Abstract
Purpose
To assess the benefit of 4D-CT angiography (4D-CTA) in determination and precise measurement of middle cerebral artery (MCA) occlusion in comparison to CTA. Possible relationship of measured occlusion lengths with recanalization after intravenous thrombolysis was analysed as a second objective.
Methods
Detailed evaluation of complete MCA occlusions in 80 patients before intravenous thrombolysis using temporal maximum intensity projection (tMIP) dataset, calculated from 4D-CTA and conventional single-phase CTA was performed. Further, manual measurement technique was compared to results of semiautomatic procedure (vessel analysis) as reference. Statistical analysis of correlation between MCA occlusion length and IVT efficacy (24 h recanalization rate according modified Thrombolysis In Myocardial Infarction criteria—mTIMI) was performed.
Results
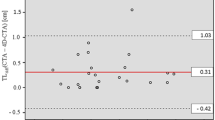
The distal end of occlusion was identified in all patients using tMIP, but only in 48 patients (60 %) using CTA. The manual measurement method was not statistically different and well correlated with reference tMIP-vessel analysis. (15.4 vs. 16.3 mm; p = 0.434; r = 97). In measurable occlusions by CTA, no significant difference was proved in manually measured lengths using tMIP and CTA (14.5 vs. 13.3 mm; p = 0.089).
Favorable recanalization (mTIMI 2–3) was achieved in 37 patients (47 %). Length of occlusion in M1 segment (p = 0.002) and M2 segment involvement (p = 0.017) were proved as independent negative predictors of recanalization. Using receiver operating characteristics analysis, the cutoff length of the M1 segment occlusion for favorable recanalization was found to be 12 mm.
Conclusion
The feasibility of MCA occlusion assessment using tMIP datasets and benefit over conventional CTA were confirmed. The manual measurement method was proved as feasible and simple with good correlation to reference semiautomatic analysis. The significant correlation of the MCA occlusion length and early recanalization was found. The length of 12 mm was recognized as cut-off length for favorable recanalization.






Similar content being viewed by others
References
Kim YS, Garami Z, Mikulik R, Molina CA, Alexandrov AV. Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion. Stroke. 2005;36:869–71.
Schellinger PD, Fiebach JB, Hacke W. Imaging-based Decision making in Thrombolytic therapy for ischemic stroke. Stroke 2003;34:575–83.
Kirmani JF, Alkawi A, Panezai S, Gizzi M. Advances in thrombolytics for treatment of acute ischemic stroke. Neurology. 2012;79:S119–25.
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Eng J Med. 2013;368:893–903.
Kirchhof K, Welzel T, Mecke T, Zoubaa S, Sartor K. Differentiation of white, mixed and red thrombi: value of CT in estimation of the prognosis of thrombolysis phantom study. Radiology. 2003; 228:126–30.
Barreto AD, Albright KC, Hallevi H, Grotta JC, Noser EA, Khaja AM, et al. Thrombus burden is associated with clinical outcome after intra-arterial therapy for acute ischemic stroke. Stroke. 2008;39:3231–5.
Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, Jansen O. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke. 2011;42:1775–7.
Riedel CH, Jensen U, Rohr A, Tietke M, Alfke K, Ulmer S, Jansen O. Assessment of thrombus in acute middle cerebral artery occlusion using thin-slice nonenhanced Computed Tomography reconstructions. Stroke. 2010;41:1659–64.
Konstas AA, Goldmakher GV, Lee TY, Lev MH. Theoretic basis and technical implementations of CT perfusion in acute ischemic stroke, Part 1: theoretic basis. AJNR Am J Neuroradiol. 2009;30:662–8.
Morhard D, Wirth CD, Fesl G, Schmidt C, Reiser MF, Becker CR, Ertl-Wagner B. Advantages of extended brain perfusion computed tomography: 9.6 cm coverage with time resolved computed tomography-angiography in comparison to standard stroke-computed tomography. Invest Radiol. 2010;45:363–9.
Zaidat OO, Lazzaro MA, Liebeskind DS, Janjua N, Wechsler L, Nogueira RG, et al. Revascularization grading in endovascular acute ischemic stroke therapy. Neurology. 2012;79:110–6.
Arnold M, Nedeltchev K, Remonda I, Fischer U, Brekenfeld C, Keserue B, Schroth G, Mattle HP. Recanalisation of middle cerebral artery occlusion after intra-arterial thrombolysis: different recanalisation grading systems and clinical functional outcome. J Neurol Neurosurg Psychiatry. 2005;76:1373–6.
Kim EY, Heo JH, Lee SK, Kim DJ, Suh SH, Kim J, Kim DI. Prediction of thrombolytic efficacy in acute ischemic stroke using thin-section noncontrast CT. Neurology. 2006;67:1846–8.
Kim EY, Lee SK, Kim DJ, Suh SH, Kim J, Heo JH, Kim DI. Detection of thrombus in acute ischemic stroke: value of thin-section noncontrast-computed tomography. Stroke. 2005;36:2745–7.
Pulli B, Yoo AJ. CT angiography source images with modern multisection CT scanners: delay time from contrast injection to imaging determines correlation with infarct core. AJNR Am J Neuroradiol. 2012;33:E61.
Frölich AM, Schrader D, Klotz E, Schramm R, Wasser K, Knauth M. Schramm P. 4D CT Angiography More Closely Defines Intracranial Thrombus Burden Than Single-Phase CT Angiography. AJNR Am J Neuroradiol. 2013;34:1908–13. doi:10.3174/ajnr.A3533.
Fröhlich AM, Psychogios MN, Klotz E, Schramm R, Knauth M, Schramm P. Angiographic reconstructions from whole-brain perfusion CT for the detection of large vessel occlusion in acute stroke. Stroke. 2012;43:97–102.
Yang CY, Chen YF, Lee CW, Huang A, Shen Y, Wei C, Liu HM. Multiphase CT angiography versus single-phase CT angiography: comparison of image quality and radiation dose. AJNR Am J Neuroradiol. 2008;29:1288–95.
Smith EJ, Vonken E, van der Schaaf IC, Mendrik AM, Dankbaar JW, Horsch AD, van Seeters T, van Ginneken B, Prokop M. Timing-invariant reconstruction for deriving high-quality CT angiographic data from cerebral CT perfusion data. Radiology. 2012;263:216–25.
Frohlich AM, Psychogios MN, Klotz E, Schramm R, Knauth M, Schramm P. Antegrade flow across incomplete vessel occlusions can be distinguished from retrograde collateral flow using 4-dimensional computed tomographic angiography. Stroke. 2012;43:2974–9.
Puetz V, Dzialowski I, Hill MD, Steffenhagen N, Coutts SB, O’Reilly C, Demchuk AM. Malignant profile detected by CT angiographic information predicts poor prognosis despite thrombolysis within three hours from symptom onset. Cerebrovasc Dis. 2010;29:584–91.
Sillanpaa N, Saarinen JT, Rusanen H, Hakomaki J, Lahteela A, Numminen H, Elovaara I, Dastidar P, Soimakallio S. The clot burden score, the Boston Acute Stroke Imaging Scale, the cerebral blood volume ASPECTS, and two novel imaging parameters in the prediction of clinical outcome of ischemic stroke patients receiving intravenous thrombolytic therapy. Neuroradiology. 2012;54:663–72.
Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, et al. Intracranial thrombus extent predicts clinical outcome, final infarct size and hemorrhagic transformation in ischemic stroke: the clot burden score. Int J Stroke. 2008;3:230–6.
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009;30:525–31.
Gralla J, Burkhardt M, Schroth G, El-Koussy M, Reinert M, Nedeltchev K, Slotboom J, Brekenfeld C. Occlusion length is a crucial determinant of efficiency and complication rate in thrombectomy for acute ischemic stroke. AJNR Am J Neuroradiol. 2008;29:247–52.
Spiotta AM, Vargas J, Hawk H, Turner R, Chaudry MI, Battenhouse H, Turk AS. Hounsfield unit value and clot length in the acutely occluded vessel and time required to achieve thrombectomy, complications and outcome. J Neurointerv Surg. 2013; doi:10.1136/neurintsurg-2013-010765.
Fugate JE, Klunder AM, Kallmes DF. What is meant by “TICI”? AJNR Am J Neuroradiol. 2013;34:1792–7.
Acknowledgements
This research was supported by the Charles University Research Fund (project number P36) and by the project of the Ministry of Health, Czech Republic for conceptual development of research organization 00669806—University Hospital in Pilsen, Czech Republic.
Conflicts of Interest
T. Flohr is an employee of Siemens Healthcare, Forchheim, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baxa, J., Rohan, V., Tupy, R. et al. Determination of the Middle Cerebral Artery Occlusion Length in Acute Stroke: Contribution of 4D CT Angiography and Importance for Thrombolytic Efficacy Prediction. Clin Neuroradiol 25, 257–265 (2015). https://doi.org/10.1007/s00062-014-0302-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-014-0302-x