Summary
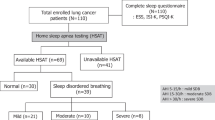
The possible relationship between lung cancer and nocturnal intermittent hypoxia, apnea and daytime sleepiness, especially the possible relationship between the occurrence and progression of lung cancer and obstructive sleep apnea syndrome (OSAS) was explored. Forty-five cases of primary lung cancer suitable for surgical resection at the Third Affiliated Hospital of Kunming Medical University between January 2017 and December 2017 were recruited (lung cancer group), and there were 45 patients in the control group who had no significant differences in age, sex and other general data from lung cancer group. The analyzed covariates included general situation, snore score, the Epworth Sleeping Scale (ESS), Pittsburgh Sleep Quality Index (PSQI), apnea and hypopneas index (AHI), oxygen desaturation index 4 (ODI4), lowest arterial oxygen saturation [LSpO2 (%)], oxygen below 90% of the time [T90% (min)], the percentage of the total recorded time spend below 90% oxygen saturation (TS90%), to explore the possible relationship between lung cancer and above indicators. The participants were followed up for one year. The results showed that: (1) There was significant difference in body mass index (BMI), ESS, AHI, T90% (min), TS90%, ODI4, snore score and LSpO2 (%) between lung cancer group and control group (P<0.05). There was no statistically significant difference in age, gender, PSQI score, incidence of concurrent hypertension, diabetes and coronary heart disease (CHD), and smoking history between the two groups (P>0.05); (2) Patients in the lung cancer group were divided into OSAS subgroup and non-OSAS subgroup according to the international standard for the diagnosis of OSAS. There was significant difference in BMI, age, staging, incidence of concurrent hypertension and concurrent CHD, snore score, ESS score, T90% (min), TS90%, ODI4 and LSpO2 (%) between OSAS subgroup and non-OSAS subgroup (P<0.05). There was no statistically significant difference in gender, PSQI score, incidence of concurrent diabetes, smoking history and lung cancer type between the two groups (P>0.05); (3) AHI was strongly negatively correlated with the LSpO2 (%) and positively with ESS, staging, snoring score, T90% (min), TS90%, ODI4 and BMI (P<0.05); (4) There were 3 deaths, 5 cases of recurrence, and 4 cases of metastasis in OSAS subgroup; and there was 1 death, 4 cases of recurrence and 2 cases of metastasis in non-OSAS subgroup during the follow-up period of one year, respectively. There was no significant difference in mortality, recurrence rate and metastasis rate between the two subgroups, and the total rate of deterioration in OSAS subgroup was significantly increased compared to the non-OSAS subgroup (P<0.05). It was concluded that the patients with lung cancer are prone to nocturnal hypoxemia, apnea, snoring and daytime sleepiness compared to control group. The incidence of OSAS in patients with lung cancer was higher, and the difference in the hypoxemia-related indicators was statistically significant. The mortality, recurrence rate, and metastasis rate increases in lung cancer patients with OSAS during the one-year follow-up period, suggesting that OSAS may be a contributing factor to the occurrence and progression of lung cancer.
Similar content being viewed by others
References
Garvey IF, Pengo MF, Drakatos P, et al. Epidemiological aspects of obstructive sleep apnea. J Thorac Dis, 2015, 7(5):920–929
Kiely JL, McNicholas WT. Cardiovascular risk factors in patients with obstructive sleep apnoea syndrome. Eur Respir J, 2000, 16(1): 128–133
Rice TB, Foster GD, Sanders MH, et al. The relationship between obstructive sleep apnea and self-reported stroke or coronary heart disease in overweight and obese adults with type 2 diabetes mellitus. Sleep, 2012, 35(9): 1293–1298
Martinez-Garcia MA, Campos-Rodriguez F, Barbe F. Cancer and OSA: Current Evidence From Human Studies. Chest, 2016, 150(2):451–463
Li L, Lu J, Xue W, et al. Target of obstructive sleep apnea syndrome merge lung cancer: based on big data platform. Oncotarget, 2017, 8(13): 21567–21578
Dreher M, Kruger S, Schulze-Olden S, et al. Sleep-disordered breathing in patients with newly diagnosed lung cancer. BMC Pulm Med, 2018, 18(1): 72
Almendros I, Wang Y, Becker L, et al. Intermittent hypoxia-induced changes in tumor-associated macrophages and tumor malignancy in a mouse model of sleep apnea. Am J Respir Crit Care Med, 2014, 189(5):593–601
Campillo N, Torres M, Vilaseca A, et al. Role of Cyclooxygenase-2 on Intermittent Hypoxia-induced Lung Tumor Malignancy in a Mouse Model of Sleep Apnea. Sci Rep, 2017,7: 44693
Khalyfa A, Almendros I, Gileles-Hillel A, et al. Circulating exosomes potentiate tumor malignant properties in a mouse model of chronic sleep fragmentation. Oncotarget, 2016, 7(34): 54676–54690
Nieto FJ, Peppard PE, Finn L, et al. Reply: sleep-disordered breathing, hypoxemia, and cancer mortality. Am J Respir Cnt Care Med, 2013, 187(3): 331–332
Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, et al. Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am JRespir Cnt Care Med, 2013, 187(1): 99–105
Shimoda LA, Semenza GL. HIF and the lung: role of hypoxia-inducible factors in pulmonary development and disease. Am J Respir Crit Care Med, 2011, 183(2): 152–156
Cortese R, Almendros I, Wang Y, et al. Mcroarray-based analysis of plasma cirDNA epigenetic modification profiling in xenografted mice exposed to intermittent hypoxia. Genom Data, 2015, 5: 17–20
Almendros I, Montserrat JM, Torres M, et al. Obesity and intermittent hypoxia increase tumor growth in a mouse model of sleep apnea. Sleep Med, 2012, 13(10): 1254–1260
Almendros I, Montserrat JM, Torres M, et al. Intermittent hypoxia increases melanoma metastasis to the lung in a mouse model of sleep apnea. Respir Physiol Neurobiol, 2013, 186(3): 303–307
Foster JG, Wong SC, Sharp TV. The hypoxic tumor microenvironment: driving the tumorigenesis of nonsmall-cell lung cancer. Future Oncol, 2014, 10(16): 2659–2674
Colten HR, Altevogt BM. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US). 2006.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985). 2005, 99(4): 1592–1599
Gozal D, Farre R, Nieto FJ. Putative Links Between Sleep Apnea and Cancer: From Hypotheses to Evolving Evidence. Chest, 2015, 148(5): 1140–1147
Giovannetti E, Wang Q, Avan A, etal. Role of CYB5A in pancreatic cancer prognosis and autophagy modulation. J Natl Cancer Inst, 2014, 106(1): djt346
Liu Y, Song X, Wang X, et al. Effect of chronic intermittent hypoxia on biological behavior and hypoxia-associated gene expression in lung cancer cells. J Cell Biochem, 2010, 111(3):554–563
Macey PM, Woo MA, Rajesh K, et al. Relationship between Obstructive Sleep Apnea Severity and Sleep, Depression and Anxiety Symptoms in Newly-Diagnosed Patients. PLoS One, 2010, 5(4): e10211
Mao ZF, Zhao TT, Wang ZN, et al. Influence of different hypoxia models on metastatic potential of SGC-7901 gastric cancer cells. Tumour Biol, 2014, 35(7):6801–6808
Hakim F, Wang Y, Zhang SX, et al. Fragmented sleep accelerates tumor growth and progression through recruitment of tumor-associated macrophages and TLR4 signaling. Cancer Res, 2014, 74(5): 1329–1337
Zielinski MR, Davis JM, Fadel JR, et al. Influence of chronic moderate sleep restriction and exercise on inflammation and carcinogenesis in mice. Brain Behav Immun, 2012, 26(4):672–679
Author information
Authors and Affiliations
Corresponding authors
Additional information
This project was supported by the National Natural Science Foundation of China (No. 81300064).
Conflict of Interest Statement
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, W., Luo, M., Fang, Yy. et al. Relationship between Occurrence and Progression of Lung Cancer and Nocturnal Intermittent Hypoxia, Apnea and Daytime Sleepiness. CURR MED SCI 39, 568–575 (2019). https://doi.org/10.1007/s11596-019-2075-6
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-019-2075-6