Abstract
Background and Aims
Novel endoscopic procedures (endoscopic sleeve gastroplasty (ESG), AspireAssist (AA), and primary obesity surgery endolumenal (POSE)) have been developed for treatment of obesity. We aimed to conduct a systematic review and meta-analysis to evaluate and compare the efficacy of these three endoscopic procedures.
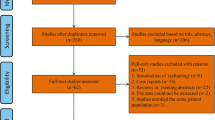
Methods
Main outcomes of interest were percent excess weight loss (%EWL) and percent total body weight loss (%TBWL). Weighted pooled means (WPMs) were calculated and analyzed using random effects model. Mean differences (MDs) were calculated to compare these procedures.
Results
Twelve studies with 1149 patients were included. WPMs for %EWL at 6 and 12 months with ESG were 49.67 (45.67, 53.66) and 52.75 (43.52, 61.98), respectively, while %TBWLs at 6 and 12 months with ESG were 16.01 (15.10, 16.92) and 17.41 (17.08, 17.74), respectively. WPMs for %EWL at 6 and 12 months with POSE were 43.79 (40.17, 47.42) and 44.91 (40.90, 48.92), respectively. WPM for %EWL at 12 months with AA was 50.85 (46.03, 55.68). While comparing ESG and POSE, at 6 months and 12 months, MD for %EWL was 6.17 (1.07, 11.26; P = 0.01) and 7.84 (− 2.05, 17.71; P = 0.06) in favor of ESG. No difference in %EWL was observed while comparing ESG with AA (P = 0.29). Likewise, MD for %EWL to compare AA and POSE was not significant (P = 0.68).
Conclusions
During a follow-up of 6–12 months, both AA and ESG had excellent efficacy in achieving significant and sustained weight loss; however, ESG was found to be superior in terms of weight loss when compared with POSE.






Similar content being viewed by others
References
World Health Organization. Obesity and overweight - fact sheet no. 312. Updated March 2013. www.who.int/mediacentre/factsheets/fs311/en/. Accessed 2 July 2018.
Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91.
CDC. Adult obesity causes & consequences. https://www.cdc.gov/obesity/adult/causes.html. Accessed 2 July 2018.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13(41):1–190. 215-357, iii-iv
Karlsson J, Taft C, Ryden A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31(8):1248–61.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Griffith PS, Birch DW, Sharma AM, et al. Managing complications associated with laparoscopic Roux-en-Y gastric bypass for morbid obesity. Can J Surg. 2012;55(5):329–36.
Jensen MD, Ryan DH. New obesity guidelines: promise and potential. JAMA. 2014;311(1):23–4.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–91.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
DG HJA. Chapter 8: assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions 2008;Version 5.0.1.
NIH. Quality assessment tool for before-after studies with no control group. National Institutes of Health Web site; 2014. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/before-after. Accessed 2 July 2018.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Sullivan S, Stein R, Jonnalagadda S, et al. Aspiration therapy leads to weight loss in obese subjects: a pilot study. Gastroenterology. 2013;145(6):1245–52. e1-5
Noren E, Forssell H. Aspiration therapy for obesity; a safe and effective treatment. BMC Obes. 2016;3:56.
Thompson CC, Abu Dayyeh BK, Kushner R, et al. Percutaneous gastrostomy device for the treatment of class II and class III obesity: results of a randomized controlled trial. Am J Gastroenterol. 2017;112(3):447–57.
Machytka EF H, Testoni P, Janssen I, et al. Aspiration therapy as a tool to treat obesity: one to four year results in a 160-patient multicenter post market registry study. Surg Obes Relat Dis. 2017;13:S57.
Abu Dayyeh BK, Acosta A, Camilleri M, et al. Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol. 2017;15(1):37–43 e1.
Lopez-Nava G, Galvao MP, Bautista-Castano I, et al. Endoscopic sleeve gastroplasty for obesity treatment: two years of experience. Arq Bras Cir Dig. 2017;30(1):18–20.
Sharaiha RZ, Kumta NA, Saumoy M, et al. Endoscopic sleeve gastroplasty significantly reduces body mass index and metabolic complications in obese patients. Clin Gastroenterol Hepatol. 2017;15(4):504–10.
Kumar N, Abu Dayyeh BK, Lopez-Nava Breviere G, et al. Endoscopic sutured gastroplasty: procedure evolution from first-in-man cases through current technique. Surg Endosc. 2018;32(4):2159–64.
Sullivan S, Swain JM, Woodman G, et al. Randomized sham-controlled trial evaluating efficacy and safety of endoscopic gastric plication for primary obesity: the ESSENTIAL trial. Obesity (Silver Spring). 2017;25(2):294–301.
Miller K, Turro R, Greve JW, et al. MILEPOST multicenter randomized controlled trial: 12-month weight loss and satiety outcomes after pose (SM) vs. medical therapy. Obes Surg. 2017;27(2):310–22.
Lopez-Nava G, Bautista-Castano I, Jimenez A, et al. The primary obesity surgery endolumenal (POSE) procedure: one-year patient weight loss and safety outcomes. Surg Obes Relat Dis. 2015;11(4):861–5.
Espinos JC, Turro R, Mata A, et al. Early experience with the incisionless operating platform (IOP) for the treatment of obesity : the primary obesity surgery endolumenal (POSE) procedure. Obes Surg. 2013;23(9):1375–83.
Lopez-Nava G, Sharaiha RZ, Vargas EJ, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg. 2017;27(10):2649–55.
Lopez-Nava G, Galvao MP, da Bautista-Castano I, et al. Endoscopic sleeve gastroplasty for the treatment of obesity. Endoscopy. 2015;47(5):449–52.
Breviere GLN, Bautista-Castano I, Fernandez-Corbelle JP, et al. Endoscopic sleeve gastroplasty (Apollo method): new approach in the treatment of obesity. Rev Esp Enferm Dig. 2016;108(4):201–6.
Lopez-Nava G, Galvao M, Bautista-Castano I, et al. Endoscopic sleeve gastroplasty with 1-year follow-up: factors predictive of success. Endosc Int Open. 2016;4(2):E222–7.
Lopez-Nava G, Galvao M, Bautista-Castaño I, et al. First results after endoscopic sleeve gastroplasty with a follow up time of 6 months. Obes Surg. 2014;24(8):1311–2.
Kumar N, Lopez-Nava G, Nicolle Peña Sahdala H, et al. Endoscopic sleeve gastroplasty: multicenter weight loss results. Gastroenterology. 2015;148(4):S179.
Kumar N, Sahdala HNP, Shaikh S, et al. Endoscopic sleeve gastroplasty for primary therapy of obesity: initial human cases. Gastroenterology. 2014;146(5):S571–S2.
Abu Dayyeh BK, Acosta A, Topazian M, et al. One-year follow-up and physiological alterations following endoscopic sleeve gastroplasty for treatment of obesity. Gastroenterology. 2015;148(4):S11–S2.
Lopez-Nava G, Manoel GN. Endoscopic sleeve gastroplasty using a modified plication method for weight loss. Gastrointest Endosc. 2014;79(5):AB362–AB3.
Lopez-Nava G, Neto Manoel G, Bautista-Castaño I, et al. First prospective endoscopic sleeve gastroplasty study at 1 year of follow up. Gastroenterology. 2015;148(4):S900–S1.
Lopez-Nava G, Sharaiha RZ, Galvao Neto M, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 242 patients with 18 months follow-up. Gastroenterology. 2016;150(4):S26.
Machytka E, Turro R, Huberty V, et al. Aspiration therapy in super obese patients-pilot trial. Gastroenterology. 2016;150(4):S822–S3.
Therapy AATFoEB, Ginsberg GG, Chand B, et al. A pathway to endoscopic bariatric therapies. Gastrointest Endosc. 2011;74(5):943–53.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;(8):CD003641.
Multicenter ESG Trial (MERIT): ClinicalTrials.gov Identifier: NCT03406975; 2018. https://clinicaltrials.gov/ct2/show/NCT03406975.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures and Conflict of Interest
Reem Z. Sharaiha is a consultant of BSC and Apollo Endosurgery. All other authors have no financial disclosures or conflicts of interest relevant to this study.
Ethical Approval
Systematic review and meta-analysis does not require formal consent.
Informed Consent
Informed consent does not apply to this systematic review and meta-analysis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix. Quality assessment of studies with NIH Quality assessment tool for before–after studies with no control group
Appendix. Quality assessment of studies with NIH Quality assessment tool for before–after studies with no control group
Criteria | Noren (2016) | Machytka (2017) | Abu Dayyeh (2017) | Lopez (2017) | Sharaiha (2017) | Kumar (2017) | Lopez (2014) | Espinos (2013) | |
|---|---|---|---|---|---|---|---|---|---|
1. Was the study question or objective clearly stated? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
2. Were eligibility/selection criteria for the study population prespecified and clearly described? | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | |
3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest? | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes | |
4. Were all eligible participants that met the prespecified entry criteria enrolled? | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes | |
5. Was the sample size sufficiently large to provide confidence in the findings? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
6. Was the test/service/intervention clearly described and delivered consistently across the study population? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
7. Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
8. Were the people assessing the outcomes blinded to the participants’ exposures/interventions? | No | No | No | No | No | No | No | No | |
9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p values for the pre-to-post changes? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
Result | Good | Fair | Good | Good | Good | Good | Good | Good | |
NIH, National Institutes of Health; N/A, not applicable | |||||||||
Quality assessment of randomized controlled trial using Cochrane tool for assessing risk of bias | |||||||||
Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | ||||
Sullivan (2017) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | |||
Miller (2017) | Low risk | High risk | High risk | Low risk | Low risk | Low risk | |||
Sullivan (2013) | Low risk | High risk | High risk | Low risk | Low risk | Low risk | |||
Thompson (2017) | Low risk | High risk | High risk | Low risk | Low risk | Low risk | |||
Rights and permissions
About this article
Cite this article
Khan, Z., Khan, M.A., Hajifathalian, K. et al. Efficacy of Endoscopic Interventions for the Management of Obesity: a Meta-analysis to Compare Endoscopic Sleeve Gastroplasty, AspireAssist, and Primary Obesity Surgery Endolumenal. OBES SURG 29, 2287–2298 (2019). https://doi.org/10.1007/s11695-019-03865-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03865-w