Abstract
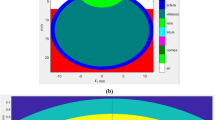
Corneal reshaping using laser ablation effect is a well-known ophthalmologic operation implemented to correct many vision disorders. UV pulsed lasers are utilized in this surgery due to their high absorption in corneal tissue without affecting the other parts of the eye. Ideally ablation may not be associated with heat transport, since high temperature is the enemy of soft tissues. However, the thermal effect of this procedure can cause tissue damage if the temperature rises above the safety level without appropriate handling. In the present study, we try to find the trade-off between efficient ablation and minimal temperature rise. So the thermal effect on the corneal tissue after applying five UV wavelengths; 193, 210, 213, 223 and 248 nm has been simulated and investigated by solving Penne’s bio-heat transfer equation using the finite element method. A 3D model of the human cornea is constructed using COMSOL Multiphysics computer software and the temperature rise is determined at the end of the laser pulse. The same spot size and pulse duration are used for each wavelength. While the absorption coefficient of the corneal tissue is the only variable as it is a wavelength dependent. The proposed results show that, the heating effect is directly proportional to the absorption coefficient. The highest recorded temperature was 259 °C at 193 nm, while, the minimum value was (70.1 °C) recorded at 248 nm at which the cornea has the lowest absorption coefficient.





Similar content being viewed by others
References
Yun SH, Kwok SJJ (2017) Light in diagnosis, therapy and surgery. Nat Biomed Eng 1(0008):1–39
Hamdy O, Alsharafi SS, Hassan MF, Eldib A, Solouma NH (2019) A multi-spot laser system for retinal disorders treatment: experimental study. Opt Int J Light Electron Opt 185:609–613
Daukantas P (2010) Lasers in ophthalmology. OPN Opt Photonics News. https://doi.org/10.1364/OPN.21.2.000028
Pidro A, Biscevic A, Pjano MA, Mravicic I, Bejdic N, Bohac M (2019) Excimer lasers in refractive surgery. Acta Inform Med 27(4):278–283
Nagaraja H, Mehta JS, Zhou X, Yam JC, Lam DSC (2019) Will SMILE become the new benchmark of corneal laser refractive surgery? Asia-Pac J Ophthalmol 8(5):351–354
Han SB, Liu YC, Mohamed-Noriega K, Mehta JS (2020) Application of femtosecond laser in anterior segment surgery. J Ophthalmol. https://doi.org/10.1155/2020/8263408
Azar DT, Koch DD (2003) LASIK: fundamentals, surgical techniques, and complications. Marcel Dekker, New York
Krader CG (2019) Laser refractive surgery advances expand options for myopic patients. Ophthalmol Times 44(5):1–9
Kane SN, Mishra A, Dutta AK (2017) Pulsed UV laser technologies for ophthalmic surgery. J Phys Conf Ser 793:1–12
Markolf NH (2007) Laser-tissue interactions: fundamentals and applications. Springer, Heidelberg
Sharma N, Vajpayee RB, Sullivan L (2005) Step by step LASIK surgery. CRC Press, New York
Shah S, Piovella M (2013) Solid-state laser platforms: two reviews the benefits of using the Pulzar Z1 and LaserSoft technologies. Cataract & Refractive Surgery Today EUROPE
Arranz-Marquez E, Katsanos A, Kozobolis VP, Konstas AGP, Teus MA (2019) A critical overview of the biological effects of mitomycin C application on the cornea following refractive surgery. Adv Ther 36(4):786–797
Liu W, Lu Y, She R, Wei G, Jiao G (2019) Thermal analysis of cornea heated with terahertz radiation. Appl Sci 9(917):1–9
Min JS, Min BM (2020) Comparison between surgical outcomes of LASIK with and without laser asymmetric keratectomy to avoid conventional laser refractive surgery adverse effects. Sci Rep 10(1):1–8
Hosszufalusi N, Mikula ER, Sun H, Hosszufalusi N, Mikula ER, Juhasz T (2011) Simulation of the temperature increase in human cadaver retina during direct illumination by 150-kHz femtosecond simulation of the temperature increase in human cadaver retina during direct illumination by 150-kHz femtosecond laser pulses. J Biomed Opt 16(10):108001
Kc G, Gurung DB, Adhikary PR (2015) mathematical model: comparative study of thermal effects of laser in corneal refractive surgeries. Appl Appl Math 10(1):620–633
Szekrenyesi C, Sandor G, Gyenes A, Kiss H, Filkorn T, Nagy ZZ (2016) The change of corneal surface temperature during surface refractive surgical procedures performed using excimer lasers with different repetitive frequencies. New Med 20:81–85
Mirnezami SA, Jafarabadi MR, Abrishami M (2013) Temperature distribution simulation of the human eye exposed to laser radiation. Laser Med Sci 4(4):175–181
Rahbar S, Shokooh-saremi M (2018) Mathematical modeling of laser linear thermal effects on the anterior layer of the human eye. Opt Laser Technol 99:72–80
Joukar A, Nammakie E, Niroomand-oscuii H (2015) A comparative study of thermal effects of 3 types of laser in eye: 3D simulation with bioheat equation. J Therm Biol 49–50:74–81
Cvetkovi M, Poljak D, Peratta A (2008) Thermal modelling of the human eye exposed to laser radiation. 16th international conference on software, telecommunications and computer network. IEEE, New York, pp 16–20
Hamdy O, Mohammed HS (2020) Investigating the transmission profiles of 808 nm laser through different regions of the rat’ s head. Lasers Med Sci. https://doi.org/10.1007/s10103-020-03098-9
Shih KC, Tse RHK, Lau YTY, Chan TCY (2019) Advances in corneal imaging: current applications and beyond. Asia-Pac J Ophthalmol 8(2):105–114
Ng E, Tan JH, Acharya UR, Suri JS (2018) Human eye imaging and modeling. CRC Press, New York
Ivarsen A, Fledelius W, Hjortdal JØ (2009) Three-year changes in epithelial and stromal thickness after PRK or LASIK for high myopia. IOVS 50(5):2061–2066
Trembly BS (2017) Thermal techniques for reshaping the cornea. Proc SPIE 1029704:1–29
Lembares A, Hu X, Kalmwf GW (1997) Absorption spectra of corneas in the far ultraviolet region. Invest Ophthalmol Vis Sci 38(6):1283–1287
Zhmakin AI (2017) Heat transfer in vivo: phenomena & models. Handbook of thermal science and engineering. Springer, Cham, pp 1–47
Ren Q, Simon G, Parel JM (1993) Ultraviolet solid-state laser (213-nm) photorefractive keratectomy. In vitro study. Ophthalmology 100(12):1828–1834. https://doi.org/10.1016/s0161-6420(93)31390-4
Lin JT (2001) Refractive surgical laser apparatus and method, U.S. patent US2001/0037105A1
Rabczuk G, Sawczak M (2006) Study on the possibilities of controlling the laser output beam properties by an intracavity deformable mirror. Opto-Electron Rev 14(2):141–147
MEL 90 from ZEISS Advancing excimer laser technology. https://www.zeiss.com/content/dam/med/ref_international/products/refractivelasers/excimerlasesolution/mel90/pdf/mel-90-broschuere-en-34-010-0004v.pdf. Accessed 29 Dec 2020
The PULZAR Z1 solid state refractive laser. http://www.customvis.com/products/laser.php. Accessed 29 Dec 2020
LaserSoft—UV ablation laser. http://katanalaser.com/products/lasersoft/. Accessed 29 Dec 2020
McDonald MB (2005) Conductive keratoplasty: a radiofrequency-based technique for the correction of hyperopia. Trans Am Ophthalmol Soc 103:512–536
Taylor P, Brunsmann U, Sauer U, Dressler K, Triefenbach N, Arba S (2010) Minimisation of the thermal load of the ablation in high-speed laser corneal refractive surgery: the intelligent thermal effect control of the AMARIS platform. J Mod Opt 57(6):466–479
Hamdy O, El-Azab J, Al-Saeed TA, Hassan MF, Solouma NH (2017) A method for medical diagnosis based on optical fluence rate distribution at tissue surface. Materials 10(9):1–13
Hamdy O, Fathy M, Al-Saeed TA, El-Azab J, Solouma NH (2017) Estimation of optical parameters and fluence rate distribution in biological tissues via a single integrating sphere optical setup. Optik 140:1004–1009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no conflict of interest.
Ethical approval
Not required as the study is a simulation study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abdelhalim, I., Hamdy, O., Hassan, A.A. et al. Dependence of the heating effect on tissue absorption coefficient during corneal reshaping using different UV lasers: A numerical study. Phys Eng Sci Med 44, 221–227 (2021). https://doi.org/10.1007/s13246-021-00971-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-021-00971-x