Abstract
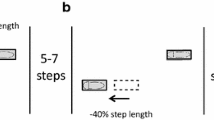
Background and aims: Visually guided stepping is an essential function in many normal activities of daily living requiring the coordination of eye movements with precise foot placement. The objective of this investigation was to compare the saccade-footlift latency in community dwelling elderly identified as high-risk for falling with elderly who are at a low-risk of falling during a walking task that requires precise foot placement. Methods: A non-randomized between-group repeated measures design was employed using independently living elderly volunteers from the Minneapolis, MN community. Thirty older adults volunteered to participate in the study; fifteen who had a history of a fall in the previous 12 months or a prolonged score on a fall risk screening instrument (Timed Up and Go test), and fifteen elders who had not fallen and had a negative score on the screening instrument. Subjects were required to walk along a pathway of 4 irregularly spaced stepping targets. The time between horizontal saccadic eye movement to the initiation of footlift (saccade-footlift latency) was the primary dependent measure. Results: The mean saccade-footlift latency between high-risk (H-R) elderly and low-risk (L-R) elderly was statistically different (mean H-R 940 ms, L-R 825 ms; F1,3=7.45, p=0.006). The H-R elderly also performed more slowly on the cognitive test — Trail Making Test Part B (mean H-R 195 s, L-R 129 s; F1,2=7.21, p=0.01). The results suggest that there is an association between horizontal saccades, stepping and cognition for elderly at risk for falling. Conclusions: The timing of saccades and precise foot placement in older persons living in the community are associated with fall risk status and cognitive status. The prolonged time for saccade-footlift in H-R elderly may be attributed to greater central nervous system processing time necessary to plan precise foot placements or volitional processing delays in postural control due to fall risk status. In addition, age related changes in cognitive functions appear to be associated with saccade stepping interaction when performing a visually guided stepping pattern and may influence the ability to coordinate precise lower extremity movements.
Similar content being viewed by others
References
Sattin RW. Falls among older persons: a public health perspective. Annu Rev Public Health 1992; 13: 489–508.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319: 1701–7.
Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health 1992; 82: 1020–3.
Fife D, Barancik JI. Northeastern Ohio Trauma Study III: incidence of fractures. Ann Emerg Med 1985; 14: 244–8.
Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 1997; 337: 1279–84.
Tinetti ME. Prevention of falls and fall injuries in elderly persons: a research agenda. Prev Med 1994; 23: 756–62.
Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc 2001; 49: 664–72.
Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 1990; 2: 136–41.
Rubenstein LZ, Robbins AS, Schulman BL, Rosado J, Osterweil D, Josephson KR. Falls and instability in the elderly. J Am Geriatr Soc 1988; 36: 266–78.
Klein BE, Klein R, Lee KE, Cruickshanks KJ. Performance-based and self-assessed measures of visual function as related to history of falls, hip fractures, and measured gait time. The Beaver Dam Eye Study. Ophthalmology 1998; 105: 160–4.
Bardy BG, Laurent M. Visual cues and attention demand in locomotor positioning. Percept Mot Skills 1991; 72: 915–26.
Chen HC, Schultz AB, Ashton-Miller JA, Giordani B, Alexander NB, Guire KE. Stepping over obstacles: dividing attention impairs performance of old more than young adults. J Gerontol A Biol Sci Med Sci 1996; 51: M116–22.
Di Fabio RP, Zampieri C, Henke J, Olson K, Rickheim D, Russell M. Influence of elderly executive cognitive function on attention in the lower visual field during step initiation. Gerontology 2005; 51: 94–107.
Hollands MA, Marple-Horvat DE. Visually guided stepping under conditions of step cycle-related denial of visual information. Exp Brain Res 1996: 109: 343–56.
Di Fabio RP, Greany JF, Zampieri C. Saccade-stepping interactions revise the motor plan for obstacle avoidance. J Mot Behav 2003; 35: 383–97.
Grasso R, Prevost P, Ivanenko YP, Berthoz A. Eye-head coordination for the steering of locomotion in humans: an anticipatory synergy. Neurosci Lett 1998; 253: 115–8.
Hollands MA, Patla AE, Vickers JN. “Look where you’re going!”: gaze behaviour associated with maintaining and changing the direction of locomotion. Exp Brain Res 2002; 143: 221–30.
Crowdy KA, Hollands MA, Ferguson IT, Marple-Horvat DE. Evidence for interactive locomotor and oculomotor deficits in cere-bellar patients during visually guided stepping. Exp Brain Res 2000; 135: 437–54.
Chapman G, Holands MA. Evidence for a link between changes to gaze behaviour and risk of falling in older adults during adaptive locomotion. Gait Posture 2006; 24: 288–94.
Johansson RS, Westling G, Backstrom A, Flanagan JR. Eye-hand coordination in object manipulation. J Neurosci 2001; 21: 6917–32.
Hollands MA, Marple-Horvat DE. Coordination of eye and leg movements during visually guided stepping. J Mot Behav 2001; 33: 205–16.
Di Fabio RP, Zampieri C, Greany JF. Aging and saccade-stepping interactions in humans. Neurosci Lett 2003; 339: 179–82.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–8.
Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function with self reported disability and prediction of mortality and nursing home admission. J Gerontol Med Sci 1994; 49: M85–94.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975: 12: 189–98.
Lezak MD. Neuropsychological Assessment, 3rd ed. New York: Oxford University Press, 1995.
Shumway-Cook, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000; 80: 896–903.
Lajoie Y, Teasdale N, Bard C, Fleury M. Attentional demands for walking: age-related changes. In: Ferrandez A, Teasdale N, eds. Changes in sensory motor behavior in aging. Amsterdam: Elsevier, 1996: 235–56.
Crowdy KA, Kaur-Mann D, Cooper HL, Mansfield AG, Offord JL, Marple-Horvat DE. Rehearsal by eye movement improves visuomotor performance in cerebellar patients. Exp Brain Res 2002; 146: 244–7.
Drew T, Jiang W, Kably B, Lavoie S. Role of the motor cortex in the control of visually triggered gait modifications. Can J Physiol Pharmacol 1996; 74: 426–42.
Glickstein M, Gerrits N, Kralj-Hans I, Mercier B, Stein J, Voogd J. Visual pontocerebellar projections in the macaque. J Comp Neurol 1994; 349: 51–72.
Stein JF, Glickstein M. Role of the cerebellum in visual guidance of movement. Physiol Rev 1992; 72: 967–1017.
van Donkelaar P, Lee RG. Interactions between the eye and hand motor systems: disruptions due to cerebellar dysfunction. J Neurophysiol 1994; 72: 1674–85.
Gauthier GM, Hofferer JM, Hoyt WF, Stark L. Visual-motor adaptation. Quantitative demonstration in patients with posterior fossa involvement. Arch Neurol 1979; 36: 155–60.
Taga G. A model of the neuro-musculo-skeletal system for anticipatory adjustment of human locomotion during obstacle avoidance. Biol Cybern 1998; 78: 9–17.
Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol 1991; 46: M164–70.
Binder EF, Storandt M, Birge SJ. The relation between psychometric test performance and physical performance in older adults. J Gerontol A Biol Med Sci 1999; 54: M428–32.
Nyberg S, Wahlström G, Bäckström T, Sundström-Poromaa I. No difference in responsiveness to a low dose of alcohol between healthy women and men. Pharmacol Biochem Behav 2004; 78: 603–10.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Greany, J.F., Di Fabio, R.P. Saccade to stepping delays in elders at high risk for falling. Aging Clin Exp Res 20, 428–433 (2008). https://doi.org/10.1007/BF03325148
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03325148