Abstract
Background
The LACE index scoring tool (Length of stay, Acuity of admission, Co-morbidities and Emergency department visits) has been designed to predict hospital readmissions. We evaluated the ability of the LACE index to predict age-specific frequent admissions and mortality.
Methods
Analysis of prospectively collected data of alive-discharge episodes between 01/04/2017 and 31/03/2019 in an NHS hospital. Data on 14,878 men and 17,392 women of mean age 64.0 years, SD = 20.5, range 18.0–106.7 years were analysed. The association of the LACE index with frequency of all-cause readmissions within 28 days of discharge and over a 2-year period, and with all-cause mortality within 30 days or within 6 months after discharge from hospital were evaluated.
Results
Within LACE index scores of 0–4, 5–9 or ≥ 10, the proportions of readmission ≥ 2 times within 28 days of discharge were 0.1, 1.3 and 9.2% (χ2 = 3070, p < 0.001) and over a 2-year period were 1.7, 4.8 and 19.1% (χ2 = 3364, p < 0.001). Compared with a LACE index score of 0–4, a score ≥ 10 increased the risk (adjusted for age, sex and frequency of admissions) of death within 6 months of discharge by 6.8-fold (5.1–9.0, p < 0.001) among all ages, and most strongly in youngest individuals (18.0–49.9 years): adjusted odds ratio = 16.1 (5.7–45.8, p < 0.001). For those aged 50–59.9, 60–69.9, 70–79.9 and ≥ 80 years, odds ratios reduced progressively to 9.6, 7.7, 5.1 and 2.3, respectively. Similar patterns were observed for the association of LACE index with mortality within 30 days of hospital discharge.
Conclusions
The LACE index predicts short-term and long-term frequent admissions and short-term and medium-term mortality, most pronounced among younger individuals, after hospital discharge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healthcare services are continually overstretched due to increasing demand, primarily from an expanding ageing population living with multiple chronic conditions and disabilities [1,2,3]. Many such individuals have frequent early hospital readmissions [4] and prolonged length of stay in hospital [5, 6], imposing a high pressure on healthcare systems [7, 8]. Information on the number of individuals with high risk of readmission and mortality would allow healthcare teams to formulate effective clinical plans and resources. The LACE index scoring tool, based on Length of stay, Acuity of admission, Co-morbidities and Emergency department visits, has been designed to predict early hospital readmissions and death [9] and has been implemented widely across hospitals in the UK and in many other countries [10,11,12,13,14].
The LACE index represents a cluster of features that indicate the health status of an individual; the higher the index score, the poorer is their health and a greater risk of death. The role of the LACE index in relation to admissions and mortality has been explored, but studies tend to focus primarily on older individuals and short periods after discharge from hospital (up to about one month) before readmission [14, 15], or death [10,11,12,13,14]. Among the overall population in England and Wales, the proportions of younger adults aged 18–29, 30–39, 40–49 and 50–59 years are 16.2, 13.3, 14.6 and 12.1%, while the respective proportions of older adults aged 60–69, 70–79 and over 80 years are lower, are 10.8, 7.1 and 4.6% [16]. However, there is a paucity of data on the ability of the LACE index to predict age-specific mortality occurring after discharge and at times greater than one month after discharge, and frequent readmissions over a prolonged period [17]. In this study, we quantify the ability of the LACE index to predict, in adults aged between 18 and 107 years, the risk of all-cause frequent unplanned readmissions (within 28 days of discharge) and multiple readmissions over a period of two years, and also to predict the risk of all-cause mortality within 30 days or within six months of discharge from hospital.
Methods
Study design, participants and setting
Data of consecutive alive-discharge episodes over two years between 1st April 2017 and 31st March 2019 in a single National Health Service hospital were prospectively collected. The data comprised clinical characteristics and care quality including age, sex, primary diagnosis on admission, the length of stay in hospital, nature of the admission, co-morbidities and number of previous emergency department visits.
Measurement
Co-morbidities were coded according to ICD-10 for calculation of the Charlson co-morbidity index [18, 19]. Information on the frequency of unplanned admissions and readmissions within 28 days and over a two-year period, and mortality within 30 days and up to six months after hospital discharge was recorded. Cancer and obstetrics spells were excluded in line with the NHS data collection for general hospital admissions [20].
The LACE index was computed (https://www.mdcalc.com/lace-index-readmission) from length of stay (score range 0–7), acuity of admission (score 0 or 3), co-morbidity (score range 0–5), emergency department visits (score range 0 or 4) with the scale ranging from 0 to 19 and the likelihood of outcome risk (mortality) is raised with increasing score [9].
Categorisation of variables
LACE indices were grouped into low (score = 0–4), moderate (score = 5–9) and high (score ≥ 10) risk [15, 21, 22]. Age was categorised by decades from 50 years old: 50–59.9, 60–69.9, 70–79.9 and ≥ 80 years. All those between 18 and 49.9 years were grouped together due to low mortality rates, while those between 80 and 107 years were combined together due to small numbers – only 2461 (7.6%) patients were older than 90 years. Readmissions within 28 days of discharge or over a period of two financial years were categorised into three groups: No readmission, readmitted once, and readmitted ≥ 2 times.
Statistical analysis
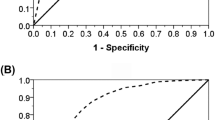
Chi-square tests were used to assess the relationship between the proportions of all-cause readmissions and rates of all-cause mortality in relation to the LACE index. Receiver operating characteristic (ROC) curves were constructed to determine the area under the curve (AUC) for the LACE index as a predictor of outcomes (mortality or frequent admissions). Cox regression survival analysis and Kaplan–Meier survival curves were constructed to examine the risk of mortality after discharge. Logistic regression was conducted using categories of LACE index scores; 0–4 (reference group), 5–9 and ≥ 10 as the predictor variable of frequent readmissions (≥ 2 times within 28 days of discharge or ≥ 2 times over a 2-year period), or mortality within 30 days or within six months of hospital discharge (dependent variables). For analysis of frequent admissions, data were adjusted for age and sex. For analysis of mortality, data were presented in three models; model 1: unadjusted, model 2: adjusted for age and sex, and model 3: adjusted for age, sex and frequency of admission in all ages first, followed by age-specific analysis. Odds ratios (OR) are given with 95% confidence intervals (CI). Analyses were performed using IBM SPSS Statistics, v23.0 (IBM Corp., Armonk, NY).
Results
Subject characteristics
Data for a total of 32,270 patients (14,878 men) and (17,392 women) aged 18–106.7 yr (mean = 64.0 years, SD = 20.5) were analysed. There were 29.3% of patients with a LACE index score of ≥ 10. A total of 11.6% were readmitted within 28 days (8.1% readmitted once and 3.3% readmitted ≥ 2 times), and 21.6% were readmitted over a 2-year period (13.5% readmitted once and 8.1% readmitted ≥ 2 times). There were 834 (2.6%) and 2192 (6.8%) patients died within 30 days (mean age of death 81.5 years, SD 12.0) and six months of discharge (mean age of death 81.2 years, SD 12.1), respectively (Table 1).
The proportions for those who were readmitted ≥ 2 times within 28 days of discharge were 1.0% (18–49.9 years), 1.5% (50–59.9 years), 2.4% (60–69.9 years), 3.3% (70–79.9 years) and 6.7% (≥ 80 years) (χ2 = 1087, p < 0.001), and for those who were readmitted ≥ 2 times over a 2-yr period were 3.3% (18–49.9 years), 5.1% (50–59.9 years), 6.7% (60–69.9 years), 8.7% (70–79.9 years) and 14.4% (≥ 80 years) (χ2 = 1335, p < 0.001).
The proportions of patients with a LACE index score ≥ 10 also rose steeply with age: 1.7% (18–49.9 years), 5.6% (50–59.9 years), 18.0% (60–69.9 years), 39.1% (70–79.9 years) and 66.6% (80–89.9 years) (χ2 = 15,804, p < 0.001) and with frequency of readmission within 28 days of discharge: 24.5% (no readmission), 59.3% (one readmission) and 82.6% (≥ 2 readmissions) (χ2 = 3070, p < 0.001), and with frequency of readmission over the 2-year period of study: 22.2% (no readmission), 46.0% (one readmission) and 69.1% (≥ 2 readmissions) (χ2 = 3364, p < 0.001).
ROC analysis to generate AUC values showed that the LACE index as a predictor of mortality within six months of hospital discharge was 80.5% (95%CI = 79.7–81.3) and frequent readmissions was 84.0%, (95%CI = 83.0–85.1).
LACE index as predictor of all-cause unplanned readmissions
Within LACE index score groups of 0–4, 5–9 or ≥ 10, the proportions of readmission ≥ 2 times within 28 days of discharge were 0.1, 1.3 and 9.2% (χ2 = 3070, p < 0.001) and over a 2-year period were 1.7, 4.8 and 19.1% (χ2 = 3364, p < 0.001) (Fig. 1). Compared with individuals with a LACE index score of 0–4 (reference group), those with a score of 5–9 had increased risk (adjusted for age and sex) of frequent admissions (≥ 2 times) within 28 days after discharge: OR = 10.4 (95% CI = 5.9–18.5, p < 0.001) and over a 2-yr period: OR = 3.1 (95% CI = 2.6–3.7, p < 0.001). This further increased in those with a score ≥ 10, frequent admissions within 28 days after discharge: OR = 94.2 (95% CI = 53.0–167.4, p < 0.001) and over a 2-yr period OR = 15.3 (95% CI = 12.6–18.6, p < 0.001).
LACE index as predictor of all-cause mortality
The proportions of patients who died within 30 days of discharge rose from 0.1% in the lowest LACE index group (0–4) to 1.4% in intermediate group (5–9) and up to 6.8% in the highest group (≥ 10) (χ2 = 957, p < 0.001). The corresponding figures for those who died within six months of discharge were 0.7, 3.9 and 17.0% (χ2 = 2275, p < 0.001). Compared with a LACE index score = 0–4, a score ≥ 10 increased the risk (adjusted for age, sex and frequency of admissions) of death within three months by 13.5-fold (95%CI = 7.4–24.6, p < 0.001) or within six months of discharge by 6.8-fold (5.1–9.0, p < 0.001).
Compared to those with a LACE index < 4 (mean for survival time from discharge = 32.1 months, 95%CI = 32.0–32.2), those with a LACE index of 4–9 or ≥ 10 had a significantly shorter survival with mean for survival time from discharge = 30.6 (95%CI = 30.5–30.8) and 29.5 (95%CI = 25.0–25.5) months respectively, log rank (Mantel-Cox) test: χ2 = 3382, p < 0.001. The hazard ratio, adjusted for age, sex and frequency of readmissions, was for a LACE index 4–9 = 2.58 (95% CI = 2.11–3.14, p < 0.001) and for a LACE index ≥ 10 = 6.38 (95% CI = 5.21–7.18, p < 0.001) (Fig. 2).
Kaplan–Meier survival plot in patients with a LACE index < 4 (dotted green line), 4–9 (dashed blue line) and ≥ 10 (solid red line). The vertical dotted black line shows the 6-month time for one of the mortality estimates. The table beneath the figure shows the number of at-risk patients at various time points for the three LACE index cohorts
A LACE index predicted mortality most strongly in younger individuals (18–49.9 years): a score ≥ 10 was associated with greater risk of death within 30 days after discharge: OR = 30.5 (95%CI = 4.6–202.9, p < 0.001), and death within six months after discharge: OR = 16.1 (5.7–45.8, p < 0.001). For those aged 50–59.9, 60–69.9, 70–79.9 and ≥ 80 years, ORs reduced to 20.5, 7.5, 15.6 and 5.3 for death within 30 days and to 9.6, 7.7, 5.1 and 2.3 for death within six months after hospital discharge, respectively (Table 2).
Discussion
This study, over a period of 2 years, found a high LACE index was related to all-cause frequent readmissions within 28 days, as well as over a two-year period, after hospital discharge. The same relation was observed for all-cause mortality within 30 days or six months post-hospital discharge. The risk of mortality was most pronounced among younger individuals; patients aged 18–49.9 years with a LACE index score ≥ 10 had a 30.5-fold increased risk of death within 30 days and a 16.1-fold increased risk of death within 6 months of discharge.
Evidence from this study supports the use of a LACE index as a valuable tool for identifying individuals at risk. The proportions of patients with a high LACE index score (≥ 10) are relatively high, but have been reported to range between 16.0–48.5% [13, 21, 22], compared with 29.3% in this study. However we observed that these values vary with age; the proportion of individuals with LACE index scores ≥ 10 was only 1.7% among the youngest group (18–49.9 years) and more than doubled with each following decade of age to a peak level of 69.1% among those aged ≥ 80 years. It is therefore important to take age into account when the rates of patients with high LACE index are analysed or reported.
Our findings of the overall rate (11.6%) of readmissions within 28 days of discharge was similar to that (12.6%) reported by Gruneir et al. [21] and by Lim et al. (11.6%) [23], but lower than the figure (18.4%) reported by Tan et al. [22], probably due to age differences between study populations. The observation of increased risk of frequent readmission among those with LACE index scores ≥ 10 was consistent with previous studies [21, 22]. In this study, we have also found that almost a fifth of patients with LACE index score ≥ 10 to be at risk of multiple readmissions (≥ 2 times) in the long-term (two-year period). These findings provide valuable information to healthcare teams to identify those at long-term risk of readmissions to support preventative and early interventional measures to those who are most vulnerable. This will improve patient care and reduce pressure and costs to healthcare services. Efforts have been made to reduce hospital readmissions such as the Hospital Readmissions Reduction Program (HRRP) in the US but results have been mixed due to increased mortality [24]. It is therefore important to address the balance of benefit and risk of readmissions reduction to avoid missing high risk patients who remain reliant on hospital readmission for necessary treatment.
The mortality rates observed in our study were also comparable to those recently reported for 30 days [25] and 6 months of discharge [26, 27]. There was a clear increasing trend in the risk of mortality from higher LACE index scores in the youngest age group. This trend continued to persist with older age groups but was progressively less pronounced. These increased risks were adjusted for age, sex and frequency of admissions. As far as we are aware, this is the first study to demonstrate an age-specific relationship between the LACE index and mortality and was achieved over a wide range of age (18–107 years). Lowering the cut-off level of a LACE index score for younger individuals may be necessary to identify more patients at high risk of mortality after hospital discharge.
This study also demonstrated that the LACE index has predictive validity for short-term (30-days) and medium-term (6-months) mortality, with clear stepwise increments in mortality. This suggests further research is required to gain greater insights into those younger individuals who have high LACE index scores, to lower their risk of death after discharge from hospital.
The strengths of this study lie in its large number of consecutive patients, which enable us to estimate the risk of mortality by decades of age, ranging from 18 to 107 years. Appropriate adjustments were made including age, sex and frequency of admission. Further adjustment for primary diagnosis on admission did not change these associations. Our hospital is typical of a General District Hospital in the UK. Our previous studies examining other health outcomes, using data from three other hospitals within the same county, showed very similar characteristics and indeed with the rest of the UK [28, 29]. Any bias is therefore likely to be minimal in our study. The present study did not collect information on socioeconomic status, employment or provenience (urban or rural) that could have some bearing on the outcomes. We employed the validated LACE index as a prognostic tool to predict outcome measures while cut-off points of 0–4, 5–9 and ≥ 10 were based on previous studies [15, 21]. These cut-off points are arbitrary therefore raising the score above 10 for the “high-risk” group would identify higher rates of mortality. Conversely lowering the cut-off score below 4 for the “low-risk” group would reduce rates of mortality, thus exaggerating the predictive ability (ORs) of mortality by the LACE index. Further studies to identify age-specific cut-offs for the LACE index as an indicator of adverse outcomes (such as mortality) are required.
In conclusion, the LACE index predicts short-term and long-term frequent admissions and short-term and medium-term mortality, most pronounced among younger individuals, after hospital discharge. Raising awareness of younger individuals with a high LACE score is recommended.
References
Kingston A, Robinson L, Booth H et al (2018) MODEM project. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing 47:374–380
Lisk R, Yeong K, Enwere P et al (2020) Associations of 4AT with mobility, length of stay and mortality in hospital and discharge destination among patients admitted with hip fractures. Age Ageing 49:411–417
Han TS, Fry CH, Gulli G et al (2020) Prestroke disability predicts adverse poststroke outcome: a registry-based prospective cohort study of acute stroke. Stroke 51:594–600
NHS Digital. Archived Emergency readmissions to hospital within 28 days of discharge, financial year 2010/11. https://files.digital.nhs.uk/BB/42FA85/hes-emer-read-hosp-28-days-disc-2001-2011-pra.pdf. Accessed Jan 2020
Bo M, Fonte G, Pivaro F et al (2016) Prevalence of and factors associated with prolonged length of stay in older hospitalized medical patients. Geriatr Gerontol Int 16:314–321
Lisk R, Uddin M, Parbhoo A et al (2019) Predictive model of length of stay in hospital among older patients. Aging Clin Exp Res 31:993–999
Lehnert T, Heider D, Leicht H et al (2011) Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 68:387–420
Hazra NC, Rudisill C, Gulliford MC (2018) Determinants of health care costs in the senior elderly: age, comorbidity, impairment, or proximity to death? Eur J Health Econ 19:831–842
van Walraven C, Dhalla IA, Bell C et al (2010) Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ 182:551–557
Cotter PE, Bhalla VK, Wallis SJ et al (2012) Predicting readmissions: poor performance of the LACE index in an older UK population. Age Ageing 41:784–789
Amarasingham R, Velasco F, Xie B et al (2015) Electronic medical record-based multicondition models to predict the risk of 30 day readmission or death among adult medicine patients: validation and comparison to existing models. BMC Med Inform Decis Mak 15:39
Shaffer BK, Cui Y, Wanderer JP (2019) Validation of the LACE readmission and mortality prediction model in a large surgical cohort: Comparison of performance at preoperative assessment and discharge time points. J Clin Anesth 58:22–26
Hakim MA, Garden FL, Jennings MD et al (2017) Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin Epidemiol 10:51–59
Low LL, Liu N, Ong ME et al (2017) Performance of the LACE index to identify elderly patients at high risk for hospital readmission in Singapore. Medicine (Baltimore) 96:e6728
Wang H, Robinson RD, Johnson C et al (2014) Using the LACE index to predict hospital readmissions in congestive heart failure patients. BMC Cardiovasc Disord 14:97
https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/age-groups/latest [Accessed April 2020]
Damery S, Combes G (2017) Evaluating the predictive strength of the LACE index in identifying patients at high risk of hospital readmission following an inpatient episode: a retrospective cohort study. BMJ Open 7:e016921
Schneeweiss S, Wang PS, Avorn J et al (2003) Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Serv Res 38:1103–1120
Romano PS, Roos LL, Jollis JG (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46:1075–1079
Gruneir A, Dhalla IA, van Walraven C et al (2011) Unplanned readmissions after hospital discharge among patients identified as being at high risk for readmission using a validated predictive algorithm. Open Med 5:e104–111
Tan SY, Low LL, Yang Y et al (2013) Applicability of a previously validated readmission predictive index in medical patients in Singapore: a retrospective study. BMC Health Serv Res 13(1):366
Lim E, Matthew N, Mok W et al (2011) Using hospital readmission rates to track the quality of care in public hospitals in Singapore. BMC Health Serv Res 11:A16
Wadhera RK, Maddox KE, Wasfy JH et al (2018) Association of the Hospital Readmissions Reduction Program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 320:2542–2552
Dharmarajan K, Wang Y, Lin Z et al (2017) Association of changing hospital readmission rates with mortality rates after hospital discharge. JAMA 318:270–278
Mazzola P, Bellelli G, Broggini V et al (2015) Postoperative delirium and pre-fracture disability predict 6-month mortality among the oldest old hip fracture patients. Aging Clin Exp Res 27:53–60
Park LP, Chu VH, Peterson G et al (2016) Validated risk score for predicting 6-month mortality in infective endocarditis. J Am Heart Assoc 5:e003016
Han TS, Fry CH, Fluck D et al (2017) Evaluation of anticoagulation status for atrial fibrillation on early ischaemic stroke outcomes: a registry-based, prospective cohort study of acute stroke care in Surrey, UK. BMJ Open 7(12):e019122
Han TS, Lean MEJ, Fluck D et al (2018) Impact of delay in early swallow screening on pneumonia, length of stay in hospital, disability and mortality in acute stroke patients. Eur J Clin Nutr 72:1548–1554
Acknowledgements
The authors wish to thank patients and all those who were involved in the project.
Funding
None.
Author information
Authors and Affiliations
Contributions
TSH and DF reviewed the topic related literature and performed the study concept and analysis design. EH, KK, BS, RW, GJ, JR, PM and DF performed the study coordination and data collection and commented on the manuscript. TSH wrote the first draft, analysed, interpreted the data and revised the manuscript. CHF edited the manuscript. All authors checked, interpreted results and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study does not require NHS Research Ethics Committee approval since it involves secondary analysis of anonymised data. This study was conducted in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heppleston, E., Fry, C.H., Kelly, K. et al. LACE index predicts age-specific unplanned readmissions and mortality after hospital discharge. Aging Clin Exp Res 33, 1041–1048 (2021). https://doi.org/10.1007/s40520-020-01609-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01609-w