Abstract
Background
Continuous positive airway pressure (CPAP) is the treatment of choice for obstructive sleep apnoea (OSA). Long-term adherence is still an unsolved problem in this treatment, although different technical modifications for pressure application have been introduced. The only proven intervention to increase therapy adherence is an intensive training programme [1].
Subjects and methods
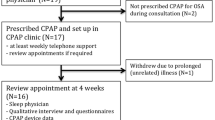
Eighty-four patients with the first diagnosis of OSA completed an intensive CPAP education programme during an in-hospital sleep laboratory stay. In this randomised prospective study the patients were treated as usual (control group) or enrolled in an outpatient training programme consisting of additional weekly telephone calls and an outpatient follow-up appointment with personal and technical support after 6 weeks. The mean daily use of CPAP was determined by reading off the internal clock of the devices, and daytime sleepiness was characterised using the Epworth Sleepiness Scale (ESS).
Results
In all, 22% of the patients rejected the therapy (mean use of less than 1 h per night). For the rest, the mean use of CPAP was 4.6± 2.7 h in the control group and 4.3± 1.8 h in the intervention group (no statistically significant difference).
Conclusion
After an intensive introduction to CPAP therapy in an inpatient environment, no increase in therapy adherence could be achieved via weekly telephone calls and a follow-up appointment.
Zusammenfassung
Hintergrund
Die Behandlung mit einem kontinuierlichen positiven Atemwegsdruck (CPAP) ist das etablierte Standardverfahren für die obstruktive Schlafapnoe (OSA). Allerdings ist die Langzeitadhärenz ein ungelöstes Problem, obwohl verschiedene technische Modifikationen der Druckapplikation in die Behandlung eingeführt worden sind. Eine Verbesserung der Adhärenz konnte bisher allein durch eine intensivierte Schulung erreicht werden.
Methoden
Während einer stationären Behandlung im Schlaflabor durchliefen 84 Patienten mit der erstmaligen Diagnose einer OSA ein intensives CPAP-Schulungsprogramm. In der randomisierten prospektiven Studie wurden die Patienten nach Entlassung entweder in üblicher Weise (Kontrollgruppe) oder in einem ambulanten Trainingsprogramm (Interventionsgruppe) betreut. Das ambulante Trainingsprogramm bestand aus wöchentlichen Telefonanrufen und einem Kontrolltermin mit ärztlicher und technischer Betreuung nach 6 Wochen. Die mittlere nächtliche Nutzung der CPAP-Therapie wurde über die in den Geräten befindlichen Speichermedien, die Schläfrigkeit über die Epworth Sleepiness Scale (ESS) ermittelt.
Ergebnisse
In der gesamten Gruppe haben 22% aller Patienten die Therapie abgebrochen (definiert als eine Nutzung von weniger als 1 h pro Nacht). Unter den Patienten, die die CPAP-Therapie nutzten, fand sich mit 4,3± 1,8 (Interventionsgruppe) versus 4,6± 2,7 h (Kontrollgruppe) kein Unterschied.
Schlussfolgerung
Nach einer intensiven Schulung der Patienten im Rahmen eines stationären Schlaflaboraufenthalts kann durch zusätzliche Schulungsmaßnahmen in Form von wöchentlichen telefonischen Kontakten und einem Kontrolltermin keine Steigerung der Adhärenz erreicht werden.



Similar content being viewed by others
References
Smith I, Nadig V, Lasserson TJ (2009) Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. Cochrane Database Syst Rev 15:CD007736
Lindberg E, Berne C, Elmasry A et al (2006) CPAP treatment of a population- based sample—what are the benefits and the treatment compliance? Sleep Med 7:553–560
Kribbs NB, Pack AI, Kline LR et al (1993) Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 147:887–895
Sin DD, Mayers I, Man GCW, Pawluk L (2002) Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea. Chest 121:430–435
Kasai T, Narui K, Dohi T et al (2008) Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 133:690–696
Milleron O, Pillière R, Foucher A et al (2004) Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Eur Heart J 25:709–711
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure, an observational study. Lancet 365:1046–1053
Buchner NJ, Sanner BM, Borgel J, Rump LC (2007) Continuous positive airway pressure treatment of mild to moderate obstructive sleep apnea reduces cardiovascular risk. Am J Respir Crit Care Med 176:1274–1280
Campos-Rodriguez F, Perez-Ronchel J, Grilo-Reina A et al (2007) Long-term effect of continuous positive airway pressure on BP in patients with hypertension and sleep apnea. Chest 132:1847–1852
Weaver TE, Maislin G, Dinges DF et al (2007) Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 30:711–719
Hoy CJ, Vennelle M, Kingshott RN et al (1999) Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med 159:1096–1100
Fischer J, Mayer G, Peter JH et al (2001) Nicht-erholsamer Schlaf. Leitlinie der dtsch. Ges. Schlafforschung und Schlafmedizin. Somnologie 5(Suppl 3)
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: brain information Service/Brain research Institute University of California 1968
ASDA Task Force (1992) EEG arousals: scoring rules and examples. Sleep 15:173–184
American Academy of Sleep Medicine Task Force (1999) Sleep 22:667–684
Kjelsberg FN, Ruud EA, Stavem K (2005) Predictors of symptoms of anxiety and depression in obstructive sleep apnea. Sleep Med 6:341–346
Chasens ER, Pack AI, Maislin G et al (2005) Claustrophobia and adherence to CPAP treatment. West J Nurs Res 27:307–321
Stepnowsky CJ Jr, Bardwell WA, Moore PJ et al (2002) Psychologic correlates of compliance with continuous positive airway pressure. Sleep 25:758
Broström A, Strömberg A, Mårtensson J et al (2007) Association of type D personality to perceived side effects and adherence in CPAP-treated patients with OSAS. J Sleep Res 16:439–447
Aloia MS, Arnedt JT, Stepnowsky C et al (2005) Predicting treatment adherence in obstructive sleep apnea using principles of behavior change. J Clin Sleep Med 1:346–353
Wild MR, Engleman HM, Douglas NJ, Espie CA (2004) Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J 24:461–465
Lewis KE, Seale L, Bartle IE et al (2004) Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep 27:134–138
Gay P, Weaver T, Loube D, Iber C (2006) Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 29:381–401
Budhiraja R, Parthasarathy S, Drake CL et al (2007) Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep 30:320–324
McArdle N, Devereux G, Heidarnejad H et al (1999) Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 159:1108–1114
Barbe F, Mayoralas LR, Duran J et al (2001)Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness. A randomized, controlled trial. Ann Intern Med 134:1015–1023
Drake CL, Day R, Hudgel D et al (2003) Sleep during titration predicts continuous positive airway pressure compliance. Sleep 26:308–311
Rosenthal L, Gerhardstein R, Lumley A et al (2000) CPAP therapy in patients with mild OSA: implementation and treatment outcome. Sleep Med 1:215–220
Lewis KE, Seale L, Bartle IE et al (2004) Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep 27:134–138
Hoffstein V, Viner S, Mateika S, Conway J (1992) Treatment of obstructive sleep apnea with nasal continuous positive airway pressure: patient compliance, perception of benefits, and side effects. Am Rev Respir Dis 145:841–845
Englemann HM, Asgari-Jirhandeh N, McLeod AL et al (1996) Self-reported use of CPAP and benefits of CPAP therapy. Chest 109:1470–1476
Reeves-Hoché MK, Hudgel DW, Meck R et al (1995) Continuous versus bilevel positive airway pressure for obstructive sleep apnea. Am J Respir Crit Care Med 151:443–449
Ayas NT, Patel SR, Malhotra A et al (2004) Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 27:249–253
Nilius G, Happel A, Domanski U, Rühle KH (2006) Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest 130:1018–1024
Duong M, Jayaram L, Camfferman D et al (2005) Use of heated humidification during nasal CPAP titration in obstructive sleep apnoea syndrome. Eur Respir J 26:679–685
Wiest GH, Harsch IA, Fuchs FS et al (2005) Initiation of CPAP therapy for OSA: does prophylactic humidification during CPAP pressure titration improve initial patient acceptance and comfort? Respiration 69:406–412
Mador MJ, Krauza M, Pervez A et al (2005) Effect of heated humidification on compliance and quality of life in patients with sleep apnea using nasal continuous positive airway pressure. Chest 128:2151–2158
Haffina M, Lasserson TJ, Smith I (2004) Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev 4:CD003531
Chervin RD, Theut S, Bassetti C, Aldrich MS (1997) Compliance with nasal CPAP can be improved by simple interventions. Sleep 20:284–289
Jean Wiese H, Boethel C, Phillips B et al (2005) CPAP compliance: video education may help! Sleep Med 6:171–174
Likar LL, Panciera TM, Erickson AD, Rounds S (1997) Group education sessions and compliance with nasal CPAP therapy. Chest 111:1273–1277
Hui DS, Chan JK, Choy DK et al (2000) Effects of augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest 117:1410–1416
Meurice JC, Ingrand P, Portier F et al (2007) A multicentre trial of education strategies at CPAP induction in the treatment of severe sleep apnoea-hypopnoea syndrome. Sleep Med 1:37–42
Richards D, Bartlett DJ, Wong K et al (2007) Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep 30:635–640
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nilius, G., Cottin, U., Domanski, U. et al. Effects of intensive outpatient training on the adherence of CPAP therapy for patients with OSA. Somnologie 16, 251–256 (2012). https://doi.org/10.1007/s11818-012-0580-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11818-012-0580-y
Keywords
- Adherence
- Continuous positive airway pressure
- Obstructive sleep apnoea
- Education
- Intensive training programme