Summary
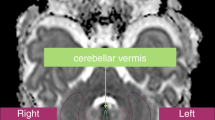
The study was based on the hypothesis that cerebellar hypoxia may play a role in sudden infant death syndrome resulting in morphological changes of the cerebellar cortex, especially with respect to Purkinje cell density. In the morphological evaluation of the Purkinje cell layer, special consideration was additionally given to secondary alterations (i.e., macrophage and/or astrocyte reaction). A total of 12 sudden infant death syndrome cases were compared with an age- and sex-matched control group. The Purkinje cell density was evaluated by determining the number of these cells per suface unit on parasagittal sections in both hemispheres. The myelomonocytic and glial reaction was demonstrated by immunohistochemical methods using lysozyme as leukocyte and macrophage markers and glial fibrillary acidic protein as an astrocyte marker. Qualitatively, no alterations resembling a macrophage or glial cell reaction were detected in sudden infant death syndrome. No differences between the right and left cerebellar hemisphere could be established in the victims of sudden infant death syndrome nor in the controls. The number of Purkinje cells per 0.352 mm2 cortex was higher in the younger victims of sudden infant death (younger than 45 weeks of gestation) than in all matched controls. A statistically significant difference in Purkinje cell density, however, could not be established, and, especially, no indications of hypoxia were observed in the cerebellar cortex.
Similar content being viewed by others
References
Azarelli B, Meade P, Müller J (1980) Hypoxic lesions in areas of primary myelination. A distinct pattern in cerebral palsy. Child's Brain 7:132–145
Becker LE (1983) Neuropathological basis for respiratory dysfunction in sudden infant death syndrome. In: Sudden infant death syndrome. Tildon JT, Roeder LM, Steinschneider A (eds), Academic Press, New York, pp 99–114
Duvernoy H, Delon S, Vannson JL (1983) The vascularization of the human cerebellar cortex. Brain Res Bull 11:419–480
Emery JL (1979) The central nervous system and cot deaths. Dev. Med Child Neurol 21:239–242
Eng LF (1985) Glial fibrillary acidic protein (GFAP): the major protein of glial intermediate filaments in differentiated astrocytes. J Neuroimmunol 8:203–214
Eng LF, De Armond SJ (1983) Immunochemistry of the glial fibrillary acidic protein. Prog Neuropathol 5:19–39
Gerhardt L (1962) Zur Morphologie der perinatalen Hypoxie. In: Klinke K (ed) Probleme der ersten Lebenstage, Schattauer Verlag. Stuttgart, pp 12–26
Gillilan LA (1969) The arterial and venous blood supplies to the cerebellum of primates. J Neuropathol Exp Neurol 28:295–307
Kinney HC, Burger PC, Harrell FE, Jr (1983) “Reactive gliosis” in the medulla oblongata of victims of the sudden infant death syndrome. Pediatrics 72:181–187
Kirchmeier P (1978) Hirnentwicklungsstörungen bei intrauteriner entwicklungsabweichung. Präliminäre Studie zur Frage der Entwicklungsbeeinträchtigung der Großhirn- und Kleinhirnrinde in Abhängigkeit von Reifungsstörungen, Hypoplasie und Durchblutungsstörungen der Planzenta bei 51 perinatalen Todesfällen. Berlin: Inaug Dis
Kloos K (1965) Neue pathologisch-anatomische Befunde bei der primären Asphyxie und dem respiratory-distress-syndrome. In: Ewerbeck, H., Friedberg V (eds) Die Übergangsstörungen des Neugeborenen und die Bekämpfung der perinatalen Mortalität. Thieme, Stuttgart, p 89–96
Kloos K, Vogel M (1974) Pathologie der Perinatalperiode. Thieme, Stuttgart
Meessen H, Stochdorph O (1952) Gehirnbefunde bei Morbus coeruleus. Proc 1st Intern Congr Neuropath, Roma. Rosenberg & Sellier, Torino, pp 459–477
Molz G, Hartmann H (1984) Dysmorphism, dysplasia, and anomaly in sudden infant death. N Engl J Med 311:259
Motoi M, Stein H, Lennert K (1980) Demonstration of lysozyme, a1-antichymotrypsin, a1-antitrypsin, albumin, and transferrin with the immunoperoxidase method in lymph node cells. Virchows Arch [B] 35:73–82
Naeye RL (1974) Hypoxemia and the sudden infant death syndrome. Science 186:837–838
Naeye RL (1976) Brain stem and adrenal abonomalities in the sudden-infant-death syndrome. Am J Clin Pathol 66:526–530
Nakamura Y, Nakashima T, Fukuda S, Nakashima H, Hashimoto T (1986) Hypoxic-ischemic brain lesions found in asphyxiating neonates. Acta Pathol Jpn 36:551–563
Nyka WM (1976) Cerebral lesions of mature newborn due to perinatal hypoxia. II. Mothers diseases. Z. Geburtsh Perinat 180:295–299
Oehmichen M (1989) Hirnveränderungen beim plötzlichen Kindstod; eine kritische Übersicht. In Andler W, Trowitsch E, Schläfke ME (eds) Der plötzliche Kindstod. Acron, Berlin New York (in press)
Oehmichen M, Linke P, Zilles K, Saternus KS (1989) Reaction of astrocytes and macrophages in the brain stem of SIDS victims? Clin Neuropathol (in press)
Osserman EF, Lawlor DP (1966) Serum and urinary lysoyzme (muramidase) in monocytic and monomyelocytic leukemia. J Exp Med 124:921–955
Quattrochi JJ, McBride PT, Yates AJ (1985) Brain stem immaturity in sudden infant death syndrome: a quantitative rapid Golgi study of dendritic spines in 95 infants. Brain Res 325:39–48
Roessmann U, Gambetti P (1986) Pathological reaction of astrocytes in perinatal brain injury. Acta Neuropathol (Berl) 70:302–307
Roessmann U, Gambetti P (1986) Astrocytes in the developing human brain. Acta Neuropathol (Berl) 70:308–313
Saternus KS, Adam G (1985) Der plötzliche Kindstod. Postmortale Flußmessugnen an den großen Halsgefäßen zum Nachweis der lageabhängigen zerebralen Hypoxämie. Dtsch Med Wochenschr 110:297–303
Schneck SA, Neuburger KT (1962) Lesions of the brain in hyaline membrane disease of infants. Acta Neuropathol (Berl) 2:11–23
Steinschneider A (1972) Prolonged apnoe and the sudden infant death syndrome: clinical and laboratory observations. Pediatrics 50:646–654
Sternberger LA (1979) Immunocytochemistry. Wiley & Sons, New York Chichester Brisbane Toronto
Takashima S, Armstrong D, Becker L, Bryan C (1978) Cerebral hypoperfusion in the sudden infant death syndrome? Brain stem gliosis and vasculature. Ann Neurol 4:257–262
Takashima S, Armstrong D, Becker LE, Huber J (1978) Cerebral white matter lesions in sudden infant death syndrome. Pediatrics 62:155–159
Takashima S, Mito T, Becker LE (1985) Neuronal development in the medullary reticular formation in sudden infant death syndrome and premature infants. Neuropediatrics 16:76–79
Taylor CR, Kledzik G (1981) Immunohistologic techniques in surgical pathology — A spectrum of “new” special stains. Hum Pathol 12:590–596
Uchimura Y (1929) Über die Blutversorgung der Kleinhirnrinde und ihre Bedeutung für die Pathologie des Kleinhirns. Z Gesamte Neurol Psychiatr 120:774–783
Valdes-Dapena M (1986) Sudden infant death syndrome. Morphology update for forensic pathologists — 1985. Forensic Sci Int 30:177–186
Van Beek JHGM, Berkenbosch A, DeGoese J, Olievier CN (1984) Effects of brain stem hypoxemia on the regulation of breathing. Respir Physiol 57:171–188
Vawter GF, Kosakewich H (1983) Aspects of morphologic variations amongst SIDS victims. In: Tildon JT, Roeder LM, Steinschneider A (eds) Sudden infant death syndrome. Academic Press, New York, pp 133–144
Veith G (1966) Probleme des frühkindlichen Hirnschadens aus der Sicht des Morphologen. In: Elert R, Hüter KA (eds) Die Prophylaxe frühkindlicher Hirnschäden. Thieme, Stuttgart, pp 4–15
Viehweg B (1972) Pulmonale hyaline Membranen und Kleinhirnveränderungen bei Neugeborenen. Zentralbl Allg Pathol 116:538–542
Wilske J (1984) Der plötzliche Säuglingstod (SIDS). Morphologische Abgrenzung, Pathomechanismus und Folgerungen für die Praxis. Springer, Berlin Heidelberg New York Tokyo
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Oehmichen, M., Wullen, B., Zilles, K. et al. Cytological investigations on the cerebellar cortex of sudden infant death victims. Acta Neuropathol 78, 404–409 (1989). https://doi.org/10.1007/BF00688177
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00688177