS, Duma MN, Kampfer S et al (2015) Impact of interfractional changes in head and neck cancer patients on the delivered dose in intensity modulated radiotherapy with protons and photons. Phys Med 31:266–272
Kraan AC, van de Water S, Teguh DN et al (2013) Dose uncertainties in IMPT for oropharyngeal cancer in the presence of anatomical, range, and setup errors. Int J Radiat Oncol Biol Phys 87:888–896
Gora J, Kuess P, Stock M et al (2015) ART for head and neck patients: On the difference between VMAT and IMPT. Acta Oncol 54:1166–1174
van der Laan HP, van de Water TA, van Herpt HE et al (2013) The potential of intensity-modulated proton radiotherapy to reduce swallowing dysfunction in the treatment of head and neck cancer: a planning comparative study. Acta Oncol 52:561–569
Langendijk JA, Lambin P, De Ruysscher D et al (2013) Selection of patients for radiotherapy with protons aiming at reduction of side effects: the model-based approach. Radiother Oncol 107:267–273
Acknowledgments
No source of funding supported this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Cozzi acts as Scientific Advisor to Varian Medical Systems and is Clinical Research Scientist at Humanitas Cancer Center. C. Stromberger, V. Budach, A. Fogliata, P. Ghadjar, W. Wlodarczyk, B. Jamil, J.D. Raguse, A. Böttcher and S. Marnitz state that there are no conflicts of interest.
This study was approved by the Institutional Review Board of the Charité Universitätsmedizin Berlin.
Rights and permissions
About this article
Cite this article
Stromberger, C., Cozzi, L., Budach, V. et al. Unilateral and bilateral neck SIB for head and neck cancer patients. Strahlenther Onkol 192, 232–239 (2016). https://doi.org/10.1007/s00066-016-0945-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-0945-4