Abstract
Introduction
Trauma resuscitation at dedicated trauma centers typically consist of ad-hoc teams performing critical tasks in a time-limited manner. This creates a high stakes environment apt or avoidable errors. Reporting of errors in trauma resuscitation is generally center-dependent and lacks common terminology.
Methods
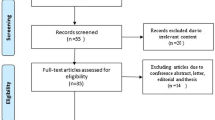
We conducted a systematic review by searching Ovid Medline, Scopus and Embase from inception to February 24, 2021 for errors in adult trauma resuscitation. English studies published after 2001 were included. Studies were assessed by two independent reviewers for meeting inclusion/exclusion criteria. Errors were characterized from the included studies and a summary table was developed. Our review was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42020152875).
Results
The literature search retrieved 4658 articles with 26 meeting eligibility criteria. Errors were identified by morbidity and mortality rounds or other committee in 62%, missed injuries on tertiary assessment or radiology review in 12%, deviations from algorithmic guidelines in 12% or predefined for chest tube complications, critical incident reporting, aspiration or delays in care. In total there were 39 unique error types identified and divided into 9 categories including Emergency Medical Services handover, airway, assessment of injuries, patient monitoring and access, transfusion/blood related, management of injuries, team communication/dynamics, procedure error and disposition.
Conclusions
Overall, our systematic review identified 39 unique error types in trauma resuscitation. Identifying these errors is imperative in developing systems for improvement of trauma care.
Résumé
Introduction
La réanimation des traumatisés dans les centres de traumatologie spécialisés consiste généralement en des équipes ad hoc qui effectuent des tâches critiques dans un temps limité. Cela crée un environnement à enjeux élevés susceptible de provoquer des erreurs évitables. Le signalement des erreurs de réanimation traumatologique dépend généralement du centre et manque de terminologie commune
Méthodes
Nous avons effectué une revue systématique en recherchant dans Ovid Medline, Scopus et Embase, du début au 24 février 2021, des erreurs de réanimation traumatologique chez l'adulte. Les études anglaises publiées après 2001 ont été incluses. Deux examinateurs indépendants ont évalué les études pour déterminer si elles répondaient aux critères d’inclusion et d’exclusion. Les erreurs ont été caractérisées à partir des études incluses et un tableau récapitulatif a été élaboré. Notre étude a été enregistrée de manière prospective dans l'International Prospective Register of Systematic Reviews (PROSPERO) (CRD42020152875).
Résultats
La recherche documentaire a permis d'extraire 4658 articles, dont 26 répondaient aux critères d'admissibilité. Les erreurs ont été identifiées par les rondes de morbidité et de mortalité ou par un autre comité dans 62% des cas, les blessures manquées lors de l'évaluation tertiaire ou de l'examen radiologique dans 12% des cas, les déviations par rapport aux directives algorithmiques dans 12% des cas ou prédéfinies pour les complications du tube thoracique, le signalement des incidents critiques, l'aspiration ou les retards dans les soins. Au total, 39 types d'erreurs uniques ont été identifiés et répartis en 9 catégories : transfert des services médicaux d'urgence, voies respiratoires, évaluation des blessures, surveillance et accès du patient, transfusion/sang, gestion des blessures, communication/dynamique de l'équipe, erreur de procédure et disposition.
Conclusions
Dans l'ensemble, notre étude systématique a identifié 39 types d'erreurs uniques dans la réanimation des traumatismes. L'identification de ces erreurs est impérative pour développer des systèmes d'amélioration des soins en traumatologie.

Similar content being viewed by others
Availability of data and material
Search strategy available in Appendix B.
References
Haas B, Stukel TA, Gomez D, Zagorski B, De Mestral C, Sharma SV, et al. The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. J Trauma Acute Care Surg. 2012;72(6):1510–7.
Haas B, Jurkovich GJ, Wang J, Rivara FP, MacKenzie EJ, Nathens AB. Survival advantage in trauma centers: expeditious intervention or experience? J Am Coll Surg. 2009;208(1):28–36.
Nolan B, Tien H, Sawadsky B, Rizoli S, McFarlan A, Phillips A, et al. Comparison of helicopter emergency medical services transport types and delays on patient outcomes at two level I trauma centers. Prehospital Emerg Care. 2017;21(3):327–33.
Davis JW, Hoyt DB, McArdle MS, Mackersie RC, Shackford SR, Eastman AB. The significance of critical care errors in causing preventable death in trauma patients in a trauma system. J Trauma - Inj Infect Crit Care. 1991;31(6):813–9.
Shackford SR, Hollingworth-Fridlund P, Cooper GF, Eastman AB. The effect of regionalization upon the quality of trauma care as assessed by concurrent audit before and after institution of a trauma system: a preliminary report. J Trauma - Inj Infect Crit Care. 1986;26(9):812–20.
Adedeji OA, Driscoll PA. The trauma team–a system of initial trauma care. Postgrad Med J. 1996;72:587–93.
Speck RM, Jones G, Barg FK, McCunn M. Team composition and perceived roles of team members in the trauma bay. J Trauma Nurs. 2012;19(3):133–8.
Fitzgerald M, Cameron P, Mackenzie C, Farrow N, Scicluna P, Gocentas R, et al. Trauma resuscitation errors and computer-assisted decision support. Arch Surg. 2011;146(2):218–25.
Settervall CHC, Domingues C de A, de Sousa RMC, Nogueira L de S. Preventable trauma deaths, vol. 46, Revista de Saude Publica. Faculdade de Saúde Pública da Universidade de São Paulo; 2012. p. 367–75.
Vioque SM, Kim PK, McMaster J, Gallagher J, Allen SR, Holena DN, et al. Classifying errors in preventable and potentially preventable trauma deaths: A 9-year review using the Joint Commission’s standardized methodology. Am J Surg. 2014;208(2):187–94.
Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006;244(3):371–80.
O’Reilly D, Mahendran K, West A, Shirley P, Walsh M, Tai N. Opportunities for improvement in the management of patients who die from haemorrhage after trauma. Br J Surg. 2013;100(6):749–55.
Sanddal TL, Esposito TJ, Whitney JR, Hartford D, Taillac PP, Mann NC, et al. Analysis of preventable trauma deaths and opportunities for trauma care improvement in utah. J Trauma. 2011;70(4):970–7.
Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007;63(6):1338–47.
Ivatury RR, Guilford K, Malhotra AK, Duane T, Aboutanos M, Martin N. Patient safety in trauma: Maximal impact management errors at a level I trauma center. J Trauma Inj Infect Crit Care. 2008;64(2):265–70.
The American College of Surgeons. Advanced trauma life support (ATLS®) Student Course Manual: the ninth edition. J Trauma Acute Care Surg. 2013;74(5):1363–6.
Kahol K, Vankipuram M, Patel VL, Smith ML. Deviations from protocol in a complex Trauma environment: Errors or innovations? J Biomed Inform. 2011;44(3):425–31.
Chang A, Schyve PM, Croteau RJ, O’leary DS, Loeb JM. The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Heal Care. 2005;17(2):95–105.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Rev Esp Nutr Humana y Diet. 2016;20(2):148–60.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7): https://doi.org/10.1371/journal.pmed.1000100.
National Institute of Health. National institue of health quality assessment tool for observational cohort and cross-sectional studies. 2017.
Jung JJ, Elfassy J, Jüni P, Grantcharov T. Adverse events in the operating room: definitions, prevalence, and characteristics. a systematic review. World J Surg. 2019;43:2379–92. https://doi.org/10.1007/s00268-019-05048-1.
Hutter MM, Rowell KS, Devaney LA, Sokal SM, Warshaw AL, Abbott WM, et al. Identification of surgical complications and deaths: an assessment of the traditional surgical morbidity and mortality conference compared with the american college of surgeons-national surgical quality improvement program. J Am Coll Surg. 2006;203(5):618–24.
Cohen TN, Cabrera JS, Litzinger TL, Captain KA, Fabian MA, Miles SG, et al. Proactive safety management in trauma care: applying the human factors analysis and classification system. J Healthc Qual. 2018;40(2):89–96.
LaGrone LN, McIntyre L, Riggle A, Robinson BRH, Maier RV, Bulger E, et al. Changes in error patterns in unanticipated trauma deaths during 20 years: In pursuit of zero preventable deaths. J Trauma Acute Care Surg. 2020;89(6):1046–53.
Navarro S, Montmany S, Rebasa P, Colilles C, Pallisera A. Impact of ATLS training on preventable and potentially preventable deaths. World J Surg. 2014;38(9):2273–8.
Giannakopoulos GF, Saltzherr TP, Beenen LF, Reitsma JB, Bloemers FW, Goslings JC, et al. Missed injuries during the initial assessment in a cohort of 1124 level-1 trauma patients. Injury. 2012;43(9):1517–21.
Schoeneberg C, Schilling M, Hussmann B, Schmitz D, Lendemans S, Ruchholtz S. Preventable and potentially preventable deaths in severely injured patients: a retrospective analysis including patterns of errors. Eur J Trauma Emerg Surg. 2017;43(4):481–9.
Montmany S, Pallisera A, Rebasa P, Campos A, Colilles C, Luna A, et al. Preventable deaths and potentially preventable deaths. What are our errors? Injury. 2016;47(3):669–73.
Nolan B, Hicks C, Petrosoniak A, Jung J, Grantcharov T. Pushing boundaries of video review in trauma: using comprehensive data to improve the safety of trauma care. Trauma Surg Acute Care Open. 2020;5(1):e000510.
Long AM, Lefebvre CM, Masneri DA, Mowery NT, Chang MC, Johnson JE, et al. The golden opportunity: multidisciplinary simulation training improves trauma team efficiency. J Surg Educ. 2019;76(4):1116–21.
Girard E, Jegousso Q, Boussat B, Francois P, Ageron FX, Letoublon C, et al. Preventable deaths in a French regional trauma system: a 6-year analysis of severe trauma mortality. J Visc Surg. 2019;156(1):10–6.
Campbell SM, Braspenning J, Hutchinson A, Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual Saf Heal Care. 2002;11:358–64.
Fernald DH, Pace WD, Harris DM, West DR, Main DS, Westfall JM. Event reporting to a primary care patient safety reporting system: a report from the ASIPS collaborative. Ann Fam Med. 2004;2(4):327–32.
Bosma E, Veen EJ, Roukema JA. Incidence, nature and impact of error in surgery. Br J Surg. 2011;98(11):1654–9.
DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the va national center for patient safety’s prospective risk analysis system. Jt Comm J Qual Improv. 2002;28(5):248–67.
Acknowledgements
The authors would like to thank David Lightfoot, information specialist at St. Michael’s Hospital, for his assistance with the literature search and development of the search strategy.
Funding
There was no specific funding used for this study from any agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AN participated in the literature search, data collection, data analysis, data interpretation, study design and writing of the manuscript, AQ participated in the data collection and data analysis. JJ participated in the study design, data interpretation and critical revision. BN participated in the study design, data analysis, data interpretation, writing and critical revision.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethics approval
None required for systematic review.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nikouline, A., Quirion, A., Jung, J.J. et al. Errors in adult trauma resuscitation: a systematic review. Can J Emerg Med 23, 537–546 (2021). https://doi.org/10.1007/s43678-021-00118-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-021-00118-7