Abstract
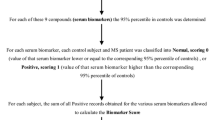
An imbalance of inflammatory/anti-inflammatory and oxidant/antioxidant molecules has been implicated in the demyelination and axonal damage in multiple sclerosis (MS). The current study aimed to evaluate the plasma levels of tumor necrosis factor (TNF)-α, soluble TNF receptor (sTNFR)1, sTNFR2, adiponectin, hydroperoxides, advanced oxidation protein products (AOPP), nitric oxide metabolites, total plasma antioxidant capacity using the total radical-trapping antioxidant parameter (TRAP), sulfhydryl (SH) groups, as well as serum levels of zinc in 174 MS patients and 182 controls. The results show that MS is characterized by lowered levels of zinc, adiponectin, TRAP, and SH groups and increased levels of AOPP. MS was best predicted by a combination of lowered levels of zinc, adiponectin, TRAP, and SH groups yielding an area under the receiver operating characteristic (AUC/ROC) curve of 0.986 (±0.005). The combination of these four antioxidants with sTNFR2 showed an AUC/ROC of 0.997 and TRAP, adiponectin, and zinc are the most important biomarkers for MS diagnosis followed at a distance by sTNFR2. Support vector machine with tenfold validation performed on the four antioxidants showed a training accuracy of 92.9% and a validation accuracy of 90.6%. The results indicate that lowered levels of those four antioxidants are associated with MS and that these antioxidants are more important biomarkers of MS than TNF-α signaling and nitro-oxidative biomarkers. Adiponectin, TRAP, SH groups, zinc, and sTNFR2 play a role in the pathophysiology of MS, and a combination of these biomarkers is useful for predicting MS with high sensitivity, specificity, and accuracy. Drugs that increase the antioxidant capacity may offer novel therapeutic opportunities for MS.



Similar content being viewed by others
References
Thompson AJ, Baranzini SE, Geurts J, Hemmer B, Ciccarelli O (2018) Multiple sclerosis. Lancet. 391(10130):1622–1636. https://doi.org/10.1016/S0140-6736(18)30481-1
Aslani S, Jafari N, Javan MR, Karami J, Ahmadi M, Jafarnejad M (2017) Epigenetic modifications and therapy in multiple sclerosis. Neuromolecular Med 19(1):11–23. https://doi.org/10.1007/s12017-016-8422-x
Witkowska AM, Socha K, Kochanowicz J, Karpińska E, Jakoniuk M, Zujko ME, Wilkiel M, Borawska MH et al (2016) Serum levels of biomarkers of immune activation and associations with neurological impairment in relapsing-remitting multiple sclerosis patients during remission. Biol Res Nurs 18(1):113–119. https://doi.org/10.1177/1099800415583105
Islam MT (2017) Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol Res 39(1):73–82. https://doi.org/10.1080/01616412.2016.1251711
Trenova AG, Slavov GS, Manova MG, Draganaova-Filipova MN, Mateva NG, Miteva LD, Miteva LD, Stanilova SA (2017) Alterations in serum levels of IL-17 in contrast to TNF-alpha correspond to disease-modifying treatment in relapsing-remitting multiple sclerosis. Scand J Clin Lab Invest 77(4):283–288. https://doi.org/10.1080/00365513.2017.1303843
Pegoretti V, Baron W, Laman JD, Eisel ULM (2018) Selective modulation of TNF–TNFRs signaling: insights for multiple sclerosis treatment. Front Immunol 9:925. https://doi.org/10.3389/fimmu.2018.00925
Faustman D, Davis M (2010) TNF receptor 2 pathway: drug target for autoimmune diseases. Nat Rev Drug Discov 9(6):482–493. https://doi.org/10.1038/nrd3030
Kallaur AP, Oliveira SR, Simão ANC, Alfieri DF, Flauzino T, Lopes J, de Carvalho Jennings Pereira W, de Meleck PC et al (2017) Cytokine profile in patients with progressive multiple sclerosis and its association with disease progression and disability. Mol Neurobiol 54(4):2950–2960. https://doi.org/10.1007/s12035-016-9846-x
Oliveira SR, Flauzino T, Sabino BS, Kallaur AP, Alfieri DF, Kaimen-Maciel DR, Morimoto HK, de Almeida ERD et al (2018) Elevated plasma homocysteine levels are associated with disability progression in patients with multiple sclerosis. Metab Brain Dis 33(5):1393–1399. https://doi.org/10.1007/s11011-018-0224-4
Ouchi N, Kihara S, Arita Y, Maeda K, Kuriyama H, Okamoto Y, Hotta K, Nishida M et al (1999) Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 100(25):2473–2476. https://doi.org/10.1161/01.cir.100.25.2473
Ribeiro CM, Oliveira SR, Alfieri DF, Flauzino T, Kaimen-Maciel DR, Simão ANC, Maes M, Reiche EMV (2019) Tumor necrosis factor alpha (TNF-α) and its soluble receptors are associated with disability, disability progression and clinical forms of multiple sclerosis. Inflamm Res 68(12):1049–1059. https://doi.org/10.1007/s00011-019-01286-0
Yokota T, Oritani K, Takahashi I, Ishikawa J, Matsuyama A, Ouchi N, Kihara S, Funahashi T et al (2000) Adiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophages. Blood 96(5):1723–1732
Wolf AM, Wolf D, Rumpold H, Enrich B, Tilg H (2004) Adiponectin induces the anti-inflammatory cytokines IL-10 and IL-1RA in human leukocytes. Biochem Biophys Res Commun 323(2):630–635. https://doi.org/10.1016/j.bbrc.2004.08.145
Motoshima H, Wu X, Mahadev K, Goldstein BJ (2004) Adiponectin suppresses proliferation and superoxide generation and enhances eNOS activity in endothelial cells treated with oxidized LDL. Biochem Biophys Res Commun 315(2):264–271. https://doi.org/10.1016/j.bbrc.2004.01.049
Wang X, Pu H, Ma C, Jiang T, Wei Q, Zhang C, Duan M, Shou X et al (2014) Adiponectin abates atherosclerosis by reducing oxidative stress. Med Sci Monit 20:1792–1800. https://doi.org/10.12659/MSM.892299
Musabak U, Demirkaya S, Genç G, Ilikci RS, Odabasi Z (2011) Serum adiponectin, TNF-α, IL-12p70, and IL-13 levels in multiple sclerosis and the effects of different therapy regimens. Neuroimmunomodulation 18(1):57–66. https://doi.org/10.1159/000317393
Guerrero-García JJ, Carrera-Quintanar L, López-Roa RI, Márquez-Aguirre AL, Rojas-Mayorquín AE, Ortuño-Sahagún D (2016) Multiple sclerosis and obesity: possible roles of adipokines. Mediat Inflamm 2016:4036232. https://doi.org/10.1155/2016/4036232
Natarajan R (2016) Biomarkers in Multiple Sclerosis Special emphasis on Melatonin and Adipokines. Acta Universitatis Tamperensis 2172 Tampere University Press Tampere 98p.
Bloemer J, Pinky PD, Govindarajulu M, Hong H, Judd R, Amin RH, Moore T, Dhanasekaran M et al (2018) Role of Adiponectin in Central Nervous System Disorders. Neural Plast 2018:4593530. https://doi.org/10.1155/2018/4593530
Ljubisavljevic S, Stojanovic I, Cvetkovic T, Vojinovic S, Stojanov D, Stojanovic D, Stefanovic N, Pavlovic D (2014) Erythrocytes' antioxidative capacity as a potential marker of oxidative stress intensity in neuroinflammation. J Neurol Sci 337(1–2):8–13. https://doi.org/10.1016/j.jns.2013.11.006
Adamczyk B, Adamczyk-Sowa M (2016, 2016) New insights into the role of oxidative stress mechanisms in the pathophysiology and treatment of multiple sclerosis. Oxid Med Cell Longev. https://doi.org/10.1155/2016/1973834
Oliveira SR, Kallaur AP, Simão AN, Morimoto HK, Lopes J, Panis C, Petenucci DL, da Silva E et al (2012) Oxidative stress in multiple sclerosis patients in clinical remission: association with the expanded disability status scale. J Neurol Sci 321(1–2):49–53. https://doi.org/10.1016/j.jns.2012.07.045
Ferreira KPZ, Oliveira SR, Kallaur AP, Kaimen-Maciel DR, Lozovoy MAB, de Almeida ERD, Morimoto HK, Mezzaroba L et al (2017) Disease progression and oxidative stress are associated with higher serum ferritin levels in patients with multiple sclerosis. J Neurol Sci 373:236–241. https://doi.org/10.1016/j.jns.2016.12.039
Lee SR (2018) Critical role of zinc as either an antioxidant or a prooxidant in cellular systems. Oxidative Med Cell Longev 2018:9156285. https://doi.org/10.1155/2018/9156285
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E et al (2011) Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann Neurol 69(2):292–302. https://doi.org/10.1002/ana.22366
Brazil. Brazilian Institute of Geography and Statistics (2011) Characteristics of the population and households: results of the universe. Available in: https://ww2.ibge.gov.br/english/estatistica/populacao/censo2010/caracteristicas_da_populacao/default_caracteristicas_da_populacao.shtm. Accessed 3 Jul 2018.
Gonzales Flecha B, Llesuv S, Boveris A (1991) Hydroperoxide-initiated chemiluminescence: an assay for oxidative stress in biopsies of heart, liver, and muscle. Free Radic Biol Med 10(2):93–100. https://doi.org/10.1016/0891-5849(91)90002-k
Witko-Sarsat V, Friedlander M, Nguyen Khoa T, Capeillère-Blandin C, Nguyen AT, Canteloup S, Dayer JM, Jungers P et al (1996) Advanced oxidation protein products as novel mediators of inflammation and monocyte activation in chronic renal failure. J Immunol 161(5):2524–2532
Navarro-Gonzálvez JA, García-Benayas C, Arenas J (1998) Semiautomated measurement of nitrate in biological fluids. Clin Chem 44(3):679–681. https://doi.org/10.1515/CCLM.2008.096
Hu ML (1994) Measurement of protein thiol groups and glutathione in plasma. In: Abelson JN, Simon MI (eds) Methods in Enzymology. Academic Press, California, pp. 380–382
Repetto M, Reides C, Gomez Carretero ML, Costa M, Griemberg G, Llesuy S (1996) Oxidative stress in blood of HIV infected patients. Clin Chim Acta 255(2):107–117
Benjamini Y, Hochberg J (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B 57(1):289–300
Kora P, Kalva SR (2015) Improved Bat algorithm for the detection of myocardia infarction. Springerplus 4:666. https://doi.org/10.1186/s40064-015-1379-7
Grollemund V, Pradat PF, Querin G, Delbot F, Le Chat G, Pradat-Peyre JF, Bede P (2019) Machine learning in amyotrophic lateral sclerosis: achievements, pitfalls, and future directions. Front Neurosci 13:135. https://doi.org/10.3389/fnins.2019.00135
Kraszula L, Jasinska A, Eusebio M, Kuna P, Glabinski A, Pietruczuk M (2012) Evaluation of the relationship between leptin, resistin, adiponectin and natural regulatory T cells in relapsing-remitting multiple sclerosis. Neurol. Neurochir Pol 46:22–28
Kallaur AP, Oliveira SR, Colado Simão AN, Delicato de Almeida ER, Kaminami Morimoto H, Lopes J, de Carvalho Jennings Pereira WL, Marques Andrade R, Muliterno Pelegrino L, Donizete Borelli S, Kaimen-Maciel DR, Reiche EM (2013) Cytokine profile in relapsing‑remitting multiple sclerosis patients and the association between progression and activity of the disease. Mol Med Rep 7(3):1010-20. https://doi.org/10.3892/mmr.2013.1256
Çoban A, Düzel B, Tüzün E, Tamam Y (2017) Investigation of the prognostic value of adipokines in multiple sclerosis. Multiple Sclerosis and Related Disorders 15:11–14. https://doi.org/10.1016/j.msard.2017.04.006
Zhang K, Guo Y, Ge Z, Zhang Z, Da Y, Li W, Zhang Z, Xue Z et al (2017) Adiponectin suppress T helper 17 differentiation and limits autoimmune CNS inflammation via the SIRT1/PPARγ/RORγ pathway. Mol Neurobiol 54:4908–4920. https://doi.org/10.1007/s12035-016-0036-7
Hietaharju A, Kuusisto H, Nieminen R, Vuolteenaho K, Elovaara I, Moilanen E (2010) Elevated cerebrospinal fluid adiponectin and adipsin levels in patients with multiple sclerosis: a Finnish co-twin study. Eur J Neurol 17:332–334
Penesova A, Vlcek M, Imrich R, Vernerova L, Marko A, Meskova M, Grunnerova L, Turcani P et al (2015) Hyperinsulinemia in newly diagnosed patients with multiple sclerosis. Metab Brain Dis 30(4):895–901. https://doi.org/10.1007/s11011-015-9665-1
Fissolo N, Cantó E, Vidal-Jordana A, Castilló J, Montalban X, Comabella M (2014) Levels of soluble TNF-RII are increased in serum of patients with primary progressive multiple sclerosis. J Neuroimmunol 271(1–2):56–59. https://doi.org/10.1016/j.jneuroim.2014.04.001
Varfolomeev E, Vucic D (2018) Intracellular regulation of TNF activity in health and disease. Cytokine 101:26–32. https://doi.org/10.1016/j.cyto.2016.08.035
Tseng W-Y, Huang Y-S, Lin H-H, Luo S-F, McCann F, McNamee K, Clanchy F, Williams R (2018) TNFR signaling and its clinical implications. Cytokine 101:19–25. https://doi.org/10.1016/j.cyto.2016.08.027
Yang S, Wang J, Brand DD, Zheng SG (2018) Role of TNF–TNF receptor 2 signal in regulatory T cells and its therapeutic implications. Front Immunol 9:784. https://doi.org/10.3389/fimmu.2018.00784
Gao H, Danzi MC, Choi CS, Taherian M, Dalby-Hansen C, Ellman DG, Madsen PM, Bixby JL et al (2017) Opposing functions of microglial and macrophagic TNFR2 in the pathogenesis of experimental autoimmune encephalomyelitis. Cell Rep 18(1):198–212. https://doi.org/10.1016/j.celrep.2016.11.083
Olmos G, Lladó J (2014) Tumor necrosis factor alpha: a link between neuroinflammation and excitotoxicity. Mediat Inflamm 2014:861231. https://doi.org/10.1155/2014/861231
Fiedler SE, George JD, Love HN, Kim E, Spain R, Bourdette D, Salinthone S (2017) Analysis of IL-6, IL-1β and TNF-α production in monocytes isolated from multiple sclerosis patients treated with disease modifying drugs. J Syst Integr Neurosci 3(3). https://doi.org/10.15761/JSIN.1000166
Fischer R, Maier O (2015) Interrelation of oxidative stress and inflammation in neurodegenerative disease: role of TNF. Oxidative Med Cell Longev 2015:610813. https://doi.org/10.1155/2015/610813
McCann FE, Perocheau DP, Ruspi G, Blazek K, Davies ML, Feldmann M, Dean JL, Stoop AA et al (2014) Selective tumor necrosis factor receptor I blockade is anti-inflammatory and reveals immunoregulatory role of tumor necrosis factor receptor II in collagen-induced arthritis. Arthritis Rheumatol 66(10):2728–2738. https://doi.org/10.1002/art.38755
Kvistad SS, Myhrn SS, Holmøy T, Benth JS, Wergeland S, Beiske AG, Bjerve KS, Hovdal H et al (2018) Serum levels of leptin and adiponectin are not associated with disease activity or treatment response in multiple sclerosis. J Neuroimmunol 323:73–77. https://doi.org/10.1016/j.jneuroim.2018.07.011
Pawlitzki M, Uebelhör J, Sweeney-Reed CM, Stephanik H, Hoffmann J, Lux A, Reinhold D (2018) Lower serum zinc levels in patients with multiple sclerosis compared to healthy controls. Nutrients 10(8):E967. https://doi.org/10.3390/nu10080967
Pan Z, Choi S, Ouadid-Ahidouch H, Yang JM, Beattie JH, Korichneva I (2017) Zinc transporters and dysregulated channels in cancers. Front Biosci 22:623–643
Socha K, Karpińska E, Kochanowicz J, Soroczyńska J, Jakoniuk M, Wilkiel M, Mariak ZD, Borawska MH (2017) Dietary habits, concentration of copper, zinc and Cu/Zn ratio in the serum and the ability status of patients with relapsing-remitting multiple sclerosis. Nutrition 40:76–81. https://doi.org/10.1016/j.nut.2017.03.009
Rosenkranz E, Maywald M, Hilgers RD, Brieger A, Clarner T, Kipp M, Plümäkers B, Meyer S et al (2016) Induction of regulatory T cells in Th1-/Th17-driven experimental autoimmune encephalomyelitis by zinc administration. J Nutr Biochem 29:116–123. https://doi.org/10.1016/j.jnutbio.2015.11.010
Bredholt M, Frederiksen JL (2016) Zinc in multiple sclerosis: a systematic review and meta-analysis. ASN Neuro 8(3). https://doi.org/10.1177/1759091416651511
Sanna A, Firinu D, Zavattari P, Valera P (2018) Zinc status and autoimmunity: a systematic review and meta-analysis. Nutrients 10(1):E68. https://doi.org/10.3390/nu10010068
Sheykhansari S, Kozielski K, Bill J, Sitti M, Gemmati D, Zamboni P, Singh AV (2018) Redox metals homeostasis in multiple sclerosis and amyotrophic lateral sclerosis: a review. Cell Death Dis 9:348. https://doi.org/10.1038/s41419-018-0379-2
Prasad AF (2014) An antioxidant and anti-inflammatory agent: role of zinc in degenerative disorders of aging. J Trace Elem Med Biol 28:364–371. https://doi.org/10.1016/j.jtemb.2014.07.019
Bao B, Ahmad A, Azmi A, Li Y, Prasad AS, Sarkar FH (2013) The biological significance of zinc in inflammation and aging. In: Rahman I, Bagchi D (eds) Inflammation, Advancing and Nutrition. NewYork, Elsevier Inc p, pp. 15–27
Funding
This study was funded, in part, by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mezzaroba, L., Simão, A.N.C., Oliveira, S.R. et al. Antioxidant and Anti-inflammatory Diagnostic Biomarkers in Multiple Sclerosis: A Machine Learning Study. Mol Neurobiol 57, 2167–2178 (2020). https://doi.org/10.1007/s12035-019-01856-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-019-01856-7