Summary
The toxicities of antimalarial drugs vary because of the differences in the chemical structures of these compounds. Quinine, the oldest antimalarial, has been used for 300 years. Of the 200 to 300 compounds synthesised since the first synthetic antimalarial, primaquine in 1926, 15 to 20 are currently used for malaria treatment, most of which are quinoline derivatives.
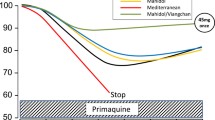
Quinoline derivatives, particularly quinine and chloroquine, are highly toxic in overdose. The toxic effects are related to their quinidine-like actions on the heart and include circulatory arrest, cardiogenic shock, conduction disturbances and ventricular arrhythmias. Additional clinical features are obnubilation, coma, convulsions, respiratory depression. Blindness is a frequent complication in quinine overdose. Hypokalaemia is consistently present, although apparently self-correcting, in severe chloroquine poisoning and is a good index of severity. Recent toxicokinetic studies of quinine and chloroquine showed good correlations between dose ingested, serum concentrations and clinical features, and confirmed the inefficacy of haemodialysis, haemoperfusion and peritoneal dialysis for enhancing drug removal.
The other quinoline derivatives appear to be less toxic. Amodiaquine may induce side effects such as gastrointestinal symptoms, agranulocytosis and hepatitis. The main feature of primaquine overdose is methaemoglobinaemia. No cases of mefloquine and piperaquine overdose have been reported.
Overdose with quinacrine, an acridine derivative, may result in nausea, vomiting, confusion, convulsion and acute psychosis.
The dehydrofolate reductase inhibitors used in malaria treatment are sulfadoxine, dapsone, proguanil (chloroguanide), trimethoprim and pyrimethamine. Most of these drugs are given in combination. Proguanil is one of the safest antimalarials. Convulsion, coma and blindness have been reported in pyrimethamine overdose. Sulfadoxine can induce Lyell and Stevens-Johnson syndromes. The main feature of dapsone poisoning is severe methaemoglobinaemia which is related to dapsone and to its metabolites. Recent toxicokinetic studies confirmed the efficacy of oral activated charcoal, haemodialysis and haemoperfusion in enhancing removal of dapsone and its metabolites.
No overdose has been reported with artemesinine, a new antimalarial tested in the People’s Republic of China.
The general management of antimalarial overdose include gastric lavage and symptomatic treatment. Chloroquine and quinine overdose require early monitoring of vital signs, ECG, blood pressure and intensive supportive treatment of cardiovascular disturbances: adrenaline (epinephrine) for circulatory arrest, isoprenaline (isoproterenol) for shock and conduction disturbances, DC countershock for ventricular tachycardia or fibrillation and sometimes pacemaker stimulation for later ventricular arrhythmia. Correction of hypokalaemia should be done very cautiously when cardiac depression has been rectified. Experimental and clinical data have shown that diazepam may reverse chloroquine cardiotoxicity. After ingestion of a large dose or when cardiotoxic symptoms are present, diazepam should be given systematically as a loading dose of 1 mg/kg followed by a continuous infusion. Dapsone-induced methaemoglobinaemia requires méthylene blue administration and repeated oral doses of activated charcoal. Haemodialysis may be indicated if methaemoglobinaemia recurs.
Chloroquine overdose remains the most severe and frequent cause of antimalarial drug poisonings. Its prognosis and high mortality should be improved by adequate supportive treatment and by the systematic and early treatment with diazepam.
Similar content being viewed by others
References
Abu-Aisha H, Abu-Sabaa HMA, Nur T. Cardiac arrest after intravenous chloroquine injection. Journal of Tropical Medicine Hygiene 82: 36–37, 1979
Adelusi SA, Dawodu AH, Salako LA. Kinetics of the uptake and elimination of chloroquine in children with malaria. British Journal of Pharmacology 14: 483–487, 1982
Akindele O, Odejide AO. Amodiaquine-induced involuntary movements. British Medical Journal 2: 214–215, 1976
Akinyanju O, Goddel JC, Ahmed J. Pyrimethamine poisoning. British Medical Journal 4: 147–148, 1973
Auzepy P, Rimailho A, Richard C, Riou B. Intoxications aiguës par les anti-arythmiques et antipaludiques. Revue de Praticien 34: 3267–3271, 1984
Bailey DJ. Cardiotoxic effects of quinidine and their treatment. Archives of Internal Medicine 105: 37–46, 1960
Barriot P, Riou B, Bodenan P, Noto R. Définition d’un protocole de prise en charge pré-hospitalière des intoxications graves par la chloroquine: résultats préliminaires. In Coeur et Toxiques, 24èmes Journées du Groupement Français des Centres Anti-Poisons, Strasbourg 24/25 Septembre 1986, résumé p. 60, 1986
Bass SW, Ramirez MA, Aviado DM. Cardiopulmonary effects of antimalarial drugs. Toxicology and Applied Pharmacology 21: 464–481, 1972
Bateman DN, Blain PG, Woodhouse KW, Rawlins MD, Dyson H, et al. Pharmacokinetics and clinical toxicity of quinine overdosage: lack of efficacy of techniques intended to enhance elimination. Quarterly Journal of Medicine 54: 125–131, 1985
Bateman DN, Dyson EH. Quinine toxicity. Advances of Drug Reactions 4: 215–233, 1986.
Bellet S, Hamdan G, Somlyo A, Lara R. The reversal of cardiotoxic effects of quinidine by molar sodium lactate: an experimental study. American Journal of Medical Sciences 237: 165–176, 1959
Bellet S, Wasserman F. The effects of molar sodium lactate in reversing the cardiotoxic effect of hyperpotassemia. Archives of Internal Medicine 100: 565–575, 1957
Bergmann M, Zauger J, Hieger W. Klinische Erfahrungen bei der Behandlung von Harnwegsinfektionen mit dem Langzeitsulfonamid Ro 4-4393. Zeitschrift für Urologie Néphrologie 56: 141–148, 1963
Bergoend H, Löffler A, Amar R, Maleville J. Réactions cutanées survenues au cours de la prophylaxie de masse de la méningite cérébro-spinale par un sulfamide long-retard (à propos de 997 cas). Annales de Dermatologie et Syphiligraphie 95: 481–490, 1968
Berlin CM, Stackman JM, Vesell ES. Quinine-induced alterations in drug disposition. Clinical Pharmacology and Therapeutics 18: 670–679, 1975
Berlin G, Brodin B, Hilden JO, Martensson J. Acute dapsone intoxication: a case treated with continuous infusion of methylene blue, forced diuresis and plasma exchange. Clinical Toxicology 22: 537–548, 1984
Berneis K, Boguth W. Distribution of sulfonamides and sulfonamide potentiators between red blood cells, proteins and aqueous phases of the blood of different species. Chemotherapy 22: 390–409, 1976
Böhni E, Fust B, Rieder J, Schaerer G, Havas L. Comparative toxicological chemotherapeutic and pharmacokinetic studies with sulphormethoxine and other sulphonamides in animals and man. Chemotherapy 14: 195–226, 1969
Boland ME, Brennand Roper SM, Henry JA. Complications of quinine poisoning. Lancet 1: 384–385, 1985
Bondurand A, N’Dri K, Coffi S, Saracino E. L’intoxication à la chloroquine au CHU Abidjan. Afrique Médical 179: 239–242, 1980a
Bondurand A, Tricoche R, Offoumou K, N’Dri D, Coffi K. Intoxications aiguës à la chloroquine. Encyclopédie Médico-Chirurgicale. Instantanés Médicaux 4: 21–23, 1980b
Boots M, Phillips M, Curtis JR. Megaloblastic anemia and pancytopenia due to proguanil in patients with chronic renal failure. Clinical Nephrology 18: 106–108, 1982
Bouvier AM, Bertrand D, Timsit JF, Ricome JL. Intoxications massives et prolongées par la nivaquine: effets du diazépam. Réanimation, Soins Intensifs, Médecine d’Urgence 2: 265, 1986
Brandfonbrener M, Kronholm J, Jones HR. The effect of serum potassium concentration and quinidine toxicity. Journal of Pharmacology and Experimental Therapeutics 154: 250–254, 1966
Brinton GS, Norton EWD, Zahn JR, Knighton RW. Ocular quinine toxicity. American Journal of Ophthalmology 90: 403–410, 1980
Britton WJ, Kevau JH. Intentional chloroquine overdosage. Medical Journal of Australia 21: 407–410, 1978
Browne GF, Coppel DL. Management of quinine overdose. Human Toxicology 3: 399–402, 1984
Bunger P. Die Pharmakokinetick des Fanasils. In Mossner & Thomssen (Eds) Infektionskrankheiten 4. Kongress Infektionskrankheiten, München, pp. 855–868, Schattauer, Stuttgart, 1967
Burg F. Intoxications volontaires par la chloroquine. Thèse Médecine, Université Louis Pasteur, Strasbourg, 1976
Caldwell RW, Nash CB. Pulmonary and cardiovascular effects of mefloquine methanesulfonate. Toxicology and Applied Pharmacology 40: 437–448, 1977
Caminade S, Ricome JL, Auzepy P. Intoxications aiguës par quinine, quinidine et chloroquine: à propos de 18 cas. Journal des Agrégés 11: 613–618, 1978
Cann HM, Verhulst HL. Fatal acute chloroquine poisoning in children. Pediatrics 27: 95–102, 1961
Catchpool JF. Antiprotozoal drugs. In Meyers et al. (Eds) Review of medical pharmacology, 5th ed., pp. 605–633, Lange Medical Publications, Canada, 1976
Cavallito JC, Nichol CA, Brenckman WD, de Angelis RL, Stickney DR, et al. Lipid-soluble inhibitors of dihydrofolate reductase. I kinetics, tissue distribution and extent of metabolism of pyrimethamine, metoprine and etoprine in the rat, dog and man. Drug Disposition and Metabolism 6: 329–337, 1978
Champagne D. Intoxications volontaires à la chloroquine. Thèse Médecine, Université de Paris, France, 1973
Charbonneau P, Lacotte J, Lemarchand C, Commeau P, Pellerin R, et al. Effet antiarythmique du diazépam lors des intoxications à la chloroquine. Réanimation, Soins Intensifs, Médecine d’Urgence 2: 265, 1986
Chen L, Qi FY, Zhou Y-C. Field observations on the antimalarial piperaquine. Chinese Medical Journal 95: 281–286, 1982
Chernof D. Dapsone-induced hemolysis in G6PD deficiency. Journal of the American Medical Association 201: 122–125, 1967
China Cooperative Research Group on Qinghaosu and its Derivatives as Antimalarials. Metabolism and pharmacokinetics of Qinghaosu and its derivatives. Journal of Traditional Chinese Medicine 2: 25–30, 1982a
China Cooperative Research Group on Qinghaosu and its Derivatives as Antimalarials. Studies on the toxicity of Qinghaosu and its derivatives. Journal of Traditional Chinese Medicine 2: 31–38, 1982b
Cibis GW, Burian HM, Blodi FC. Electroretinogram changes in acute quinine poisoning. Archives of Ophthalmology 90: 307–309, 1973
Clyde DF. Drug resistance of malaria parasites in Tanzania. East African Medical Journal 43: 405–408, 1966
Conso F. Death from acute poisoning in man. Veterinary and Human Toxicology 21 (Suppl.): 68–69, 1979
Constantin B, Charmot G. Intoxications volontaires par la chloroquine. Thérapie 21: 387–395, 1966
Cooke TJL. Dapsone poisoning. Medical Journal of Australia 23: 1158–1159, 1970
Crouzette J, Vicaut E, Palombo S, Girre C, Fournier PE. Experimental assessment of the protective activity of diazepam on the acute toxicity of chloroquine. Journal of Toxicology, Clinical Toxicology 20: 271–279, 1983
Czajka PA, Flynn PJ. Nonfatal chloroquine poisoning. Clinical Toxicology 13: 361–369, 1978
Davies R. Fatal poisoning with undolac (diaminodiphenylsulphone). Lancet 1: 905–906, 1950
Desjardins RE, Pamplin CL, von Bredow J, Barry KG, Canfield CJ. Kinetics of a new antimalarial, mefloquine. Clinical Pharmacology and Therapeutics 26: 372–379, 1979
Diamondstone AH, Braveman BL, Baker LA. Ventricular tachycardia and bilateral amaurosis produced by quinine poisoning. Archives of Internal Medicine 80: 763–770, 1947
Di Maio JM, Henry MLD. Chloroquine poisoning. Southern Medical Journal 67: 1031–1035, 1974
Djelardje S. Intoxications volontaires par la chloroquine. Thèse Médecine, Université d’Abidjan, 1976
Don Micheal TA, Aiwazzadeh S. Effects of acute chloroquine poisoning. American Heart Journal 79: 831–842, 1970
Dyson EH, Proudfoot AT, Bateman DN. Quinine amblyopia: is current management appropriate? Clinical Toxicology 23: 571–578, 1985-1986
Dyson EH, Proudfoot AT, Prescott LF, Heyworth R. Death and blindness due to overdose of quinine. British Medical Journal 291: 31–33, 1985
Elliot RH. Quinine poisoning, its ocular lesions and visual disturbances. American Journal of Ophthalmology 1: 547–560, 650–658, 1918
Elmalem J, Poulet B, Gamier R, Frelon JH, Castot A. Les accidents graves lors de la prescription de pyriméthamine chez les nourissons traités pour une toxoplasmose. Thérapie 40: 357–359, 1985
Elonen E, Neuvonen PJ, Halmekoski J, Mattila MJ. Acute dapsone intoxication: a case with prolonged symptoms. Clinical Toxicology 14: 79–85, 1979
Endre ZH, Charlesworth JA, MacDonald GJ, Woodbridge L. Successful treatment of acute dapsone intoxication using charcoal hemoperfusion. Australia and New Zealand Journal of Medicine 13: 509–512, 1983
Ferone R. Dihydrofolate reductase inhibitors. In Peters & Richards (Eds) Handbook of experimental pharmacology, Vol. 68, Antimalarial drugs II, pp. 207–221, Springer, Berlin, 1984
Findlay GM. Recent advances in chemotherapy, 3rd ed., Vol. 2, Churchill J+A, London, 1951
Fleckenstein L, Pamplin CL, von Bredow J, Heiffer MH. Pharmacokinetics of halofantrine a new antimalarial. 2nd International Conference on Malaria and Babesiosis, Annecy. Abstract, p. 87, 1983
Floyd M, Hill AVL, Ormston BJ, Menzies R, Porter R. Quinine amblyopia treated by haemodialysis. Clinical Nephrology 2: 44–46, 1974
Frija GA. Intoxications aiguës à la chloroquine: à propos de 38 cas. Médecine Tropicale 35: 23–30, 1975
Frisk Holmberg M, Bergqvist Y, Domeij-Niberg B, Hellström L, Jansson F. Chloroquine serum concentration and side effects: evidence for dose-dependent kinetics. Clinical Pharmacology and Therapeutics 25: 345–350, 1979
Frisk Holmberg M, Bergqvist Y, Englund U. Chloroquine intoxication. British Journal of Clinical Pharmacology 15: 502–503, 1983
Frisk Holmberg M, Bergqvist Y, Termond E, Domeij-Nyberg B. The single dose kinetics of chloroquine and its major metabolite desethyl-chloroquine in healthy subject. European Journal of Clinical Pharmacology 26: 521–530, 1984
Garnham JC, Shotton KRE, Turner P. The bioavailability of quinine. Journal of Tropical Medicine and Hygiene 70: 264–269, 1976
Garrod GD, Judson JA. Fatal quinine poisoning: a case report. New Zealand Medical Journal 94: 215–216, 1981
Gelber R, Peters JH, Gordon GR, Glazko AJ, Levy L. The polymorphic acetylation of dapsone in man. Clinical Pharmacology and Therapeutics 12: 225–238, 1971
Gibbs JL, Trafford A, Sharpstone P. Quinine amblyopia treated by combined haemodialysis and activated resin haemoperfusion. Lancet 1: 752–753, 1985
Gillespie P, Wagner F. Amodiaquine agranulocytosis. Medical Journal of Australia 1: 298, 1977
Glader BE. Haemolysis by diphenylsulphones: comparative effects of DDS and hydroxylamine D. Journal of Laboratory and Clinical Medicine 81: 267–272, 1973
Gladtke E. Ein Sulfanilamid mit extrem lagnsamer Elimination: Elimination, Verteilung, Dosierung und enterale Absorption von 4-Sulfanilamido-5,6-dimethoxypyrimidin beim Kind. Klinische Wochenschrift 43: 1332–1334, 1965
Glick L, Munford J. Quinine amblyopia: treatment by stellate ganglion block. British Medical Journal 2: 94–96, 1955
Gosselin RE, Hodge HC, Smith RP, Gleason MN (Eds). Clinical toxicology of commercial products, 4th ed., pp. 282–289, Williams and Wilkins Co., Baltimore, 1976
Gottsegen G, Östör E. Prevention of the cardiotoxic effect of quinidine by isoproterenol. American Heart Journal 65: 102–109, 1963
Granier P, Carrere-Debat D, Holzapfel L, Giudicelli DP. Correction des troubles de conduction intra-ventriculaires par le diazépam au cours de deux intoxications massives par la chloroquine. 24èmes Journées du Groupement Français des Centres Anti-Poisons, Strasbourg 24/25 Septembre 1986. Résumé, p. 60, 1986
Greaves J, Evans DAP, Gilles HM, Fletcher KA, Bunnag D, et al. Plasma kinetics and urinary excretion of primaquine in man. British Journal of Clinical Pharmacology 10: 399–405, 1980
Gustafsson LI, Walker O, Alvan G, Beermann B, Estevez F, et al. Disposition of chloroquine in man after single intravenous and oral doses. British Journal of Clinical Pharmacology 15: 471–479, 1983
Hatton CSR, Peto TEA, Bunch C, Pasvol G, Russell SJ, et al. Frequency of severe neutropenia associated with amodiaquine prophylaxis against malaria. Lancet 1: 411–413, 1986
Heath A, Ahlmen J, Mellstrand T, Wickström I. Resin hemoperfusion in chloroquine poisoning. Journal of Toxicology, Clinical Toxicology 19: 1067–1071, 1982
Hess ME, Schmidt CF. Cardiovascular effects of chloroquine with special reference to its antifibrillatory action. Circulation Research 7: 86–92, 1959
Hiremath CB. Absorption, distribution and excretion of x-(2-di-n-butylaminoéthyl)-1,3-dichloro-6-trifluoromethyl-9-phenanthrene methanol-C14) in rats and rhesus monkeys. Federation Proceedings 33: 472, 1974
Hirst LW, Sanborn G, Green WR, Miller NR, Heath WD. Amodiaquine ocular changes. Archives of Ophthalmology 100: 1300–1304, 1982
Hoang PTD, Pourriat JL, Larmignat P, Lapandry C, Gabry AL, et al. Intoxications aiguës à la chloroquine: traitement par le diazépam. Annales Françaises d’Anesthésie et Réanimation 1: 321–323, 1982
Hofheinz W, Merkli B. Quinine and quinine analogues. In Peters & Richards (Eds) Handbook of experimental pharmacology, antimalarial drugs II, Vol. 68, pp. 61–81, Springer, Berlin, 1984
Hornstein OP, Ruprecht KW. Fansidar-induced Stevens-Johnson syndrome. New England Journal of Medicine 307: 1529–1530, 1982
Hruby K, Missliwetz J. Poisoning with oral antiarrhythmic drugs. International Journal of Clinical Pharmacology, Therapy and Toxicology 23: 253–257, 1985
Hutchinson DBA, Whiteman PD, Farquhar JAV. Agranulocytosis associated with Maloprim: review of cases. Human Toxicology 5: 221–227, 1986
Irey NS. Blood and tissue concentrations of drugs associated with fatalities. Medical Clinics of North America 58: 1093–1102, 1974
Israili ZH, Cucinell SA, Vaught J, Davis E, Lesser JM, et al. Studies of the metabolism of dapsone in man and experimental animals: formation of N-hydroxy metabolites. Journal of Pharmacology and Experimental Therapeutics 187: 138–151, 1973
Jaeger A, Sauder P, Tempe JD, Mantz JM. Intoxications aiguës par le disopyramide: etude multicentrique de 106 observations. Nouvelle Presse Médicale 10: 2883–2887, 1981
Jaeger A, Mangin P, Sauder P, Kopferschmitt J, Lugnier A, et al. Acute chloroquine intoxication: toxicokinetic study of 5 cases. Clinical Toxicology 23: 468, 1985
Kale OO. Clinical trials of amodiaquine in onchocerciasis. Bulletin of the World Health Organisation 60: 929, 1982
Koudogbo B, Asseko MC, Nguemby Mbina C, Laguerret-Atadou V. Mode d’action antidotique du diazepam dans le traitement des intoxications à la chloroquine. Journal de Toxicologie Clinique et Expérimentale 6: 307–312, 1986
Kramer PA, Glader BE, Li TK. Mechanism of methaemoglobin formation by diphenylsulphones: effects of 4-amino-4′hydroxyaminodiphenylsulphone and other p-substituted derivatives. Biochemical Pharmacology 21: 1265–1274, 1972
Lambert M, Sonnet J, Mahieu P, Hassoun A. Delayed sulfhemoglobinemia after acute dapsone intoxication. Journal of Toxicology, Clinical Toxicology 19: 45–50, 1982
Lareng L, Fabre M, Jean D, Bourzai V. Intoxication par la Nivaquine. Cahiers d’Anesthésiologie 28: 223–231, 1980
Larrey D, Castot A, Pessayre D, Merigot P, Maschayekhy JP, et al. Amodiaquine-induced hepatitis. A report of seven cases. Annals of Internal Medicine 104: 801–803, 1986
Lee CC, Kintner LD, Castles TR, Landes AM, Cronin MC, et al. Acute and subacute oral toxicities of x-(2-piperidyl)-2,8-bis (trifluoromethyl)-4-quinolinemethanol hydrochloride, WR-142.490 (AY-65742) in dogs: interim report no. 57, US Army medical research and development command contract no. DA.49.193-MD-2759, Jan. 21, 1972a
Lee CC, Kintner LD, Castles TR, Landes AM, Cronin MC, et al. Acute and subacute toxicities of x-(2-piperidyl)-2,8-bis (trifluoromethyl)-4-quinoline-methanol hydrochloride: WR-142.490 (AY-65742) in rodents. Interim report no. 56. US Army medical research and development command contract no. DA-49-193-MD-2559, Jan. 20, 1972b
Lee CC, Kintner LD, Sanyer JL, Castles TR, Landes AM, et al. Acute and subacute toxicities of l,3-dichloro-6-trifluoromethyl-9-(l-hydroxy-3-(dibutylamino) propyl) phenanthrene hydrochloride, WR-171.669 (BBB-41223), in rodents: Interim report no. 65. US Army medical research and development command contract no. DA-49-193-MD-2759, October 3, 1972c
Lepeu G, Codine P, Jambon F, Bertrand A. Agranulocytose à l’amodiaquine. Nouvelle Presse Médicale 10: 2827, 1981
Lindenmayer JP, Vargas P. Toxic psychosis following use of quinacrine. Journal of Clinical Psychiatry 42: 162–164, 1981
Lofaso F, Baud FJ, Halna de Fretay X, Bismuth C, Staikowsky F, et al. Hypokaliémie au cours d’intoxications massives par la chloroquine. Journal de Toxicologie Clinique et Expérimentale 6: 33–39, 1986a
Lofaso F, Baud FJ, Halna de Fretay X, Staikowsky F, Sidhhom N, et al. Hypokaliémies au cours d’intoxications massives par la chloroquine: trois cas. Réanimation, Soins Intensifs, Médecine d’Urgence 2: 236, 1986b
Maddux BD, Whitting RB. Toxic synergism of disopyramide and hyperkaliemia. Chest 78: 654–656, 1980
Maegraith BG, Tottey MM, Adams ARD, Homer-Andrews WH, King JD. The absorption and excretion of paludrine in the human subject. Annals of Tropical Medicine and Parasitology 40: 493–506, 1946
Maier RD, Benkert B. Toxikologische Aspekete beim mehrtägigen Verlauf einer tödlichen Chloroquin-intoxikation. Zeitschrift für Rechtsmedizin 92: 27–33, 1984
Manfredi G, de Panfilis G, Zampetti M, Allegra F. Studies on dapsone induced haemolytic anaemia. British Journal of Dermatology 100: 427, 1979
McCann WP, Permisohn R, Palmisano PA. Fatal chloroquine poisoning in a child: experience with peritoneal dialysis. Pediatrics 55: 536–537, 1975
McChesney EW, Banks PDWF, McAuliff JP. Laboratory studies of the 4-aminoquinoline antimalarials. II. Plasma levels of chloroquine and hydroxychloroquine in man after various oral dosage regimens. Antibiotics and Chemotherapy 12: 583–593, 1962
McChesney EW, Fasco MJ, Banks WF. The metabolism of chloroquine in man during and after repeated oral dosage. Journal of Pharmacology and Experimental Therapeutics 158: 323–331, 1967
McGuiness BW. Experience with sulphormethoxine, a new longacting sulphonamide. British Journal of Clinical Practice 23: 331–334, 1969
Mihaly GW, Ward SA, Edwards G, Orme ME, Breckenridge AM. Pharmacokinetics of primaquine in man: identification of the carboxylic acid derivative as a major plasma metabolite. British Journal of Clinical Pharmacology 17: 441–446, 1984
Mimica I, Fry W, Eckert G, Schwartz DE. Multiple-dose kinetic study of mefloquine in healthy male volunteers. Chemotherapy 29: 184–187, 1983
Mondain J, Gras G, Ndiaye PD. Répartition tissulaire de la chloroquine dans dix-huit cas d’intoxication volontaire. Bulletin de la Société de Pathologie Exotique 72: 86–92, 1979
Morgan MDL, Pusey CD, Rainford DJ, Robins-Cherry AM. The treatment of quinine poisoning with charcoal haemoperfusion. Postgraduate Journal of Medicine 59: 25–27, 1983
Mu JY, Israili ZH, Dayton PG. Studies of the disposition and metabolism of mefloquine HC1 (WR 142,490), a quinolinemethanol antimalarial, in the rat: limited studies with an analog, WR 30,090. Drug Metabolism and Disposition 3: 198–210, 1975
Muhlens P. Die Behandlung der naturlichen menschlichen Malaria-Infektion mit Plasmochin. Naturwissenschaften 14: 1162–1166, 1926
Neftel KA, Woodtly W, Schmid M, Frick PG, Fehr J. Amodiaquine induced agranulocytosis and liver damage. British Medical Journal 292: 721–723, 1986
Neuvonen PJ, Elonen E, Haapanen EJ. Acute dapsone intoxication: clinical findings and effect of oral charcoal and haemodialysis on dapsone elimination. Acta Medica Scandinavica 214: 215–220, 1983
Nir I. Antiprotozoal drugs. In Dukes (Ed.) Side effects of drugs annual 8, pp. 273–281, Elsevier Science Publishers B.V., Amsterdam, 1984
O’Keefe B, Hayler AM, Holt DW, Medd R. Cardiac consequences and treatment of disopyramide intoxication: experimental evaluation in dogs. Cardiovascular Research 13: 630–634, 1979
Orloff J, Berliner RW. The mechanism of the excretion of ammonia in the dog. Journal of Clinical Investigations 35: 233–235, 1956
Otten H, Plempel M, Siegenthaler W. Antibiotica-Fibel, 4th ed., Thieme, Stuttgart, 1975
Pengelly CD. Dapsone-induced hemolysis. British Medical Journal 246: 662–664, 1963
Pille G, Labegorre J, Lambourg J, Lunven P. Intoxications volontaires à la chloroquine (Nivaquine*) à Dakar (Sénégal). Médecine Tropicale 18: 304–311, 1958
Powell RD, McNamara JV. Quinine: side effects and plasma levels. Proceedings of the Helminthological Society of Washington 39: 331–338, 1972
Pussard E, Verdier F, Faurisson F, Blayo MC. Pharmacocinétique de FAmodiaquine et prophylaxie du paludisme a Plasmodium Falciparum. Bulletin de la Société de Pathologie Exotique 78: 959–964, 1985
Rainier-Pope CR, Schrire V, Beck W, Barnard CN. The treatment by closed-chest resuscitation and external defibrillation. American Heart Journal 63: 582–590, 1962
Rakotoson L. Intoxication aiguë par la chloroquine. Journal Européen de Toxicologie 6: 85–93, 1973
Reber H, Rutishauser G, Thölen H. Clearance-Untersuchungen am Menschen mit Sulfamethoxazol und Sulforthodimethoxin. In Proceedings of the 3rd International Congress of Chemotherapy, Stuttgart, 1963, Vol. 1, pp. 648–653, Thieme, Stuttgart, 1964
Reigart JR, Harold LT, Lindsey JM. Repetitive doses of activated charcoal in dapsone poisoning in a child. Journal of Toxicology, Clinical Toxicology 19: 1061–1066, 1982
Reimold WD, Larbig D, Kochsiek K. Hypokaliämie und Herzrhythmusstörungen infolge Chininvergiftung. Deutsche Medizinische Wochenschrift 95: 517–521, 1970
Rinehart J, Arnold J, Canfield CJ. Evaluation of two phenanthrenemethanols for antimalarial activity in man: WR-122.455 and WR-171.669. American Journal of Tropical Medicine and Hygiene 25: 769–774, 1976
Riou B, Rimailho A, Galliot M, Bourdon R. Effets du diazépam dans l’intoxication expérimentale aiguë par la chloroquine. Réanimation, Soins Intensifs, Médecine d’Urgence 2: 236, 1986
Ritschel WA, Hammer GV, Thompson GA. Pharmacokinetics of antimalarials and proposais for dosage regimens. International Journal of Clinical Pharmacology 16: 395–401, 1978
Robertson DH, Kothanda Raman KR. Quinine poisoning: an unusual indication for stellate ganglion blockade. Anaesthesia 34: 1041–1042, 1979
Robinson AE, Coffer AI, Camps FE. The distribution of chloroquine in man after fatal poisoning. Journal of Pharmacy and Pharmacology 22: 700–703, 1970
Rollo IM. Chemotherapy of parasitic diseases. In Goodman & Gilman (Eds) The pharmacological basis of therapeutics, pp. 1095–1124, 5th ed., Macmillan Company, New York, 1975
Rollo IM. Drugs used in the chemotherapy of malaria. In Goodman & Gilman (Eds) The pharmacological basis of therapeutics, pp. 1044, 6th ed., Macmillan Company, New York, 1980
Ru-Yun J. Artemether. Drugs of the Future 7: 717–718, 1982
Sabcharoen A, Chongsuphajaisiddhi T, Attanath P. Serum quinine concentrations following the initial dose in children with falciparum malaria. South East Asian Journal of Tropical Medicine and Public Hygiene 13: 556–562, 1982
Sabto J, Pierce RM, West RH, Gurr FW. Haemodialysis, peritoneal dialysis, plasmapheresis and forced diuresis for the treatment of quinine overdose. Clinical Nephrology 16: 264–268, 1981
Scholer HJ, Leimer R, Richie R. Sulphonamides and sulphones. Handbook of Experimental Pharmacology 68: 123–206, 1984
Schvartsman S. Sulfone methemoglobinemia. Clinical Toxicology 15: 468, 1979
Schwartz DE, Eckert G, Hartmann D, Weber B, Richard-Lenoble D, et al. Single dose kinetics of mefloquine in man. Chemotherapy 28: 70–84, 1982
Schwartz DE, Warrell DA, Dubach VC, Ranalder VB, White NJ, et al. Pharmacokinetic parameters of mefloquine in adult male Thai patients and Swiss volunteers. Abstract. Proceedings of the XIth International Congress for Tropical Medicine and Malaria. Calgary, p. 136, 1984
Smith CC, Ihrig J, Menne R. Antimalarial activity and metabolism of the biguanides. 1. Metabolism of chloroguanide and chloroguanide triazine in Rhesus monkeys and man. American Journal of Tropical Medicine Hygiene 10: 694–703, 1961
Smith CC, Schmidt LH. Observations on the absorption of pyrimethamine from the gastrointestinal tract. Experimental Parasitology 13: 178–185, 1963
Stanfield JP. A case of acute poisoning with dapsone. Journal of Tropical Medicine and Hygiene 66: 292–295, 1963
Sturt J. Too much of a good thing. Papua New Guinea Medical Journal 10: 97, 1967
Sweeney TR. Drug with quinine-like action. In Peters & Richards (Eds) Handbook of experimental pharmacology, Vol. 68/11, Antimalarial drugs, current antimalarials and new drug developments, pp. 267–324, Springer Verlag, Berlin, 1984
Szajewski J, Dorywalski T, Tomecka Z, Sabiniewich M. A case of severe poisoning with diaminediphenylsulphone (DDS, an antileprous drug). Polish Archives of Medicine 49: 181–186, 1972
Tariq M, Abdullah AA. Chloroquine. Analytical Profiles of Drug Substances 13: 95–125, 1984
Tayler P, Edelstein A, Hugues IA. A case of quinine self-poisoning in a boy. Archives of Disease in Childhood 55: 478–488, 1980
Tester Dalderup CBM. Antiprotozoal drugs. In Dukes (Ed.) Meyler’s side effects of drugs, 10th ed., pp. 525–537, Elsevier Science Publishers, Amsterdam, 1984
Trenholme GM, Williams RL, Rieckmann KH, Frischer H, Carson PE. Quinine disposition during malaria and during induced fever. Clinical Pharmacology and Therapeutics 19: 459–467, 1976
Van Stone JC. Hemodialysis and chloroquine poisoning. Journal of Laboratory and Clinical Medicine 88: 87–90, 1976
Viala A, Durand A, Cano JP, Jouglard J. La chloroquine: sort dans l’organisme et toxicologie analytique. Journal Européen Toxicologie 72: 189–201, 1972
Vitris M, Aubert M. Intoxications à la chloroquine: notre expérience à propos de 80 cas. Dakar Medical 28: 593–602, 1983
Walker O, Dawodu AH, Adeyokunnu AA, Salako LA, Alvan G. Plasma chloroquine and desethylchloroquine concentrations in children during and after chloroquine treatment for malaria. British Journal of Clinical Pharmacology 16: 701–705, 1983
Wasserman F, Brodsky L, Kathe JH, Rodensky PL, Dick MM, et al. The effect of molar sodium lactate in quinidine intoxication: an experimental study. American Journal of Cardiology 2: 294–299, 1959
Weetman RM, Boxer LA, Brown MP, Mantich NM, Baehner RL. In vitro inhibition of granulopoeisis by 4-amino-4′-hydroxylamino-diphenylsulphone. British Journal of Haematology 45: 361–370, 1980
Weniger H. Review of side effects and toxicity of chloroquine. Bulletin of the World Health Organization 79: 906, 1979
White NJ, Chantavanich P, Krishna S, Bunch S, Silamut K. Quinine disposition kinetics. British Journal of Clinical Pharmacology 16: 399–404, 1983
White NJ. Clinical pharmacokinetics of antimalarial drugs. Clinical Pharmacokinetics 10: 187–215, 1985
White NJ, Looareesuwan S, Warrel DA, Warrel MJ, Bunnag D, et al. Quinine pharmacokinetics and toxicity in cerebral and uncomplicated falciparum malaria. American Journal of Medicine 73: 564–571, 1982
Willerson D, Rieckmann KH, Kass L, Carson PE, Frischer H, et al. The chemoprophylactic use of diformyldiamino-diphenylsulfone (DFD) in falciparum malaria. American Journal of Tropical Medicine Hygiene 21: 138–143, 1972
Woodhouse KW, Henderson DB, Charlton B, Peaston RT, Rawlins MD. Acute dapsone poisoning: clinical features and pharmacokinetic studies. Human Toxicology 3: 507–510, 1983
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jaeger, A., Sauder, P., Kopferschmitt, J. et al. Clinical Features and Management of Poisoning due to Antimalarial Drugs. Med Toxicol Adverse Drug Exp 2, 242–273 (1987). https://doi.org/10.1007/BF03259868
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03259868