Abstract
Purpose
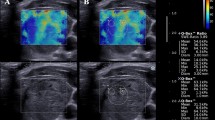
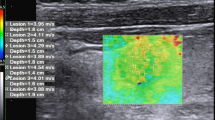
The aim of this study is to assess the diagnostic efficacy and interobserver agreement of acoustic radiation force impulse (ARFI) elasticity imaging in differentiating thyroid nodules.
Methods
In our study, 74 consecutive patients (52 females, 22 males; age range 27–77 years, mean: 41 years) with 82 thyroid nodules (60 benign nodules, and 22 malignant) were examined by two radiologists with different experience. Patients underwent either cytology using fine needle aspiration cytology or thyroid surgery. The diagnostic performance of the two operators at ARFI with sensitivity, specificity, positive predictive and negative predictive value, and ROC curves was estimated. Inter-reader variability between the two operators was defined using Cohen’s k.
Results
According to receiver operating characteristics ROC curves (AUROC = 0.86 for observer 1; 0.81 for observer 2) sensitivity, specificity, PPV and NPV of reader 1 and 2 were respectively: 90, 75, 90.91 and 96.55 %; (cut-off value of shear wave: 2.455 m/s); 90, 72, 90 and 96.90 % (cut-off value shear wave: 2.365 m/s). Concordance between the two operators was good (k = 0.755).
Conclusions
This work is a feasibility study evaluating ARFI imaging. Its results suggest that ARFI imaging is a reproducible method which can be utilized with good diagnostic performance in the thyroid for discriminating benign and malignant nodules using the cut-off value of 2.455 m/s. However, larger studies are needed to validate this method.
Riassunto
Scopo
Lo scopo di questo studio è la valutazione della efficacia diagnostica e della concordanza inter-osservatore dell’imaging elastografico ARFI, per la differenziazione di noduli tiroidei.
Metodo
Nel nostro studio, 74 pazienti consecutivi (52 femmine, 22 maschi; range di età 22–77 anni, età media 41 anni) con 82 noduli tiroidei (60 noduli benigni e 22 maligni), sono stati esaminati da due radiologi con diverso livello di esperienza. I pazienti sono stati sottoposti o a citologia aspirativa con ago sottile (FNAC), o a chirurgia tiroidea. La performance diagnostica dei due operatori all’ ARFI è stata stimata con la sensibilità, la specificità, il valore predittivo positivo (VPP) e negativo (VPN), attraverso le curve ROC (receiver operating characteristics). La variabilità inter-osservatore tra i due operatori, è stata definita usando la kappa di Cohen.
Risultati
Secondo le curve ROC (AUROC = 0.86 per il primo osservatore; 0.81 per il secondo osservatore) la sensibilità, la specificità, il VPP e il VPN per gli osservatori 1 e 2, erano rispettivamente: 90, 75, 90,91, e 96.55 %; (valore medio di shear wave: 2.455 m/s); 90, 72, 90 e 96.90 % (valore medio di shear wave: 2.365 m/s). La concordanza tra I due operatori era buona (k = 0.755).
Conclusioni
Questo lavoro è uno studio preliminare che valuta l’imaging elastografico con Acustic Radiation Force Impulse. I risultati suggeriscono che l’ARFI è un metodo riproducibile che può essere utilizzato con buona performance diagnostica per la differenziazione di noduli benigni e maligni della tiroide, usando come valore di cut-off 2.455 m/s. Comunque, sono necessari studi con più ampia casistica di pazienti per la validazione di questa metodica.




Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Murray T, Xu J et al (2006) Cancer statistics. CA Cancer J Clin 56:106–130
Trimboli P, Condorelli E, Catania A, Sorrenti S (2009) Clinical and ultrasound parameters in the approach to thyroid nodules cytologically classified as indeterminate neoplasm. Diagn Cytopathol 37:783–785
Iannuccilli JD, Cronan JJ, Monchik JM (2004) Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J Ultrasound Med 23:1455–1464
Wienke JR, Chong WK, Fielding JR, Zou KH, Mittelstaedt CA (2003) Sonographic features of benign thyroid nodules: interobserver reliability and overlap with malignancy. J Ultrasound Med 22:1027–1031
Sorrenti S, Trimboli P, Catania A, Ulisse S, De Antoni E et al (2009) Comparison of malignancy rate in thyroid nodules with cytology of indeterminate follicular or indeterminate Hürthle cell neoplasm. Thyroid 19:355–360
Trimboli P, Ulisse S, D’Alò M, Solari F, Fumarola A et al (2008) Analysis of clinical, ultrasound and colour flow-Doppler characteristics in predicting malignancy in follicular thyroid neoplasms. Clin Endocrinol 69:342–344
Tee YY, Lowe AJ, Brand CA, Judson RT (2007) Fine-needle aspiration may miss a third of all malignancny in palpable thyroid nodules: a comprehensive literature review. Ann Surg 246:714–720
Cantisani V, Grazhdani H, Ricci P et al (2013) Q-elastography of solid thyroid nodules: Assessment of diagnostic efficacy and inter observer variability in a large patient cohort. Eur Radiol (Epub ahead of print)
Cantisani V, Lodise P, Grazhdani H et al (2013) Ultrasound elastograhpy in the evaluation of thyroid pathology. Current status. Eur J Radiol (Epub ahead of print)
Ning CP, Jiang SQ, Zhang T, Sun LT, Liu YJ et al (2012) The value of strain ratio in differential diagnosis of thyroid solid nodules. Eur J Radiol 81:286–291
Cantisani V, D’Andrea V, Biancari F, Medvedyeva O, Di Segni M et al (2012) Prospective evaluation of multiparametric ultrasound and quantitative elastosonography in the differential diagnosis of benign and malignant thyroid nodules. Eur J Radiol 81:2678–2683
Cantisani V, Ulisse S, Guaitoli E, De Vito C, Caruso R et al (2012) Q-elastography in the presurgical diagnosis of thyroid nodules with indeterminate cytology. PLoS One 7(11):e50725
Bojunga J, Herrmann E, Meyer G, Weber S, Zeuzem S et al (2010) Real-time elastography for the differentiation of benign and malignant thyroid nodules: a meta-analysis. Thyroid 20:1145–1150
Friederich-Rust M, Romenski O, Meyer G, Dauth N, Holzer K et al (2012) Acoustic radiation force impulse-imaging for the evaluation of the thyroid gland: a limited patient feasibility study. Ultrasonics 52:69–74
Sporea I, Vlad M, Bota S, Sirli RL, Popescu A et al (2011) Thyroid stiffness assessment by acoustic radiation force impulse elastography (ARFI). Ultraschall Med 32:281–285
Gu J, Du L, Bai M, Chen H, Jia X et al (2012) Preliminary study on the diagnostic value of acoustic radiation force impulse technology for differentiating between benign and malignant thyroid nodules. J Ultrasound Med 31:763–771
(1996) Guidelines of the Papanicolaou Society of Cytopathology for the examination of fine-needle aspiration specimens from thyroid nodules. The Papanicolaou Society of Cytopathology task force on standards of practice. Mod Pathol 9:710–715
Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J et al (2005) Thyroid gland tumor diagnosis at US elastography. Radiology 237:202–211
Wilson T, Chen Q, Zagzebski JA, Varghese T, Van Middlesworth L (2006) Initial clinical experience imaging scatterer size and strain in thyroid nodules. J Ultrasound Med 25:1021–1029
Xing P, Wu L, Zhang G, Li S, Liu C et al (2011) Differentiation of benign from malignant thyroid lesions: calculation of the strain ratio on thyroid sonoelastography. J Ultrasound Med 30:663–669
Park SH, Kim SJ, Kim EK, Kim MJ, Son EJ, Kwak JY (2009) Interobserver agreement in assessing the sonographic and elastographic features of malignant thyroid nodules. AJR 193(5):W416–W423
Lim DJ, Luo S, Kim MH, Ko SH, Kim Y (2012) Interobserver agreement and intraobserver reproducibility in thyroid ultrasound elastography. AJR 198:896–901
Cosgrove D, Piscaglia F, Bamber J et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall Med 34:238–53 (also free on line at http://www.efsumb.org)
Shan B, Pelegri AA, Maleke C, Konofagou EE (2008) A mechanical model to compute elastic modulus of tissue for harmonic motion imaging. J Biomech 41:2150–2158
Sumi C (2008) Regularization of tissue shear modulus reconstruction using strain variance. IEEE Trans Ultrason Ferroelectr Freq Control 55:297–307
Garra BS (2011) Elastography: current status, future prospects, and making it work for you. Ultrasound Q 27:177–186
Nightingale K, Bentley R, Trahey G (2002) Observations of tissue response to acoustic radiation force: opportunities for imaging. Ultrason Imaging 24:129–138
Nightingale KR, Palmeri ML, Nightingale RW, Trahey GE (2001) On the feasibility of remote palpation using acoustic radiation force. J Acoust Soc Am 110:625–634
Zhai L, Palmeri ML, Bouchard RR, Nightingale RW, Nightingale KR (2008) An integrated indenter-ARFI imaging system for tissue stiffness quantification. Ultrason Imaging 30:95–111
Fahey BJ, Palmeri ML, Trahey GE (2007) The impact of physiological motion on tissue tracking during radiation force imaging. Ultrasound Med Biol 33:1149–1166
Merino S, Arrazola J, Cárdenas A, Mendoza M, De Miguel P et al (2011) Utility and interobserver agreement of ultrasound elastography in detection of malignant thyroid nodules in clinical care. Am J Neuroradiol 32:2142–2148
Conflict of interest
The authors of this paper, Hektor Grazhdani, Vito Cantisani, Pietro Lodise, Giorgio Di Rocco, Maria Cristina Proietto, Eloisa Fioravanti, Antonello Rubini, Adriano Redler, declare that no fund or grant was received for this research and that there are no relationships/conditions/circumstances that present a potential conflict of interest.
Ethical standard statement
Informed consent was obtained from all patients and the study was performed in accordance with the ethical guidelines of the Helsinki Declaration and approved by the local ethics committee.
Author information
Authors and Affiliations
Corresponding authors
Additional information
H. Grazhdani and V. Cantisani provided an equal contribution.
Rights and permissions
About this article
Cite this article
Grazhdani, H., Cantisani, V., Lodise, P. et al. Prospective evaluation of acoustic radiation force impulse technology in the differentiation of thyroid nodules: accuracy and interobserver variability assessment. J Ultrasound 17, 13–20 (2014). https://doi.org/10.1007/s40477-013-0062-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-013-0062-5