Abstract
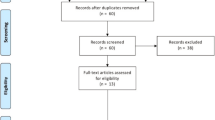
Three-dimensional (3D) printing is a process where a physical object is created from a three-dimensional computer model through successive material layering. 3D printing is used in many industries to design and manufacture new products. Creation of training models for use in medical education is now possible via adoption of medical 3D printing. This article presents a critical-realist review of the medical literature evaluating different ways 3D printing has been used to produce training models for medical education, with a special emphasis on transplantation medicine. From the 68 articles identified by this review, three themes emerged: (a) 3D printing of patient-specific models for preoperative planning, (b) printing training devices for direct use in simulation-based medical education, and (c) printing molds for simulation models that are then used to cast non-printable materials such as soft tissues. Only two reports were identified that described the use of 3D printing for education in transplantation medicine. Many opportunities exist for further research and advancement of 3D printing within the field of transplantation medicine.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004;13 Suppl 1:i2–10.
Boulet JR, Murray D, Kras J, Woodhouse J, McAllister J, Ziv A. Reliability and validity of a simulation-based acute care skills assessment for medical students and residents. Anesthesiology. 2003;99(6):1270–80.
Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–6.
Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci. 2012;7:33.
Barsness KA, Rooney DM, Davis LM. The development and evaluation of a novel thoracoscopic diaphragmatic hernia repair simulator. J Laparoendosc Adv Surg Tech A. 2013;23(8):714–8.
Davis LM, Barsness KA, Rooney DM. Design and development of a novel thoracoscopic tracheoesophageal fistula repair simulator. Stud Health Technol Inform. 2013;184:114–6.
Davis LM, Hawkinson EK, Barsness KA. The evolution of design: a novel thoracoscopic diaphragmatic hernia repair simulator. Stud Health Technol Inform. 2014;196:89–95.
Hawkinson EK, Davis LM, Barsness KA. Design and development of low-cost tissue replicas for simulation of rare neonatal congenital defects. Stud Health Technol Inform. 2014;196:159–62.
Akiba T, Inagaki T, Nakada T. Three-dimensional printing model of anomalous bronchi before surgery. Ann Thorac Cardiovasc Surg. 2014;20(Suppl):659–62.
Bustamante S, Bose S, Bishop P, Klatte R, Norris F. Novel application of rapid prototyping for simulation of bronchoscopic anatomy. J Cardiothorac Vasc Anesth. 2014;28(4):1134–7.
Hochman JB, Kraut J, Kazmerik K, Unger BJ. Generation of a 3D printed temporal bone model with internal fidelity and validation of the mechanical construct. Otolaryngol Head Neck Surg. 2014;150(3):448–54.
Lethaus B, Poort L, Bockmann R, Smeets R, Tolba R, Kessler P. Additive manufacturing for microvascular reconstruction of the mandible in 20 patients. J Craniomaxillofac Surg. 2012;40(1):43–6.
Lu S, Xu YQ, Chen GP, Zhang YZ, Lu D, Chen YB, et al. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg. 2011;16(5):240–8.
Nakada T, Akiba T, Inagaki T, Morikawa T. Thoracoscopic anatomical subsegmentectomy of the right S2b + S3 using a 3D printing model with rapid prototyping. Interact Cardiovasc Thorac Surg. 2014;19(4):696–8.
Zopf DA, Hollister SJ, Nelson ME, Ohye RG, Green GE. Bioresorbable airway splint created with a three-dimensional printer. N Engl J Med. 2013;368(21):2043–5.
Li J, Nie L, Li Z, Lin L, Tang L, Ouyang J. Maximizing modern distribution of complex anatomical spatial information: 3D reconstruction and rapid prototype production of anatomical corrosion casts of human specimens. Anat Sci Educ. 2012;5(6):330–9.
Rose AS, Kimbell JS, Webster CE, Harrysson OL, Formeister EJ, Buchman CA. Multi-material 3D Models for Temporal Bone Surgical Simulation. Ann Otol Rhinol Laryngol. 2015;124(7):528–36.
Waran V, Pancharatnam D, Thambinayagam HC, Raman R, Rathinam AK, Balakrishnan YK, et al. The utilization of cranial models created using rapid prototyping techniques in the development of models for navigation training. J Neurol Surg A Cent Eur Neurosurg. 2014;75(1):12–5.
Schmauss D, Gerber N, Sodian R. Three-dimensional printing of models for surgical planning in patients with primary cardiac tumors. J Thorac Cardiovasc Surg. 2013;145(5):1407–8.
Schmauss D, Schmitz C, Bigdeli AK, Weber S, Gerber N, Beiras-Fernandez A, et al. Three-dimensional printing of models for preoperative planning and simulation of transcatheter valve replacement. Ann Thorac Surg. 2012;93(2):e31–3.
Kang SH, Kim MK, You TK, Lee JY. Modification of planned postoperative occlusion in orthognathic surgery, based on computer-aided design/computer-aided manufacturing-engineered preoperative surgical simulation. J Oral Maxillofac Surg. 2015;73(1):134–51.
Levine JP, Patel A, Saadeh PB, Hirsch DL. Computer-aided design and manufacturing in craniomaxillofacial surgery: the new state of the art. J Craniofac Surg. 2012;23(1):288–93.
Liu YF, Xu LW, Zhu HY, Liu SS. Technical procedures for template-guided surgery for mandibular reconstruction based on digital design and manufacturing. Biomed Eng Online. 2014;13:63.
Hughes A, Soden P, O'Donnchadha B, Tansey A, Abdulkarim A, McMahon C, et al. A ‘Hip’ approach to revision hip surgery-3D printing in complex acetabular reconstruction. Ir J Med Sci. 2014;183(1):S47.
Schwartz A, Money K, Spangehl M, Hattrup S, Claridge RJ, Beauchamp C. Office-based rapid prototyping in orthopedic surgery: a novel planning technique and review of the literature. Am J Orthop (Belle Mead NJ). 2015;44(1):19–25.
Tam MD, Laycock SD, Bell D, Chojnowski A. 3-D printout of a DICOM file to aid surgical planning in a 6 year old patient with a large scapular osteochondroma complicating congenital diaphyseal aclasia. J Radiol Case Rep. 2012;6(1):31–7.
Tan H, Yang K, Wei P, Zhang G, Dimitriou D, Xu L, et al. A novel preoperative planning technique using a combination of CT angiography and three-dimensional printing for complex toe-to-hand reconstruction. J Reconstr Microsurg. 2015;31(5):369–77.
Rondinoni C, E Souza VHO, Matsuda RH, Salles ACP, Santos MV, Filho OB, et al. editors. Inter-institutional protocol describing the use of three-dimensional printing for surgical planning in a patient with childhood epilepsy: From 3D modeling to neuronavigation. 2014 I.E. 16th International Conference on e-Health Networking, Applications and Services, Healthcom 2014; 2015.
Spottiswoode BS, van den Heever DJ, Chang Y, Engelhardt S, Du Plessis S, Nicolls F, et al. Preoperative three-dimensional model creation of magnetic resonance brain images as a tool to assist neurosurgical planning. Stereotact Funct Neurosurg. 2013;91(3):162–9.
Zein NN, Hanouneh IA, Bishop PD, Samaan M, Eghtesad B, Quintini C, et al. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013;19(12):1304–10. 3D printing was used in transplant surgery; employed 3D printing for preoperative planning.
Kusaka M, Sugimoto M, Fukami N, Sasaki H, Takenaka M, Anraku T, et al. Initial experience with a tailor-made simulation and navigation program using a 3-D printer model of kidney transplantation surgery. Transplant Proc. 2015;47(3):596–9. 3D printing was used in transplant surgery; employed 3D printing for preoperative planning.
Waran V, Menon R, Pancharatnam D, Rathinam AK, Balakrishnan YK, Tung TS, et al. The creation and verification of cranial models using three-dimensional rapid prototyping technology in field of transnasal sphenoid endoscopy. Am J Rhinol Allergy. 2012;26(5):e132–6.
Waran V, Narayanan V, Karuppiah R, Owen SL, Aziz T. Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons. J Neurosurg. 2014;120(2):489–92.
Waran V, Narayanan V, Karuppiah R, Thambynayagam HC, Muthusamy KA, Rahman ZAA, et al. Neurosurgical endoscopic training via a realistic 3-dimensional model with pathology. Simul Healthc. 2015;10(1):43–8.
Cheung CL, Looi T, Lendvay TS, Drake JM, Farhat WA. Use of 3-dimensional printing technology and silicone modeling in surgical simulation: development and face validation in pediatric laparoscopic pyeloplasty. J Surg Educ. 2014;71(5):762–7.
Longfield EA, Brickman TM, Jeyakumar A. 3D printed pediatric temporal bone: a novel training model. Otol Neurotol. 2015;36(5):793–5.
Hawkinson EK, Davis LM, Barsness KA, editors. Design and development of a laparoscopic Gastrostomy tube placement simulator. Stud Health Technol Inform. 2014.
Stone J, Candela B, Alleluia V, Fazili A, Richards M, Feng C, et al. A novel technique for simulated surgical procedures using 3D printing technology. J Urol. 2015;193(4):e270.
Turney BW. A new model with an anatomically accurate human renal collecting system for training in fluoroscopy-guided percutaneous nephrolithotomy access. J Endourol. 2014;28(3):360–3.
Stratasys. 3D Printing with Digital Materials. http://www.stratasys.com/materials/polyjet/digital-materials. Accessed 26 Sept 2015.
Hawkinson EK, Davis LM, Barsness KA. Design and development of a laparoscopic gastrostomy tube placement simulator. Stud Health Technol Inform. 2014;196:155–8.
Kurenov SN, Ionita C, Sammons D, Demmy TL. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J Thorac Cardiovasc Surg. 2015;149(4):973–9.e1.
Maddox M, Feibus A, Lee B, Wang J, Thomas R, Silberstein J. Evolution of 3-d physical models of renal malignancies using multi-material 3-d printers. J Urol. 2015;193(4):e242.
Miyazaki T, Yamasaki N, Tsuchiya T, Matsumoto K, Takagi K, Nagayasu T. Airway stent insertion simulated with a three-dimensional printed airway model. Ann Thorac Surg. 2015;99(1):e21–3.
Rose AS, Webster CE, Harrysson OLA, Formeister EJ, Rawal RB, Iseli CE. Pre-operative simulation of pediatric mastoid surgery with 3D-printed temporal bone models. Int J Pediatr Otorhinolaryngol. 2015;79(5):740–4.
Silberstein JL, Maddox MM, Dorsey P, Feibus A, Thomas R, Lee BR. Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: a pilot study. Urology. 2014;84(2):268–72.
Sugimoto M. Bio-elastic patient-specific organ and abdominal cavity replication using multi-material 3d printer for robotic surgical simulation. Surg Endosc Other Interv Techn. 2015;29:S4.
Tam MD, Laycock SD, Brown JR, Jakeways M. 3D printing of an aortic aneurysm to facilitate decision making and device selection for endovascular aneurysm repair in complex neck anatomy. J Endovasc Ther. 2013;20(6):863–7.
Tam MD, Latham T, Brown JR, Jakeways M. Use of a 3D printed hollow aortic model to assist EVAR planning in a case with complex neck anatomy: potential of 3D printing to improve patient outcome. J Endovasc Ther. 2014;21(5):760–2.
Takagi K, Nanashima A, Abo T, Araf J, Matsuo N, Fukuda T, et al. Three-dimensional printing model of liver for operative simulation in perihilar cholangiocarcinoma. Hepato-Gastroenterology. 2014;61(136):2315–6.
Biglino G, Verschueren P, Zegels R, Taylor AM, Schievano S. Rapid prototyping compliant arterial phantoms for in-vitro studies and device testing. J Cardiovasc Magn Reson. 2013;15:2.
Chandrasekhara V. Thinking inside the box: 3-dimensional printing for interventional EUS training. Gastrointest Endosc. 2015;81(2):447–9.
Costello JP, Olivieri LJ, Krieger A, Thabit O, Marshall MB, Yoo SJ, et al. Utilizing three-dimensional printing technology to assess the feasibility of high-fidelity synthetic ventricular septal defect models for simulation in medical education. World J Pediatr Congenit Hearth Surg. 2014;5(3):421–6.
Costello JP, Olivieri LJ, Su L, Krieger A, Alfares F, Thabit O, et al. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit Heart Dis. 2015;10(2):185–90.
Dhir V, Itoi T, Fockens P, Perez-Miranda M, Khashab MA, Seo DW, et al. Novel ex vivo model for hands-on teaching of and training in EUS-guided biliary drainage: creation of “mumbai EUS” stereolithography/3D printing bile duct prototype (with videos). Gastrointest Endosc. 2015;81(2):440–6.
Dimeo AJ, Lalush DS, Grant E, Morcuende JA. Development of a surrogate biomodel for the investigation of clubfoot bracing. J Pediatr Orthop. 2012;32(7):e47–52.
Dziegielewski PT, Zhu J, King B, Grosvenor A, Dobrovolsky W, Singh P, et al. Three-dimensional biomodeling in complex mandibular reconstruction and surgical simulation: prospective trial. J Otolaryngol Head Neck Surg. 2011;40 Suppl 1:S70–81.
Fasel JH, Beinemann J, Schaller K, Gailloud P. A critical inventory of preoperative skull replicas. Ann R Coll Surg Engl. 2013;95(6):401–4.
Fu M, Lin L, Kong X, Zhao W, Tang L, Li J, et al. Construction and accuracy assessment of patient-specific biocompatible drill template for cervical anterior transpedicular screw (ATPS) insertion: an in vitro study. PLoS One. 2013;8(1):e53580.
Holt BA, Hearn G, Hawes R, Tharian B, Varadarajulu S. Development and evaluation of a 3D printed endoscopic ampullectomy training model. Gastrointest Endosc. 2015;81(5):AB330–1.
McMenamin PG, Quayle MR, McHenry CR, Adams JW. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ. 2014.
Nishimoto S, Sotsuka Y, Kawai K, Fujita K, Kakibuchi M. Three-dimensional mock-up model for chondral framework in auricular reconstruction, built with a personal three-dimensional printer. Plast Reconstr Surg. 2014;134(1):180e–1.
Olivieri LJ, Krieger A, Loke YH, Nath DS, Kim PCW, Sable CA. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Soc Echocardiogr. 2015;28(4):392–7.
Sakuragi T. Stereolithographic biomodelling of pulmonary hilum by multislice computed tomography imaging. Eur J Cardiothorac Surg. 2014;46(1):143.
Salmi M, Paloheimo KS, Tuomi J, Wolff J, Makitie A. Accuracy of medical models made by additive manufacturing (rapid manufacturing). J Craniomaxillofac Surg. 2013;41(7):603–9.
Starosolski ZA, Kan JH, Rosenfeld SD, Krishnamurthy R, Annapragada A. Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol. 2014;44(2):216–21.
Watson RA. A low-cost surgical application of additive fabrication. J Surg Educ. 2014;71(1):14–7.
Werner H, Rolo LC, Araujo Junior E, Dos Santos JR. Manufacturing models of fetal malformations built from 3-dimensional ultrasound, magnetic resonance imaging, and computed tomography scan data. Ultrasound Q. 2014;30(1):69–75.
West SJ, Mari JM, Khan A, Wan JH, Zhu W, Koutsakos IG, et al. Development of an ultrasound phantom for spinal injections with 3-dimensional printing. Reg Anesth Pain Med. 2014;39(5):429–33.
Hakansson A, Rantatalo M, Hansen T, Wanhainen A. Patient specific biomodel of the whole aorta - the importance of calcified plaque removal. Vasa. 2011;40(6):453–9.
Mashiko T, Yang Q, Kaneko N, Konno T, Yamaguchi T, Watanabe E. Pre-surgical simulation of microvascular decompression for hemifacial spasm using 3D-models. Neurol Surg. 2015;43(1):41–9.
Mashiko T, Otani K, Kawano R, Konno T, Kaneko N, Ito Y, et al. Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 2015;83(3):351–61.
O'Reilly MK, Reese S, Herlihy T, Geoghegan T, Cantwell CP, Feeney RN, et al. Fabrication and assessment of 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training in medicine. Anat Sci Educ. 2015.
Wurm G, Lehner M, Tomancok B, Kleiser R, Nussbaumer K. Cerebrovascular biomodeling for aneurysm surgery: simulation-based training by means of rapid prototyping technologies. Surg Innov. 2011;18(3):294–306.
Acknowledgments
The authors would like to thank Senior Clinical Informationist, Jonna Peterson, at Northwestern University’s Galter Health Sciences Library for her help conducting the search.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ellen O’Brien, Diane B. Wayne, Katherine A. Barsness, William C. McGaghie, and Jeffrey H. Barsuk declare that they have no conflict of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Tissue Engineering and Regeneration
Appendix
Appendix
Sixty-eight articles describing 3D printing used for medical education. Authors that only suggested future use of their models in preoperative planning were categorized as “simulation model.” If the authors used a mold, despite using the model for either simulation, or preoperative planning, the article was categorized as “mold making.”
Reference | Article Summary | Specialty | Use of 3D Printing |
Akiba et al. [9] | Created 3D printed bronchi and associated pulmonary vessels from a CT scan to help planning in a patient with anomalous bronchial anatomy prior to thoracosopic surgery to remove a lung tumor. | Thoracic Surgery | Pre-Op |
Hughes et al. [24] | Printed models of two patients’ acetabular anatomy to assist surgical decision-making before revision hip arthroplasty. Screw trajectory simulation was also carried out on the models. | Orthopedic Surgery | Pre-Op |
Kang et al. [21] | 3D printed craniofacial anatomy of a patient to plan a corrective surgery for a prognathic mandible with right deviation. | Maxillofacial Surgery | Pre-Op |
Kurenov et al. [42] | Printed pulmonary artery trees from 10 normal patients to facilitate anatomic study and surgical planning of lobectomy. Researchers used the models to design a catheter to give regional chemotherapy. | Thoracic Surgery | Pre-Op |
Kusaka et al. [31•] | Developed a kidney graft and pelvic cavity replica as a patient-specific 3D model for living kidney transplantation. | Transplantation Medicine | Pre-Op |
Lethaus et al. [12] | 3D printed models of 20 patients’ mandibles to adapt reconstruction plates prior to mandibular resection and reconstruction surgery. | Maxillofacial Surgery | Pre-Op |
Levine et al. [22] | Used 3D printed models in presurgical planning of four different patients including mandibular tumor resection and fibular flap reconstruction, repair of skeletofacial abnormalities, maxillofacial trauma, and posttraumatic TMJ ankylosis. | Maxillofacial Surgery | Pre-Op |
Liu et al. [23] | Printed 3D model of a patient’s mandible and fibular bone which was used as a reference to plan a fibular grafting during a mandibular reconstruction following tumor resection. Although the article focused on one patient’s surgical results, 15 patients with mandibular reconstructions using the methodology. | Maxillofacial Surgery | Pre-Op |
Maddox et al. [43] | Created 3D models of 12 patient’s kidneys with suspicious masses for trainees to visualize and understand surgical resection. | Urology | Pre-Op |
Miyazaki et al. [44] | Created 3D printed bronchial model for airway stenting insertion practice before performing the procedure on the patient with a single lung transplant complicated by stenosis of the intermediate bronchus. | Thoracic Surgery | Pre-Op |
Nakada et al. [14] | Used a 3D printed model of the bronchovascular anatomy from CT scans of patient with lung cancer before thoracoscopic resection. | Thoracoscopic Surgery | Pre-Op |
Rondinoni et al. [28] | Produced a model that represented the brain and face segment of a child with Sturge-Weber syndrome for presurgical planning. | Neurological Surgery | Pre-Op |
Rose et al. [45] | Created a 3D model of a child’s temporal bone to perform pre-operative simulation and planning of a tympano-mastoidectomy for a recurrent cholesteatoma. | Otolaryngology | Pre-Op |
Schmauss et al. [19] | 3D printed models for surgical planning of a patient with a right ventricular cardiac fibroma to decide the best surgical approach (partial resection, total resection, or heart transplant). | Cardiac surgery | Pre-Op |
Schmauss et al. [20] | Printed a model of a patient with severe aortic stenosis and a porcelain aorta who died after transcatheter aortic valve replacement for evaluation of previous surgical panning. | Cardiac Surgery | Pre-Op |
Schwartz et al. [25] | Created rapid prototypes in seven cases of orthopedic surgery for preoperative plan for hip, knee and shoulder arthroplasties, corrective osteotomy and osteochondroma resection. | Orthopedic Surgery | Pre-Op |
Silberstein et al. [46] | Created 3D models of five patient’s kidneys with enhancing renal lesions for trainees to visualize before surgical resection. | Urology | Pre-Op |
Spottiswood et al. [29] | Created patient-specific 3D scale models of two patients’ brains to indicate the location and extent of a tumor relative to brain surface features and important adjacent structures using functional MRI. | Neurological surgery | Pre-Op |
Sugimoto et al. [47] | Created bio-elastic organ and abdominal cavity replication for robotic surgical simulation in 10 patients. | General Surgery | Pre-Op |
Tam et al. [26] | 3D printed a large scapular osteochondroma in a patient with congenital diaphyseal aclasia to plan the surgical approach. | Orthopedic Surgery | Pre-Op |
Tam et al. [48] | 3D Printed hollow aortic aneurysm model to determine if complex anatomy was amenable to stenting in a specific patient. | Vascular Surgery | Pre-Op |
Tam et al. [49] | 3D printed a hollow aortic aneurysm model from a patient with complex anatomy. Simulated the endovascular aneurysm repair before performing the procedure in the patient. | Vascular Surgery | Pre-Op |
Tan et al. [27] | Created 3D soft tissue and skeletal models for injured and uninjured hands for preoperative planning in complicated toe-to-hand reconstruction. | Orthopedic Surgery | Pre-Op |
Takagi et al. [50] | Printed patient specific liver with intrahepatic cholangiocarcinoma. Compared resected specimen on actual patient to 3D model confirming proper cutting location post hoc. | Surgical Oncology | Pre-Op |
Zopf et al. [15] | 3D printed the bronchial anatomy of an infant with tracheobronchomalacia created a bioresorbable tracheal splint for insertion into the bronchial tree. | Otolaryngology | Pre-Op |
Zein et al. [30•] | Printed models of three sets recipients and donor livers prior to transplant surgery. | Transplantation Medicine | Pre-Op |
Barsness et al. [5] | Created 3D printed rib cages for diaphragmatic hernia repair model and trained pediatrics surgeon at a national meeting. | Pediatric Surgery | Simulation Models |
Biglino et al. [51] | Printed compliant arterial phantoms for in-vitro studies and device testing of a hypoplastic aorta and a right ventricular outflow tract. | Cardiovascular Imaging | Simulation Models |
Bustamante et al. [10] | 3D printed two tracheobronchial tree models and connected them to a mannequin for simulation of bronchoscopic anatomy. | Anesthesiology | Simulation Models |
Chandrasekhara et al. [52] | 3D printed bile duct prototype for teaching and training endoscopic ultrasound guided biliary drainage. | Gastroenterology | Simulation Models |
Cheung et al. [35] | Developed 3D printed model of the kidney, renal pelvis, and ureter cast with silicone for pediatric laparoscopic pyeloplasty. | Urology | Simulation Models |
Costello et al. [53] | Created five 3D printed cardiac models of common ventricular septal defect based on archived MRIs for teaching medical students. | Cardiology | Simulation Models |
Costello et al. [54] | Incorporated five 3D printed cardiac models of ventricular septal defects into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. | Cardiology | Simulation Models |
Davis et al. [6] | Created 3D printed thoracoscopic tracheoesophageal fistula repair simulator (model included skin, ribs, and fistula). | Pediatric Surgery | Simulation Models |
Davis et al. [7] | Designed a novel thoracoscopic diaphragmatic hernia repair simulator with 3D printing (model included skin, ribs, diaphragm, hernia). | Pediatric Surgery | Simulation Models |
Dhir et al. [55] | Created and evaluated a model for training endoscopic ultrasound-guided biliary drainage. | Gastroenterology | Simulation Models |
Dimeo et al. [56] | Developed of a surrogate biomodel for the investigation of clubfoot bracing with 3D printing pediatric bones. | Orthopedic Surgery | Simulation Models |
Dziegielewski et al. [57] | Created 3D model for complex mandibular reconstruction and surgical simulation training for residents. | Maxillofacial Surgery | Simulation Models |
Fasel et al. [58] | Created 3D skull models from cadavers to look at feasibility as a training substitute. | Anatomic Pathology | Simulation Models |
Fu et al. [59] | Created anatomy-specific biocompatible drill templates from cadaveric CT scans in preparation for cervical anterior transpedicular screw insertion. The template was tested on the same cadaveric cervical vertebrate from which it was created with success. | Orthopedic Surgery | Simulation Models |
Hochman et al. [11] | 3D printed a replication of human temporal bone from CT scans for training purposes. Tested 4 different model types for realism during dissection by resident and staff physicians. | Otolaryngology | Simulation Models |
Holt et al. [60] | Developed and evaluated of a 3D printed endoscopic ampullectomy training model (stomach, duodenum, ampulla). | Gastroenterology | Simulation Models |
Li et al. [16] | Used anatomic corrosion casts of cadavers to create 3D lung models with the bronchial tree, and arteries, and veins. | Anatomic Pathology | Simulation Models |
Longfield et al. [36] | 3D printed pediatric temporal bone training model for temporal bone surgery including mastoidectomy, facial recess procedures and cochleostomy. | Otolaryngology | Simulation Models |
Lu et al. [13] | Created 3D printed cervical pedicle screw templates for training of screw placement on cadaver spines. | Orthopedic Surgery | Simulation Models |
McMenamin et al. [61] | Used 3D printing to produce anatomical teaching resources. | Anatomic Pathology | Simulation Models |
Nishimoto et al. [62] | Printed 3D mock-up model for chondral framework in auricular reconstruction that can be sterilized and used for planning in the operating room. | Plastic Surgery | Simulation Models |
Olivieri et al. [63] | Printed models of eight ventricular septal defects and three peri prosthetic aortic valve leaks using 3D echocardiographic images. | Cardiology | Simulation Models |
Rose et al. [17] | 3D printed models of temporal bone were created and dissected by otolaryngologists who rated the model for anatomic suitability and realism of operative bone drilling. | Otolaryngology | Simulation Models |
Sakuragi et al. [64] | 3D printed a biomodel of pulmonary hilum by CT imaging. | Cardiothoracic Surgery | Simulation Models |
Salmi et al. [65] | 3D printed skull models to determine accuracy of printers. | Maxillofacial Surgery | Simulation Models |
Starosolski et al. [66] | Applied 3D printing technology to print the bony anatomy of pediatric musculoskeletal disorders. | Orthopedic Surgery | Simulation Models |
Waran et al. [32] | Created cranial models using 3D printing of the nasal cavity, paranasal sinuses, and intrasellar pathology for endoscopic transsphenoidal surgery training. | Neurological Surgery | Simulation Models |
Waran et al. [33] | Used 3D printer to create models of the head to enhance the training experience of neurosurgeons when performing craniotomies for tumor resections. | Neurological Surgery | Simulation Models |
Waran et al. [34] | Created 3D printed head model with hydrocephalus that was used for neurosurgical endoscopic third ventriculostomy and intraventricular biopsy training. | Neurological Surgery | Simulation Models |
Waran et al. [18] | Used patient CT data from three actual patients (one with each of hydrocephalus, a right frontal cortical lesion, and midline clival meningioma) to create 3D printed models used for navigational brain surgery simulations. | Neurological Surgery | Simulation Models |
Watson et al. [67] | 3D printed multiple patient-specific portal and hepatic venous anatomies for surgical resident education. | General Surgery | Simulation Models |
Werner et al. [68] | Manufactured models of fetal malformations built from 3D ultrasound, MRI, and CT scan data. | Pediatrics | Simulation Models |
West et al. [69] | Developed a 3D printed model of a spine that could be used for ultrasound imaging and spinal injections. | Anesthesiology | Simulation Models |
Hakansson et al. [70] | Created patient specific aorta from a mold after digital removing calcified plaque. The model was used for practicing endovascular stenting of a thoracoabdominal aneurysm. | Vascular Surgery | Mold Making |
Hawkinson et al. [41] | 3D printed a laparoscopic gastrostomy tube placement simulator (skin, ribs, stomach). | Pediatric Surgery | Mold Making |
Hawkinson et al. [8] | 3D printed molds of tissue replicas for simulation of rare neonatal congenital defects including esophageal atresia, duodenal atresia and tracheoesophageal fistulas. | Pediatric Surgery | Mold Making |
Mashiko et al. [71] | Created 3D models of skulls, cerebellum, and blood vessels for simulating microvascular decompression for hemifacial spasms in seven patients. | Neurological Surgery | Mold Making |
Mashiko et al. [72] | Developed 3D printed hollow elastic model for cerebral aneurysm clipping simulation before surgery on 12 patients. | Neurological Surgery | Mold Making |
O’Reilly et al. [73] | Fabricated 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training. | Interventional Radiology | Mold Making |
Stone et al. [38] | Created 3D printed molds of a left kidney, renal artery/vein, pelvicalyceal system, great vessels, and tumors to train surgeons on operative techniques. | Urology | Mold Making |
Turney et al. [39] | Built an anatomically accurate human renal collecting system by 3D printing CT urograms. The models were created for training in fluoroscopy-guided percutaneous nephrolithotomy access. | Urology | Mold Making |
Wurm et al. [74] | Created cerebrovascular biomodel for aneurysm surgery clipping training. | Neurological Surgery | Mold Making |
Rights and permissions
About this article
Cite this article
O’Brien, E.K., Wayne, D.B., Barsness, K.A. et al. Use of 3D Printing for Medical Education Models in Transplantation Medicine: a Critical Review. Curr Transpl Rep 3, 109–119 (2016). https://doi.org/10.1007/s40472-016-0088-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0088-7