Abstract
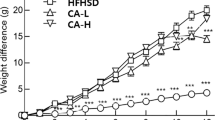
The present study evaluated the effects of asiatic acid (AA), a pentacyclic triterpenoid from Centella asiatica on lipid metabolism parameters in a rat model of obesity induced using a high fat diet (HFD) for 42 days. AA (20 mg/kg body weight [BW]) was administered orally once daily for 42 days, and an orlistat-treated group of rats (10 mg/kg BW) was included for comparison. Changes in BW, blood glucose levels, insulin resistance and leptin, adiponectin, amylase, and lipase levels in the blood; lipid profiles of plasma; liver antioxidants levels; and acetyl CoA carboxylase(ACC), uncoupling protein-2 (UCP2), and carnitine palmitoyltransferase-1 (CPT1) mRNA expression were observed in the experimental rats. Our results revealed that AA (20 mg/kg BW), similar to orlistat, reduced the increase in BW; increased bone mineral contents and bone mineral densities; reduced blood glucose levels, insulin resistance, leptin, plasma lipid levels; increased adiponectin, amylase, lipase levels in the blood; showed antioxidant activity; and altered mRNA expression of lipid metabolism-related genes, including ACC, UCP 2, and CPT 1, in the HFD-fed rats. From these results, we concluded that AA possesses significant anti-obesity potential through the suppression of BW gain, lipid lowering action, development of insulin and leptin sensitivity, antioxidant activity, and increased mRNA expression of lipid metabolism-related genes.
Graphical Abstract









Similar content being viewed by others
References
Despres JP (2012) Body fat distribution and risk of cardiovascular disease: an update. Circulation 126:1301–1313
Saravanan G, Ponmurugan P, Deepa MA, Senthilkumar B (2014) Anti-obesity action of gingerol: effect on lipid profile, insulin, leptin, amylase and lipase in male obese rats induced by a high-fat diet. J Sci Food Agric 94:2972–2977
Ferranti S, Mozaffarian D (2008) The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 54:6945–6955
Jindal A, Brietzke S, Sowers JR (2012) Obesity and the cardiorenal metabolic syndrome: therapeutic modalities and their efficacy in improving cardiovascular and renal risk factors. Car Ren Med 2(4):314–327
George M, Rajaram M, Shanmugam E (2014) New and emerging drug molecules against obesity. J Cardiovasc Pharmacol Ther 19(1):65–76
Colagiuri S (2010) Diabesity: therapeutic options. Diabetes Obes Metab 12:463–473
Kishino E, Ito T, Fujita K, Kiuchi Y (2006) A mixture of the Salacia reticulata (Kotala himbutu) aqueous extract and cyclodextrin reduces the accumulation of visceral fat mass in mice and rats with high-fat diet-induced obesity. J Nutr 136:433–439
Zhao Y, Shu P, Zhang Y, Lin L (2014) Effect of Centella asiatica on oxidative stress and lipid metabolism in hyperlipidemic animal models. Oxid Med Cell Longev 154:1–7
Huang SS, Chiu CS, Chen HJ, Hou WC, Sheu MJ, Lin YC, Shie PH, Huang GJ (2011) Antinociceptive activities and the mechanisms of anti-inflammation of asiatic acid in mice. Evid Based Complement Altern Med. doi:10.1155/2011/895857
Ramachandran V, Saravanan R, Senthilraja P (2014) Antidiabetic and antihyperlipidemic activity of asiatic acid in diabetic rats, role of HMG CoA: in vivo and in silico approaches. Phytomed 212:225–232
Ramachandran V, Saravanan R (2013) Asiatic acid prevents lipid peroxidation and improves antioxidant status in rats with streptozotocin-induced diabetes. J Funct Foods 5:1077–1087
Ji W, Zhao M, Wang M, Yan W, Liu Y, Ren S (2017) Effects of canagliflozin on weight loss in high-fat diet-induced obese mice. PLoS ONE 12(6): e0179960.
Buettner R, Schölmerich J, Bollheimer LC (2007) High-fat diets: modeling the metabolic disorders of human obesity in rodents. Obesity 15:798–808
Naidu PB, Uddandrao VS, Naik RR, Suresh P, Meriga B, Begum MS, Pandiyan R, Saravanan G (2016) Ameliorative potential of gingerol: promising modulation of inflammatory factors and lipid marker enzymes expressions in HFD induced obesity in rats. Mol Cell Endocrinol 419:139–147
Oben J, Kuate D, Agbor G, Momo C, Talla X (2006) The use of a Cissus quadrangularis formulation in the management of weight loss and metabolic syndrome. Lip Heal Dis 5:24
Srinivasan K, Patole PS, Kaul CL, Ramarao P (2004) Reversal of glucose intolerance by pioglitazone in high-fat diet fed rats. Exp Clin Pharmacol 26:327–333
Naidu PB, Ponmurugan P, Begum MS, Mohan K, Meriga B, Naik RR, Saravanan G (2015) Diosgenin reorganises hyperglycaemia and distorted tissue lipid profile in high-fat diet–streptozotocin-induced diabetic rats. J Sci Food Agric 95:3177–3182
Randle PJ, Garland PB, Hales CN, Newsholme EA (1963) The glucose fatty-acid cycle. Its role in insulin sensitivity andmetabolic disturbances in diabetes mellitus. Lancet 1:785–789
Saravanan G, Ponmurugan P (2012) Ameliorative potential of S-allylcysteine: effect on lipid profile and changes in tissue fattyacid composition in experimental diabetes. Exp Toxicol Pathol 64:639–644
Fungwe TV, Cagen LM, Cook GA (1993) Dietary cholesterol stimulated hepatic biosynthesis of triglyceride and reduces oxidation of fatty acids in the rat. J Lipid Res 34:933–941
Kim Y, Park T (2008) Genes are differentially expressed in the epididymal fat of rats rendered obese by a high-fat diet. Nutr Res 28:414–422
Zhou CJ, SongHuang JQ (2013) Sweet tea leaves extract improves leptin resistance in diet-induced obese rats. J Ethnopharm 145:386–392
Manuel TV, Sam JB (2007) Role of dietary so y protein in obesity. Int J Med Sci 4:72–82
Liu J, He T, Lu Q, Shang J, Sun H, Zhang L (2010) Asiatic acid preserves β cell mass and mitigates hyperglycemia in streptozocin-induced diabetic rats. Diabetes Metab Res Rev 26:448–454
Garg A (2006) Adipose tissue dysfunction in obesity and lipodystrophy. Clin Cornerstone 8:7–13
Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, Carr DR (2002) The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations. Diabetes 51:1005–1015
Arita Y, Kihara S, Ouchi N (1999) Paradoxical decrease of an adipose-specific protein, adiponectin in obesity. Biochem Biophys Res Commun 257:79–83
Kamohara S, Burcelin R, Halaas JL, Friedman JM, Charron MJ (1997) Acute stimulation of glucose metabolism in mice by leptin treatment. Nature 389:374–377
Staiger H, Haring HU (2005) Adipocytokines: fat-derived humoral mediators of metabolic homeostasis. Exp Clin Endocrinol Diabetes 113:67–79
Crozier A, Jaganath IB, Clifford MN (2009) Dietary phenolics: chemistry, bioavailability and effects on health. Nat Prod Rep 26:1001–1043
Ono Y, Hattori E, Fukaya Y, Imai S, Ohizumi Y (2006) Anti-obesity effect of Nelumbo nucifera leaves extract in mice and rats. J Ethnopharm 106:238–244
Nakajima K, Muneyuki T, Munakata H (2011) Revisiting the cardiometabolic relevance of serum amylase. BMC Res Not 4:419
Tundis R, Loizzo MR, Menichini F (2010) Natural products as alpha-amylase and alpha-glucosidase inhibitors and their hypoglycaemic potential in the treatment of diabetes: an update. Mini Rev Med Chem 10:315–331
Layer P, Rizza RA, Zinsmeister AR, Carlson GL, DiMagno EP (1986) Effect of a purified amylase inhibitor on carbohydrate tolerance in normal subjects and patients with diabetes mellitus. Mayo Clin Proce 61:442–447
Naidu PN, Uddandrao VS, Sasikumar V, Naik RR, Pothani S, Begum MS, Varatharaju C, Meriga B, Kalaivani A, Saravanan G (2017) Reversal of endothelial dysfunction in aorta of streptozotocinnicotinamide-induced type-2 diabetic rats by S-Allylcysteine. Mol Cell Biochem. doi:10.1007/s11010-017-2994-0
Jin D, Xua Y, Mei X (2013) Antiobesity and lipid lowering effects of theaflavins on high-fat diet induced obese rats. J Funct Foods 5:1142–1150
Park Y, Storkson JM, Liu W, Albright J, Cook ME, Pariza MW (2004) Structure–activity relationship of conjugated linoleic acid and its cognates in inhibiting heparin-releasable lipoprotein lipase and glycerol release from fully differentiated 3T3-L1 adipocytes. J Nutr Biochem 15:561–569
Torre-Villalvazo I, Tovar AR, Ramos-Barragan VE, Cerbon-Cervantes MA, Torres N (2008) Soy protein ameliorates metabolic abnormalities in liver and adipose tissue of rats fed a high fat diet. J Nutr 138:462–468
Garjani A, Fathiazad F, Zakheri A, Akbari NA, Azarmie Y (2009) The effect of total extract of Securigera securidaca L. seeds on serum lipid profiles, antioxidant status, and vascular function in hypercholesterolemic rats. J Ethnopharm 126:525–532
Yongqi G, Guanzhong W, Xin S, Hongxia Y, Juan Z (2009) Antiobesity action of a daidzein derivative on male obese mice induced by a high-fat diet. Nutr Res 29:656–663
Moller DE (2001) New drug targets for type 2 diabetes and the metabolic syndrome: a review. Nature 414:821–827
Uddandrao VS, Brahmanaidu P, Saravanan G (2016) Therapeutical perspectives of S-allylcysteine: effect on diabetes and other disorders in animal models. Car Hem Age Med Chem. doi:10.2174/1871525714666160418114120
Winterbourn CC (1995) Concerted antioxidant activity of glutathione and superoxide dismutase. In: Packer L, Fuchs J (eds) Biothiols in health and disease. Marcel Dekker Inc, New York, pp 117–134
Saravanan G, Ponmurugan P (2011) Ameliorative potential of S-allylcysteine on oxidative stress in STZ induced diabetic rats. Chem Biol Interact 189:100–106
Uddandrao VS, Brahmanaidu P, Meriga B, Saravanan G (2016) The potential role of S-allylcysteine as antioxidant against various disorders in animal models. Oxid Antioxid Med Sci 5(3):79–86
Naidu PB, Harishankar N, Meriga B, Pothana S, Sajjalaguddam RR (2015) Effects of Piper nigrum extracts: Restorative perspectives of high-fat diet-induced changes on lipid profile, body composition, and hormones in Sprague-Dawley rats. Pharm Biol 53(9):1318–1328
Naidu PB, Uddandrao VS, Pothani S, Naik RR, Begum MS, Varatharaju C, Pandiyan R, Saravanan G (2016) Effects of S-allylcysteine on biomarkers of polyol pathway in experimental type II diabetes in rats. Can J Diabetes 40:442–448
Van Herpen NA, Schrauwen-Hinderling VB (2008) Lipid accumulation in non-adipose tissue and lipotoxicity. Physiol Behav 94:231–241
Harbilas D, Braulta A, Valleranda D (2012) Populus balsamifera L. (Salicaceae) mitigates the development of obesity and improves insulin sensitivity in a diet-induced obese mouse model. J Ethnopharm 141:1012–1020
Wanga LJ, Zhang HW, Zhoua JY (2014) Betaine attenuates hepatic steatosis by reducing methylation of the MTTP promoter and elevating genomic methylation in mice fed a high-fat diet. J Nutr Biochem 25:329–336
Andrews ZB, Erion DM, Beiler R, Choi CS, Shulman GI, Horvath TL (2010) Uncoupling protein-2 decreases the lipogenic actions of ghrelin. Endocrinology 151:2078–2086
Ferre P, Foufelle F (2010) Hepatic steatosis: a role for de novo lipogenesis and the transcription factor SREBP-1c. Diabetes Obes Metab 12:83–92
Acknowledgements
The authors thank Muthyammal College of Arts and Science, Rasipuram, Tamilnadu, India, for providing facilities to do animal studies and also express heartfelt thanks to the management of K. S. Rangasamy College of Arts and Science, Tiruchengode, Tamilnadu, for their support and encouragement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures involving laboratory animals were in accordance with the guidelines of Committee for the purpose of control and supervision of experiments on animals (CPCSEA), Government of India, and institutional animal ethical committee of Muthyammal College of Arts and Science (Approval No: IAEC/MCAS/05/2016).
Rights and permissions
About this article
Cite this article
Rameshreddy, P., Uddandrao, V.V.S., Brahmanaidu, P. et al. Obesity-alleviating potential of asiatic acid and its effects on ACC1, UCP2, and CPT1 mRNA expression in high fat diet-induced obese Sprague–Dawley rats. Mol Cell Biochem 442, 143–154 (2018). https://doi.org/10.1007/s11010-017-3199-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3199-2