Abstract
Study design
Prospective radiographic study.
Objectives
To determine the three-dimensional (3D) changes in deformity correction with magnetically controlled growing rod (MCGR) distractions.
Summary of background data
MCGRs can achieve similar coronal plane correction as traditional growing rods. The changes in the sagittal and axial planes are unknown and should be studied as these factors reflect potential for proximal junctional kyphosis and rotational deformity. Frequent MCGR distractions may potentially improve axial plane deformities to the same extent as coronal and sagittal plane deformities.
Methods
Early onset scoliosis (EOS) patients who underwent dual MCGRs with minimum 2-year follow-up were included in this study. 3D reconstructions of 6-monthly biplanar images were used to study changes in coronal, sagittal and axial planes. Changes in growth parameters (body height and arm span) were scaled to changes in coronal Cobb angles, sagittal profile (T1–12, T4–12, L1–L5, L1–S1), and rotational profile at the proximal thoracic, main thoracic and lumbar curves, and pelvic parameters (sagittal pelvic tilt, lateral pelvic tilt and pelvis rotation).
Results
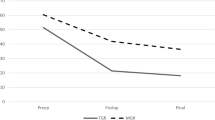
A total of 10 EOS patients were studied. The mean age at index surgery was 8.2 ± 3.0 years and mean postoperative follow-up of 34.3 ± 9.5 months. Six patients had rod exchange at mean 29.5 ± 11.8 months after initial implantation. Despite consistent gains in body height and arm span, the main changes in coronal and rotational profiles only occurred at the initial rod implantation surgery with only small changes occurring with subsequent follow-ups. Patients with higher preoperative proximal junctional angles had flattening of the sagittal plane occurring at initial surgery with early rebound. No changes in pelvic parameters were observed.
Conclusions
The 3D changes with MCGR are mainly observed with initial rod implantation and no significant changes are observed with distractions. The MCGR can prevent deformity progression in the axial plane.
Level of evidence
IV


Similar content being viewed by others
References
Akbarnia BA, Emans JB (2010) Complications of growth-sparing surgery in early onset scoliosis. Spine (Phila Pa 1976) 35:2193–2204
Bess S, Akbarnia BA, Thompson GH et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 92:2533–2543
Redding GJ, Mayer OH (2011) Structure-respiration function relationships before and after surgical treatment of early-onset scoliosis. Clin Orthop Relat Res 469:1330–1334
Akbarnia BA, Breakwell LM, Marks DS et al (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine (Phila Pa 1976) 33:984–990
Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine (Phila Pa 1976) 30:S46–57
Winter RB, Moe JH, Lonstein JE (1984) Posterior spinal arthrodesis for congenital scoliosis. An analysis of the cases of two hundred and ninety patients, five to nineteen years old. J Bone Joint Surg Am 66:1188–1197
Bess S, Akbarnia BA, Thompson GH et al (2011) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 92:2533–2543
Cheung KM, Cheung JP, Samartzis D et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379:1967–1974
Akbarnia BA, Cheung K, Noordeen H et al (2013) Next generation of growth-sparing techniques: preliminary clinical results of a magnetically controlled growing rod in 14 patients with early-onset scoliosis. Spine (Phila Pa 1976) 38:665–670
Cheung JP, Cheung KM (2019) Current status of the magnetically controlled growing rod in treatment of early-onset scoliosis: what we know after a decade of experience. J Orthop Surg 27:2309499019886945
Cheung JP, Cahill P, Yaszay B, Akbarnia BA, Cheung KM (2015) Special article: update on the magnetically controlled growing rod: tips and pitfalls. J Orthop Surg (Hong Kong) 23:383–390
Cheung JPY, Yiu K, Kwan K, Cheung KMC (2019) Mean 6-year follow-up of magnetically controlled growing rod patients with early onset scoliosis: a glimpse of what happens to graduates. Neurosurgery 84:1112–1123
Cheung JPY, Yiu KKL, Samartzis D, Kwan K, Tan BB, Cheung KMC (2018) Rod lengthening with the magnetically controlled growing rod: factors influencing rod slippage and reduced gains during distractions. Spine (Phila Pa 1976) 43:E399–E405
Heydar AM, Sirazi S, Bezer M (2016) Magnetic controlled growing rods (MCGR) As a treatment of early onset scoliosis (EOS): early results with two patients had been fused. Spine (Phila Pa 1976) 41:E1336–E1342
Teoh KH, Winson DM, James SH et al (2016) Magnetic controlled growing rods for early-onset scoliosis: a 4-year follow-up. Spine J 16:S34–S39
Cheung JP, Samartzis D, Cheung KM (2014) A novel approach to gradual correction of severe spinal deformity in a pediatric patient using the magnetically-controlled growing rod. Spine J 14:e7–13
Kwan KYH, Cheung JPY, Yiu KKL, Cheung KMC (2018) Ten year follow-up of Jarcho-Levin syndrome with thoracic insufficiency treated by VEPTR and MCGR VEPTR hybrid. Eur Spine J 27:287–291
Cheung JP, Bow C, Samartzis D, Ganal-Antonio AK, Cheung KM (2016) Clinical utility of ultrasound to prospectively monitor distraction of magnetically controlled growing rods. Spine J 16:204–209
Cheung JPY, Yiu KKL, Bow C, Cheung PWH, Samartzis D, Cheung KMC (2017) Learning curve in monitoring magnetically controlled growing rod distractions with ultrasound. Spine (Phila Pa 1976) 42:1289–1294
Charroin C, Abelin-Genevois K, Cunin V et al (2014) Direct costs associated with the management of progressive early onset scoliosis: estimations based on gold standard technique or with magnetically controlled growing rods. Orthop Traumatol Surg Res 100:469–474
Rushton PRP, Siddique I, Crawford R, Birch N, Gibson MJ, Hutton MJ (2017) Magnetically controlled growing rods in the treatment of early-onset scoliosis: a note of caution. Bone Joint J 99:708–713
Wong CKH, Cheung JPY, Cheung PWH, Lam CLK, Cheung KMC (2017) Traditional growing rod versus magnetically controlled growing rod for treatment of early onset scoliosis: cost analysis from implantation till skeletal maturity. J Orthop Surg (Hong Kong) 25:2309499017705022
Gunzburg R, Gunzburg J, Wagner J, Fraser RD (1991) Radiologic interpretation of lumbar vertebral rotation. Spine 16:660–664
Lopez-Sosa F, Guille JT, Bowen JR (1995) Rotation of the spine in congenital scoliosis. J Pediatr Orthop 15:528–534
Perdriolle R, Vidal J (1985) Thoracic idiopathic scoliosis curve evolution and prognosis. Spine (Phila Pa 1976) 10:785–791
Krismer M, Sterzinger W, Haid C, Frischhut B, Bauer R (1996) Axial rotation measurement of scoliotic vertebrae by means of computed tomography scans. Spine (Phila Pa 1976) 21:576–581
Lam GC, Hill DL, Le LH, Raso JV, Lou EH (2008) Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis 3:16
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine (Phila Pa 1976) 32:568–573
Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31:681–687
Obid P, Yiu KKL, Cheung KM, Kwan K, Ruf M, Cheung JPY (2018) Reliability of rod lengthening, thoracic, and spino-pelvic measurements on biplanar stereoradiography in patients treated with magnetically controlled growing rods. Spine (Phila Pa 1976) 43:1579–1585
Glaser DA, Doan J, Newton PO (2012) Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976) 37:1391–1397
Deschenes S, Charron G, Beaudoin G et al (2010) Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 35:989–994
Pomero V, Mitton D, Laporte S, de Guise JA, Skalli W (2004) Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) 19:240–247
Ilharreborde B, Steffen JS, Nectoux E et al (2011) Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976) 36:E1306–E1313
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Cohen J, Cohen P, West SG, Aiken LS (2003) Applied multiple regression/correlation analysis for the behavioral sciences, 3rd edn. Lawrence Erlbaum Associates, Hillsdale
Acaroglu E, Yazici M, Alanay A, Surat A (2002) Three-dimensional evolution of scoliotic curve during instrumentation without fusion in young children. J Pediatr Orthop 22:492–496
Kamaci S, Demirkiran G, Ismayilov V, Olgun ZD, Yazici M (2014) The effect of dual growing rod instrumentation on the apical vertebral rotation in early-onset idiopathic scoliosis. J Pediatr Orthop 34:607–612
Sangole AP, Aubin CE, Labelle H et al (2009) Three-dimensional classification of thoracic scoliotic curves. Spine (Phila Pa 1976) 34:91–99
Luk KD, Cheung WY, Wong Y, Cheung KM, Wong YW, Samartzis D (2012) The predictive value of the fulcrum bending radiograph in spontaneous apical vertebral derotation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 37:E922–E926
Luk KD, Vidyadhara S, Lu DS, Wong YW, Cheung WY, Cheung KM (2010) Coupling between sagittal and frontal plane deformity correction in idiopathic thoracic scoliosis and its relationship with postoperative sagittal alignment. Spine (Phila Pa 1976) 35:1158–1164
Yao G, Cheung JPY, Shigematsu H et al (2017) Characterization and predictive value of segmental curve flexibility in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976) 42:1622–1628
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned reoperations in magnetically controlled growing rod surgery for early onset scoliosis with a minimum of two-year follow-Up. Spine (Phila Pa 1976) 42:E1410–E1414
Lebon J, Batailler C, Wargny M et al (2017) Magnetically controlled growing rod in early onset scoliosis: a 30-case multicenter study. Eur Spine J 26:1567–1576
Funding
This study was supported by the Scoliosis Research Society.
Author information
Authors and Affiliations
Contributions
JPYC—Study conception and design, data acquisition, analysis, interpretation of data, drafting manuscript. PWHC—Data acquisition and analysis, interpretation of data, revising manuscript. KMCC—Interpretation of data, revising manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no financial or competing interests to disclose.
Ethical approval
Permission to reproduce copyrighted materials or signed patient consent forms granted. The study was approved by the local institutional review board (UW 16-336).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheung, J.P.Y., Cheung, P.W.H. & Cheung, K.M.C. The effect of magnetically controlled growing rods on three-dimensional changes in deformity correction. Spine Deform 8, 537–546 (2020). https://doi.org/10.1007/s43390-020-00055-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00055-y