Abstract
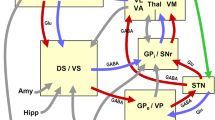
Movement disorders according to clinical phenomenology are divided into hypokinetic (Parkinson’s disease, dementia with Lewy bodies, multiple system atrophy), hyperkinetic (chorea, dyskinesias, tremor), atactic (spinocerebellar, Friedreich’s ataxia), and motor neuron disorders. Only the first two are considered. Most are caused by the dysfunction of the basal ganglia, which work in tandem with the cortex via complex (corticobasal ganglia/thalamocortical) circuits, although virtually the entire nervous system is engaged in motor control. Recent progress provided insight into their pathogenesis and molecular pathology. Many are neurodegenerative proteinopathies, classified into synucleinopathies, tauopathies, polyglutamine repeat, and other disorders. This is a brief overview of the neuropathology of major forms.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Jellinger KA. Neuropathology of movement disorders. In: Winn HR, editor. Youmans neurological surgery, vol. 1. 7th ed. Philadelphia: Elsevier-Saunders; 2016. p. e83.1–41.
Jellinger KA. Neuropathology of sporadic Parkinson’s disease: evaluation and changes of concepts. Mov Disord. 2012;27:8–30.
Del Tredici K, Braak H. Review: sporadic Parkinson’s disease: development and distribution of alpha-synuclein pathology. Neuropathol Appl Neurobiol. 2016;42:33–50.
Bellucci A, Mercuri NB, Venneri A, Faustini G, Longhena F, Pizzi M, et al. Review: Parkinson’s disease: from synaptic loss to connectome dysfunction. Neuropathol Appl Neurobiol. 2016;42:77–94.
Kordower JH, Olanow CW, Dodiya HB, Chu Y, Beach TG, Adler CH, et al. Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain. 2013;136:2419–31.
Wakabayashi K, Tanji K, Odagiri S, Miki Y, Mori F, Takahashi H. The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol Neurobiol. 2013;47:495–508.
Dickson DW. Parkinson’s disease and parkinsonism: neuropathology. Cold Spring Harb Perspect Med. 2012;2, a009258.
Lue L-F, Walker DG, Adler CH, Shill H, Tran H, Akiyama H, et al. Biochemical increase in phosphorylated a-synuclein precedes histopathology of Lewy-type synucleinopathies. Brain Pathol. 2012;22:745–56.
Jellinger KA. Synuclein and Parkinson’s disease: an update. In: Martinez A, Gil C, editors. Emerging drugs and targets for Parkinson’s disease. London: The Royal Society of Chemistry; 2013. p. 175–216.
Alafuzoff I, Ince PG, Arzberger T, Al-Sarraj S, Bell J, Bodi I, et al. Staging/typing of Lewy body related alpha-synuclein pathology: a study of the BrainNet Europe Consortium. Acta Neuropathol. 2009;117:635–52.
Jellinger KA. Neuropathobiology of non-motor symptoms in Parkinson disease. J Neural Transm (Vienna). 2015;122:1429–40.
Halliday G, McCann H, Shepherd C. Evaluation of the Braak hypothesis: how far can it explain the pathogenesis of Parkinson’s disease? Expert Rev Neurother. 2012;12:673–86.
Beach TG, Adler CH, Lue L, Sue LI, Bachalakuri J, Henry-Watson J, et al. Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol. 2009;117:613–34.
Walker Z, Possin KL, Boeve BF, Aarsland D. Lewy body dementias. Lancet. 2015;386:1683–97.
Walker L, McAleese KE, Thomas AJ, Johnson M, Martin-Ruiz C, Parker C, et al. Neuropathologically mixed Alzheimer’s and Lewy body disease: burden of pathological protein aggregates differs between clinical phenotypes. Acta Neuropathol. 2015;129:729–48.
Halliday GM, Song YJ, Harding AJ. Striatal beta-amyloid in dementia with Lewy bodies but not Parkinson’s disease. J Neural Transm. 2011;118:713–9.
Fanciulli A, Wenning GK. Multiple-system atrophy. N Engl J Med. 2015;372:249–63.
Ahmed Z, Asi YT, Sailer A, Lees AJ, Houlden H, Revesz T, et al. The neuropathology, pathophysiology and genetics of multiple system atrophy. Neuropathol Appl Neurobiol. 2012;38:4–24.
Jellinger KA. Neuropathology of multiple system atrophy: new thoughts about pathogenesis. Mov Disord. 2014;29:1720–41.
Kruer MC. The neuropathology of neurodegeneration with brain iron accumulation. Int Rev Neurobiol. 2013;110:165–94.
Li A, Paudel R, Johnson R, Courtney R, Lees AJ, Holton JL, et al. Pantothenate kinase-associated neurodegeneration is not a synucleinopathy. Neuropathol Appl Neurobiol. 2013;39:121–31.
Lashley T, Rohrer JD, Mead S, Revesz T. Review: an update on clinical, genetic and pathological aspects of frontotemporal lobar degenerations. Neuropathol Appl Neurobiol. 2015;41:858–81.
Irwin DJ, Brettschneider J, McMillan CT, Cooper F, Olm C, Arnold SE, et al. Deep clinical and neuropathological phenotyping of Pick disease. Ann Neurol. 2016;79:272–87.
Tatsumi S, Uchihara T, Aiba I, Iwasaki Y, Mimuro M, Takahashi R, et al. Ultrastructural differences in pretangles between Alzheimer disease and corticobasal degeneration revealed by comparative light and electron microscopy. Acta Neuropathol Commun. 2014;2:161.
Halliday G, Bigio EH, Cairns NJ, Neumann M, Mackenzie IR, Mann DM. Mechanisms of disease in frontotemporal lobar degeneration: gain of function versus loss of function effects. Acta Neuropathol. 2012;124:373–82.
Rub U, Vonsattel JP, Heinsen H, Korf HW. The Neuropathology of Huntington s disease: classical findings, recent developments and correlation to functional neuroanatomy. Adv Anat Embryol Cell Biol. 2015;217:1–146.
Govert F, Schneider SA. Huntington’s disease and Huntington’s disease-like syndromes: an overview. Curr Opin Neurol. 2013;26:420–7.
Tsuji S. Dentatorubral-pallidoluysian atrophy. Handb Clin Neurol. 2012;103:587–94.
Kara E, Hardy J, Houlden H. The pallidopyramidal syndromes: nosology, aetiology and pathogenesis. Curr Opin Neurol. 2013;26:381–94.
Bandmann O, Weiss KH, Kaler SG. Wilson’s disease and other neurological copper disorders. Lancet Neurol. 2015;14:103–13.
Jinnah HA, Teller JK, Galpern WR. Recent developments in dystonia. Curr Opin Neurol. 2015;28:400–5.
Paudel R, Hardy J, Revesz T, Holton JL, Houlden H. Review: genetics and neuropathology of primary pure dystonia. Neuropathol Appl Neurobiol. 2012;38:520–34.
Albanese A, Bhatia K, Bressman SB, Delong MR, Fahn S, Fung VS, et al. Phenomenology and classification of dystonia: a consensus update. Mov Disord. 2013;28:863–73.
Govert F, Deuschl G. Tremor entities and their classification: an update. Curr Opin Neurol. 2015;28:393–9.
Louis ED. Essential tremor: from bedside to bench and back to bedside. Curr Opin Neurol. 2014;27:461–7.
Jellinger KA. Neuropathology of essential tremor. J Mult Scler. 2016;3:165.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer-Verlag Wien
About this chapter
Cite this chapter
Jellinger, K.A. (2017). Neuropathology of Movement Disorders. In: Falup-Pecurariu, C., Ferreira, J., Martinez-Martin, P., Chaudhuri, K. (eds) Movement Disorders Curricula. Springer, Vienna. https://doi.org/10.1007/978-3-7091-1628-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-7091-1628-9_5
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-1627-2
Online ISBN: 978-3-7091-1628-9
eBook Packages: MedicineMedicine (R0)