Abstract
The main goal of organ-allocation systems is to guarantee equal access to the limited resource of liver grafts for every patient on the waiting list, striking a balance between the ethical principles of equity, utility, benefit, need, and fairness. The European healthcare scenario is very complex, as it is essentially decentralized, and each nation—and region inside the nation—operates with a significant degree of autonomy. Furthermore, the epidemiology of liver diseases and hepatocarcinoma (HCC) differs between European countries and clearly affects indications and priorities. The aims of this review were to analyze the liver-allocation policies for HCC in different European countries. The European area considered for this analysis included five macro-areas or countries with similar liver-sharing and allocation policies: Centro Nazionale Trapianti (CNT) in Italy; Eurotransplant (Germany, the Netherlands, Belgium, Luxembourg, Austria, Hungary, Slovenia, and Croatia); Organizacion Nacional de Transplantes (ONT) in Spain; Etablissement français des Greffes (EfG) in France; NHS Blood & Transplant (NHSBT) in the UK and Ireland; and Scandiatransplant (Sweden, Norway, Finland, Denmark, and Iceland). Each area identified as a network for organ sharing in Europe adopts an allocation system based on either a center-oriented or a patient-oriented policy. Worldwide, two primary principles dominate the priorization of patients with HCC on the waiting list for deceased-donor liver transplant: urgency and utility. Although no common organ-allocation policy for European countries exists, long-term survival rates for patients with HCC on the transplant waiting lists are comparable to those reported in the United Network for Organ Sharing (UNOS) register. However, as allocation principles are discussed, new proposals emerge, and the epidemiology of liver disease changes, we strongly recommend steps are taken toward a common system.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: ••Of major importance
Ringe B, Pichlmayr R, Tusch G. Surgical treatment of hepatocellular carcinoma: experience with liver resection and transplantation in 198 patients. World J Surg. 1991;15(2):270–85.
Ryder SD. Guidelines for the diagnosis and treatment of hepato- cellular carcinoma (HCC) in adults. Gut. 2003;52 Suppl 3: p. iii1-iii8.
Mazzaferro V et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693–9.
Adam R et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57(3):675–88. doi:10.1016/j.jhep.2012.04.015.
Ioannou GN, Perkins JD, Carithers Jr RL. Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology. 2008;134(5):1342–51.
Toso C, Majno P, Berney T, Morel P, Mentha G, Combescure C. Validation of a dropout assessment model of candidates with/without hepatocellular carcinoma on a common liver transplant waiting list. Transplant Int. 2014;27:686–95.
Merani S, Majno P, Kneteman NM, et al. The impact of waiting list alpha-fetoprotein changes on the outcome of liver transplant for hepatocellular carcinoma. J Hepatol. 2011;55:814–9.
Toso C, Mentha G, Majno P. Liver transplantation for hepatocellular carcinoma: Five steps to prevent recurrence. Am J Transplant. 2011;11:2031–5.
Toso C, Mazzaferro V, Bruix J, et al. Toward a better liver graft allocation that accounts for candidates with and without hepatocellular carcinoma. Am J Transplant. 2014;14(10):2221–7.
Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The survival benefit of liver transplantation. Am J Transplant. 2005;5:307–13.
Schaubel DE, Sima CS, Goodrich NP, Feng S, Merion RM. The survival benefit of deceased donor liver transplantation as a function of candidate disease severity and donor quality. Am J Transplant. 2008;8:419–25.
Cillo U, Vitale A, Volk ML, et al. The survival benefit of liver transplantation in hepatocellular carcinoma patients. Dig Liver Dis. 2010;42:642–9.
Ravaioli M, Grazi GL, Ercolani G, et al. Liver allocation for hepatocellular carcinoma: A European center policy in the pre-MELD era. Transplantation. 2006;81:525–30.
Ravaioli M, Grazi GL, Ballardinin G, et al. Liver transplantation with the Meld system: a prospective study from a single European center. Am J Transplant. 2006;6:1572–7.
Vitale A, Volk ML, De Feo TM, et al. A method for establishing allocation equity among patients with and without hepatocellular carcinoma on a common liver transplant waiting list. J Hepatol. 2014;60:290–7. This article provides the first model in which HCC and non-HCC patients are equally prioritized according to transplant benefit.
Eurotransplant manual. Chap 5. Available at www.eurotransplant.org
Ramos RE, Ortiz de Urbina J, Santoyo Santoyo J, et al. Degree of uniformity in the treatment of hepatocellular carcinoma in the Spanish teams of liver transplantation [Spanish]. Med Clin (Barc). 2013;141(9):406–10.
V Consensus Meeting of the Spanish Society for Liver Transplant on high-risk recipients, immunosupression scenarios and management of hepatocarcinoma on the transplant waiting list. Cir Esp. 2015;93(10):619-37. doi: 10.1016/j.ciresp.2015.04.007
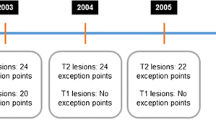
Francoz C et al. Model for end-stage liver disease exceptions in the context of the french model for end-stage liver disease score-based liver allocation system. Liver Transpl. 2011;17:1137–51.
Barber KM, Pioli S, Blackwell JE, et al. Development of a UK score for patients with end-stage liver disease. Hepatology. 2007;46:510A.
Menon KV, Hakeem AR, Heaton ND. Review article: liver transplantation for hepatocellular carcinoma - a critical appraisal of the current worldwide listing criteria. Aliment Pharmacol Ther. 2014;40(8):893–902.
Fosby B et al. Liver transplantation in the nordic countries - an intention to treat and post-transplant analysis from the nordic liver transplant registry 1982-2013. Scand J Gastroenterol. 2015;50(6):797–808. doi:10.3109/00365521.2015.1036359.
Shukla A et al. Liver transplantation: east versus west. J Clin Exp Hepatol. 2013;3(3):243–53. doi:10.1016/j.jceh.2013.08.004.
Cillo U, Burra P, Mazzaferro V, et al. A multistep, consensus-based approach to organ allocation in liver transplantation: toward a “blended principle model”. Am J Transplant. 2015;15:2552–61.
Mazzaferro V. Squaring the circle of selection and allocation in liver transplantation for HCC: an adaptive approach. Hepatology. 2016;63(5):1707–17. This is a new perspective of patients’ priority for liver tranplantation due to HCC. This model is able to contemplate together tumor size and number, tumor response to the locoregional treatments, and feasibility of pre-transplant treatments.
De Giorgio M, Vezzoli S, Cohen E, Armellini E, Lucà MG, Verga G, et al. Prediction of progression-free survival in patients presenting with hepatocellular carcinoma within the Milan criteria. Liver Transpl. 2010;16(4):503–12.
De Carlis L, Di Sandro S, Giacomoni A, Slim A, Lauterio A, Mangoni I, et al. Beyond the Milan criteria: what risks for patients with hepatocellular carcinoma progression before liver transplantation? J Clin Gastroenterol. 2012;46(1):78–86.
Acknowledgments
This work was in part supported by Liver Center Grant P30DK034989 (to MS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Mario Strazzabosco, Stefano Okolicsanyi, Vincenzo Buscemi, Leonardo Centonze, Luciano De Carlis, Riccardo De Carlis, Stefano Di Sandro, Fabio Ferla, Andrea Lauterio, Raffaella Sguinzi, and Luca Saverio Belli have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Liver Transplantation
Rights and permissions
About this article
Cite this article
De Carlis, L., Di Sandro, S., Centonze, L. et al. Liver-allocation policies for patients affected by HCC in Europe. Curr Transpl Rep 3, 313–318 (2016). https://doi.org/10.1007/s40472-016-0117-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0117-6