Abstract
The increasing rates of HIV infection that are currently being reported in high-income countries can be partly explained by migration from countries with generalized epidemics. Yet, early diagnosis of HIV/AIDS in immigrants remains a challenge. This study investigated factors that might be limiting immigrants’ access to HIV/AIDS care. Data from 268 legal immigrant students of two Swedish language schools in Northern Sweden were analyzed using logistic regression. Thirty-seven percent reported reluctance to seek medical attention if they had HIV/AIDS. Fear of deportation emerged as the most important determinant of reluctance to seek care after adjusting for socio-demographic factors, knowledge level, stigmatizing attitudes and fear of disclosure. Targeted interventions should consider the heterogeneity of migrant communities and the complex interplay of various factors which may impede access to HIV-related services. The myth about deportation because of HIV/AIDS should be countered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increasing numbers of reported HIV infections are being observed in high-income countries, it is thought due to migration from high-prevalence countries [1–4]. For instance, 43 percent of all new HIV cases reported in the European Union (EU) as acquired heterosexually in 2007 were migrants from high-prevalence countries [1]. However, there is also evidence of immigrants becoming infected after migration to EU countries [4–6]. Similarly, in Sweden, 54 percent of all new HIV infections reported in 2009 were immigrants from countries with generalized epidemics [5, 7].
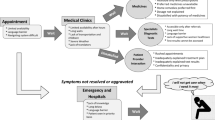
The current association between migration from high prevalence countries and the epidemiology of HIV has raised concerns in many receiving countries, where governments are responding by adopting laws and policies specifically targeting migrants [2–4, 8]. In Sweden, foreign-born persons from high risk countries are systematically offered a medical screening that also includes voluntary HIV-testing soon after arrival [9]. Furthermore, the Swedish Communicable Disease Act (2004:168), which classifies HIV infection and AIDS disease (HIV/AIDS) as ‘public health threats’ urges anyone who suspects being infected to consult a physician without delay for diagnosis and treatment, to assist clinicians in contact tracing and to protect others from the risk of infection including disclosing one’s HIV status to those at risk [10].
Most investigators acknowledge that care, treatment and prevention of HIV/AIDS in immigrants are influenced by a wide range of social, cultural and political factors [3, 8, 11–15]. Immigrants bring with them not only their disease profiles, but also their socio-demographic and cultural backgrounds. Thus, the meaning of HIV diagnosis and perceptions of people living with HIV/AIDS (PLWH) are likely to be grounded in the knowledge and experience from their country of birth [13, 15–17]. Additionally, immigrants living with HIV/AIDS may be unlikely to disclose their HIV status if they expect stigma and prejudice from their own/host communities [12, 16, 18–21]. Finally, concerns about deportation following disclosure of HIV status may impede contacts with official government agencies, including health care services [3, 8, 13, 21, 22]. In the present study we aim to assess the relationships between socio-demographic characteristics, HIV knowledge, stigma towards PLWH, fear of disclosure, fear of deportation and willingness to seek care.
Methods
Participants
Over the period October 2007 to September 2008, a total of 592 immigrants were registered as students in the Swedish for Immigrants’ (SFI: Svenska för Invandare) and Individual Programme’s Introductory Course (IVIK: Individuellt Program Introduktionskurs) in Umeå, a university town in Northern Sweden with about 111,600 inhabitants, including 9,577 immigrants. We adopted Statistics Sweden’s definition of an immigrant, which was: foreign-born, legally admitted, and expected to stay at least 12 months in Sweden [23].
The study followed the guidelines for ethical clearance provided by the Regional Ethical Review Board in Umeå, and its protocol was approved by the Doctoral Education Board (Faculty of Medicine) at Umeå University [24]. Permission was obtained from the principals of the schools before commencement. Participation in the study was voluntary, and written consent of parents/guardians was required for minors.
The schools were visited six times and, of the 592 students formally registered, 214 students were not included for various reasons such as: sick/parental leave, drop-outs, part-time students, or duplicate records. In addition, 69 students could not participate due to lack of interpreters for their languages (SFI: 10/276; IVIK: 23/102) or missing guardian’s consent (36/102)—this resulted in a sample of 309 students (SFI: 266/276 and IVIK: 43/102). We could not ascertain the reason for 29 students failing to participate. The analysis was thus based on 268 (96%) of the 280 individuals who completed the questionnaire, which gave an overall response rate of 71 percent (268/378—276 adults and 102 youths).
Data Collection
An original questionnaire developed by the first author, based on other Knowledge, Attitudes and Practices (KAP) surveys on HIV/AIDS, was pilot-tested, revised and then anonymously administered to participants [25–27]. It included 69 items concerning knowledge and beliefs about different aspects of HIV/AIDS, 17 items concerning attitudes towards PLWH and five items regarding fear of disclosure of HIV status (with which they could agree or disagree). Also added were a set of socio-demographic items and a series of items related to HIV/AIDS control in Sweden. The questionnaire was available in Swedish, English or French and language assistance was provided where necessary (in such cases, interpreters read and clarified items in the students’ vernacular). Of the 268 respondents, six were interviewed in Amharic, 71 in Arabic, 38 in Badinani, nine in Chinese, three in Dari, 28 in English, 22 in French, three in Japanese, 13 in Persian, 23 in Somali, four in Sorani, 13 in Spanish, eight in Swahili, 23 in Thai and four in Tigrinya.
Measures
In addition to the following socio-demographic variables: geographic origin, age, sex, years of education and having undergone medical screening/health check up or not, other variables included:
-
1.
HIV-knowledge score
For each individual item, correct answers were re-coded into ‘1’, and incorrect or ‘do not know’ into ‘0’. A single summary score for each topic was obtained by summing the number of correct responses to correlated items and dividing it by the total number of the items in the topic. An aggregate measure was then computed, summing the values of each of the nine topics, thus yielding a knowledge score for each participant. The score ranged from 0 to 9 with higher scores reflecting higher levels of knowledge. For the purpose of logistic regression analysis, the cumulative scores were further dichotomised into ‘low’ and ‘high’ levels of HIV knowledge. Respondents who scored at least six were coded as having ‘high/good’ knowledge and the remaining were coded as having ‘low/poor’ knowledge.
-
2.
Stigmatizing attitudes towards PLWH score
Attitudes towards PLWH were assessed through responses to three categories of correlated statements about attitudes towards PLWH. This construct measured “external” or enacted stigma which refers to perceptions, discriminatory attitudes and rejection of persons because of their confirmed or suspected HIV status [28]. The same process as for HIV knowledge was repeated and an attitude score for each participant was then generated, ranging from 0 to 3. Higher scores reflected lower levels of stigma. For the purpose of logistic regression analysis, the cumulative scores were dichotomized into ‘positive’ and ‘negative’ attitudes. Respondents who scored at least two were coded as having a ‘positive’ attitude (=0) and the remaining as having a ‘negative/stigmatizing’ attitude (=1).
-
3.
Fear of disclosure of HIV status
A new variable was created, based on respondents’ summary scores for answers to five attitudinal items about concerns or feelings of shame associated with disclosure of their own or a relative’s HIV status (range 0–1). This construct measured the expression of “internal” or felt stigma which refers to the shame and fear of being stigmatized or discriminated against associated with being HIV positive that affects PLWH and their family members [28]. The variable was further dichotomized by coding. Respondents who scored less than 0.7 overall were classified as ‘being afraid of disclosure’ (=1) and the remaining respondents as ‘not being afraid of disclosure’ (=0).
-
4.
Fear of deportation
Participants were asked whether they would fear being deported if they had HIV/AIDS. Participants who answered ‘Yes’ or ‘Don’t know’ were coded as ‘being insecure/afraid of expulsion’ (=1) and those who answered ‘No’ were coded as ‘not being afraid of expulsion’ (=0).
-
5.
Reluctance to seek HIV/AIDS care
Participants were asked whether they would be afraid to contact health care services if they had HIV/AIDS. Those who answered ‘Yes’ or ‘Don’t know’ were coded as ‘reluctant or uncertain to seek care’ (=1), and those who answered ‘No’ were coded as ‘not being reluctant to seek care’ (=0).
Analysis
Descriptive statistics were performed to summarise the data. To assess the relationships among variables logistic regression analyses (with 95 percent confidence intervals) were performed using the Statistical Package of Social Science (SPSS Inc, Chicago, IL) for Windows version 15.0. A P-value of <0.05 was considered statistically significant.
The association of key demographic variables with knowledge level was evaluated, treating all demographic characteristics as independent variables. Then, the same process was successively applied to ‘stigmatizing attitudes towards PLWH’, ‘fear of disclosure’, ‘fear of expulsion’ and ‘reluctance to seek care’. Thereafter, bivariate and multivariate analyses for the relationships between predictors and the dependent variable of interest, reluctance to seek care were performed.
Results
Sample Characteristics
The demographic characteristics of the 268 respondents are summarised in Table 1. Slightly more than half of participants were male (55%) and the mean age was 30 years for both men and women (range 16–63). Respondents originated from 133 different countries, but the majority (95%) originated from low-income countries. More than 70 percent of participants underwent medical screening that also included HIV testing. We believe that some tested positive, but HIV being such a sensitive issue we avoided to collect information regarding HIV status.
Knowledge About Different Aspects of HIV/AIDS
The mean and median HIV-knowledge scores for the sample were 4.9 and 5.3 respectively (SD = 2.2, maximum = 9). Only 34 percent of respondents were classified as having ‘high’ knowledge. Common misconceptions are summarized in Table 2.
The majority were aware of effective ways to prevent sexual transmission of HIV, with 76 percent mentioning the use of condoms, 70 percent citing a monogamous sexual relationship, and 62 percent mentioned abstinence. Nevertheless, some respondents wrongly agreed that birth pills (18%), spermicidal substances (16%) and taking a shower after sex (16%) could effectively prevent sexual transmission of HIV.
Nearly eight in ten respondents were aware that an HIV-positive test result means that a person is not only infected with HIV (79%) but also infectious (76%); however, about one in four equated it with imminent death (23%).
Respondents with fewer years of education (OR0–6 = 3.3, CI: 1.33–8.03, P = 0.010; OR7–12 = 2.8, CI: 1.25–6.46, P = 0.013) were more likely to have ‘low/poor’ HIV knowledge than were persons with more than 12 years. Of all geographic regions, only those from the Middle East (OR = 11.3, CI: 2.58–49.19, P = 0.001), were more likely to have ‘low/poor’ HIV knowledge compared with those from high income countries.
Attitudes Towards Persons Living with HIV/AIDS and Fear of Disclosure
Attitudinal items were grouped in two main categories to study the extent and ways in which stigmatizing attitudes towards the disease and those affected were expressed (Table 3). Overall, the mean and median attitude scores were 1.4 and 1.5 for stigmatizing attitudes towards PLWH (SD = 0.8, max = 3), and 0.4 (mean = median) for fear of disclosure (SD = 0.3, max = 1) respectively.
Although most respondents claimed that they would care for their sick relatives (69%) and not try to avoid contact with them (63%), merely 29 percent of respondents were classified as having a ‘low level’ of stigma.
Respondents from the Middle-East (OR = 37.02, CI: 7.40–185.28, P < 0.001), those with low level of education (OR0–6 = 5.9, CI: 2.01–17.39, P = 0.001; OR7–12 = 4.2, CI: 1.58–11.31, P = 0.004) were more likely to express stigmatizing attitude towards PLWH than those from high income countries and with high level (>12 years) of education.
Up to eight in 10 (80%) respondents were classified as ‘afraid’ or ‘uncertain’ about disclosure of their own, or a relative’s, HIV/AIDS status. Female respondents (OR = 4.2, CI: 1.71–10.16, P = 0.002), those with low levels (OR0–6 = 13.9, CI: 3.22–60.44, P < 0.001; OR7–12 = 5.1, CI: 1.78–14.56, P = 0.002) of education and those from the Middle East (OR = 6.1, CI: 1.36–27.43, P = 0.018) were more likely ‘to be afraid or uncertain about disclosure of HIV status’ than were male respondents and those with high level (>12 years) of education and those from high income countries.
Fear of Deportation and Reluctance to Seek Medical Attention
Nearly half (49%) of the group expressed concerns or insecurity about being deported because of an HIV diagnosis, and almost four in ten respondents (37%) stated that they would be reluctant or uncertain to seek medical attention if they had HIV/AIDS.
Youngest (16–24 years) respondents (OR = 4.9, CI: 1.41–16.99, P = 0.012), those from the Middle East (OR = 5.8, CI: 1.35–24.68, P = 0.018) and female respondents (OR = 2.2, CI: 1.12–4.16, P = 0.022) were more likely to fear or feel ambivalent about deportation because of an HIV/AIDS diagnosis than were the oldest (>45 years), males respondents and those from high income countries.
Predictors of Reluctance to Seek HIV/AIDS Care
Table 4 displays the results of both bivariate and multivariate analyses for the outcome of interest.
At the bivariate level, seven of the nine predictor variables were significant. Youngest respondents were more likely to be reluctant to seek care than were oldest (>45 years). Respondents with lowest education (0–6 years) and those from the Middle East were also more likely to be reluctant to seek care than were those with more than 6 years of education and those from high income countries. In addition, those who had poor HIV knowledge and those who expressed stigmatizing attitude towards PLWH were more likely to be reluctant to seek care than were those who had good knowledge and those who expressed tolerant attitudes. Finally, those who were afraid of disclosure and deportation were also more likely to be reluctant to seek care than were those who were not afraid. However, at the multivariate level, only respondents with lowest education (≤6 years), those who did not undergo medical screening and those who feared disclosure or deportation were likely to be reluctant to seek medical attention.
Discussion
Almost 40 percent of our respondents reported that they would be reluctant to seek medical attention if they had HIV/AIDS. Our respondents were neither asylum seekers nor undocumented migrants, but despite their ‘settled’ immigration status, the key factor associated with their reluctance to seek care was fear of deportation. For successful interventions, there is a need to better understand underlying factors that are critical for migrants’ decisions to seek care. In the current study, we have made some tentative assumptions regarding the role of certain of these factors on willingness to seek care
Low education and being from the Middle East were associated with a ‘low level’ of HIV knowledge. These findings first suggest a lack of access or poor understanding of available information for the low educated. Secondly, public education campaigns are not adequately targeting migrants from the Middle East in either their native countries or Sweden due to low prevalence as compared to other regions/subgroups where the epidemic is more prevalent [2, 21]. These findings stress the need to adjust HIV education and preventative efforts to include low-educated immigrants and those from countries with low HIV prevalence, as their vulnerability to HIV acquisition might also increase as a result of the immigration process [2, 4, 8, 11, 15, 29]. The positive relationship between higher level of HIV knowledge and willingness to seek care at the bivariate level may be the result of a greater understanding of the disease, thereby the benefits of seeking care.
It also appears that stigmatizing attitudes towards PLWH were positively associated with being from the Middle East. This could reflect the fact that migrants from regions, where HIV/AIDS is common are more familiar with both the disease and PLWH, and thus more tolerant than those from the Middle East where the disease is still a taboo and mainly concentrated in groups of people already stigmatized. Furthermore, low educated (≤12 years) respondents who were also found to have poor knowledge may be likely to hold misconceptions about different aspects of HIV/AIDS. This could result in more fear of transmission through casual contacts and more anxiety about their ability to protect themselves, and thus more stigmatizing attitudes towards PLWH [19, 30]. The positive relationship between stigmatizing attitudes and reluctance to seek care at the bivariate level suggests that those who hold negative attitude towards PLWH are also likely to have a negative attitude towards the disease itself if they were affected. These findings support other studies that underscore the role of education and increased understanding of HIV in tackling HIV-related stigma as well as the importance of dealing with it in the scheme of HIV/AIDS care and prevention efforts targeting immigrants [2, 13, 19, 22, 31].
Fear of disclosure which was more common among the less educated and those from the Middle East both who were found to have low level of HIV knowledge and to hold stigmatizing attitudes towards PLWH calls for knowledge-enhancing programmes targeting these groups to change their attitudes. The positive relationships between fear of disclosure and reluctance to seek care at both bivariate and multivariate levels suggest that tackling this fear could improve care seeking behaviour. These findings indicate that in a social context where HIV remains misunderstood, interventions promoting knowledge and correcting misconceptions about different aspects of HIV may reduce stigma and encourage disclosure, which is important for HIV care and prevention activities [14, 18, 19].
Furthermore, female respondents were more likely to fear disclosure of their HIV status and deportation because of HIV/AIDS than their male counterparts. In most of the respondents’ countries of origin, gender norms and social attitudes towards HIV and AIDS make women more vulnerable to the negative consequences of HIV and AIDS, in both familial and societal settings, and thus more reluctant to disclose and to return home [2, 16, 17, 19, 20, 32]—this calls for gender-specific interventions. However, fear of deportation which was common among youngest respondents and those from the Middle East might as well expresse concerns about a better future than HIV itself since the majority in this group originated from countries in conflict.
The most surprising findings to emerge from the present study is the strong association between fear of deportation and reluctance to seek care among this sample of ‘settled’ immigrants, which does not support most of the previous research findings [3, 8, 13, 16, 21, 22]. This urges policy makers to avoid conflating migration and HIV/AIDS control issues as it can undermine public health goals by inhibiting the very people at highest risk for HIV from seeking care [8, 21, 33]. The association between not being screened and being reluctant to seek care is an indication that contact with healthcare professionals during medical screening results in improved awareness about the benefit of seeking care.
Our findings also underscore the role of multiple factors on willingness to seek HIV-related care among this sample of settled migrants. These factors are likely to intervene through a web of causation, possibly explaining why some factors did not achieve significance at the multivariate level. Although much of the previous research has not supported fear of deportation as a predictor of health seeking behavior for legal migrants, we presume that its impact may be mediated by a series of intervening factors that are linked to each other. In fact, fear of deportation may be operating through a cognitive appraisal of negative consequences following disclosure of HIV that may be based on perceived social attitudes towards migrants in general and persons living with HIV/AIDS in particular, and individual’s knowledge about HIV/AIDS, which, in turn may be influenced by socio-demographic characteristics [8, 11, 12, 15, 17, 19, 21, 30, 34, 35]. Further examination of the relationships among predictors is warranted.
There are a number of limitations in this study: First, it cannot inform us about asylum seekers and undocumented migrants whose fear of deportation might be even greater than what is reported here. Second, although great efforts were made to overcome language, legal and educational barriers, speakers of minority languages and some younger respondents could not be included due to lack of interpreters. Third, the questionnaire used was primarily developed for the purpose of this particular study and might need further modification for use with other migrant groups. Fourth, duration of stay and HIV status were not obtainable for most respondents in this study, so their effects on unwillingness to seek care are unknown. Finally, the questions were posed in hypothetical terms rather than actual situations, which may be quite different since people often answer in terms of what they think is the ‘correct answer’ and may actually act otherwise. Despite the above-mentioned limitations, one of the main strengths of this study is that we could include immigrants from all regions of the world, particularly those with the highest rates of emigration, which may make our findings applicable to other high-income countries with a similar influx of immigrants from the same regions.
Conclusions
The increase in reported HIV infections among immigrant communities in high-income countries raises concerns about the need for targeted interventions. Policy makers and health professionals need to take into account the wide range and complexity of different factors that influence health-seeking behaviours. The myths about HIV, as well as fear of deportation, and gender role issues, need to be addressed. Meanwhile more health promotion work is needed to reduce the stigma, empower women and raise awareness about the benefits of seeking care.
References
European Centre for Disease Prevention and Control & WHO Regional Office for Europe. HIV/AIDS Surveillance in Europe 2007. Stockholm, Sweden. Surveillance Report; 2008. Available at: http://www.ecdc.eu.
UNAIDS/WHO: HIV Data. AIDS epidemic update 2009. Geneva, Switzerland. Available at: http://www.unaids.org/en/KnowlegdeCentre/HIVData/EpiUpdate/EpiUpdateArchive/2009/default.asp.
European Centre for Disease Prevention and Control. Migrant health—background note to the ‘ECDC Report on migration and infectious diseases in the EU’. Stockholm, Sweden. ECDC technical report; 2009. Available at: http://www.ecdc.europa.eu/en/publications/Publications/0907_TER_Migrant_health_Background_note.pdf.
European Centre for Disease Prevention and Control. Migrant health—epidemiology of HIV and AIDS in migrant communities and ethnic minorities in EU/EEA countries. Stockholm, Sweden. ECDC technical report; 2009. Available at: http://www.ecdc.europa.eu/en/publications/Publications/0907_TER_Migrant_health_HIV_Epidemiology_review.pdf.
The Swedish Institute for infectious Disease Control. Statistik för hivinfektion 2009. Stockholm, Sweden. Available at: http://www.smittskyddsinstitutet.se/statistik/hivinfektion/?t=com&p=15137#statistics-nav.
Kamga Wambo GO, Bätzing-Feigenbaum J, Hamouda O. HIV seroconversion following immigration in Germany – Analysis of reported HIV/AIDS cases among immigrants from Sub-Saharan Africa in Germany 2001–2008. Stockholm: European Scientific Conference on Applied Infectious Disease Epidemiology; 2009. Available at: http://escaide2009.ecdc.europa.eu/download.cfm-SAVE=2528&LG=1.pdf.
Wouters OJ, Arneborn M, Velicko I. An analysis of the Swedish HIV epidemic and the efficacy of contact tracing. Stockholm: European Scientific Conference on Applied Infectious Disease Epidemiology; 2009.
Amon JJ, Todrys KW. Fear of foreigners: HIV-related restrictions on entry, stay, and residence. J Int AIDS Soc. 2008; 11. doi:10.1186/1758-2652-11-8.
Government Offices of Sweden. UNGASS: Country progress report 2010. Sweden. Stockholm, Sweden. Available at: http://www.hivportalen.se/publikationer/Sidor/ungasscountryprogreereport2010sweden.aspx.
Swedish National Board of Health and Welfare. Smittspårning vid sexuellt överförbara infektioner., Västerås, Sweden. Socialstyrelsen; 2007.
Anderson J. Coming and going: some aspects of care for migrants with HIV in the UK. J Infect. 2008;57:11–15. doi:10.1016/j.jinf.2008.05.002.
Bhattacharya G. Health care seeking for HIV/AIDS among South Asians in the United States. Health Soc Work. 2004;29:106–15.
European Centre for Disease Prevention and Control. Migrant health—access to HIV prevention, treatment and care for migrant populations in EU/EEA countries. Stockholm, Sweden. ECDC technical report; 2009.
Levy V et al. Factors in the delayed HIV presentation of immigrants in Nothern California: implications for voluntary counselling and testing programs. J Immigr Health. 2006. doi:10.1007/s10903-006-9015-9.
Solskone V, Shtarkshall RA. Migration and HIV prevention programmes: linking structural factors, culture, and individual behaviour—an Israeli experience. Soc Sci Med. 2002;55:1297–307.
Körner H. HIV and migration: two major uncertainties for people from culturally and linguistically diverse backgrounds. National Centre in Social Research: social research issues paper 2005; 72. Available at: http://www.nchsr.unsw.edu.au/media/File/SRIP04.pdf.
Beyene Y. Potential HIV risk behaviors among Ethiopians and Eritreans in the diaspora: a bird’s-eye view. Northeast Afr J. 2000; 7:119–142. Available at: http://www.muse.jhu.edu/login?uri=/juornals/northeast_african_studies/v007/7.2/beyene.pdf DOI: 10.1353/nas.2004.0014.
Erwin J et al. Pathways to HIV testing and care by black African and white patients in London. Sex Transm Inf. 78:37–39. Available at: http://www.sti.bmj.com/content/78/1/37.full.html. doi:10.1136/sti.78.1.37.
Yang H, et al. HIV-related knowledge, stigma, and willingness to disclose: a mediation analysis. AIDS Care. 2006;18:717–24.
Maman S, Medley A. Gender dimensions of HIV status disclosure to sexual partners: rate, barriers and outcomes. Geneva: World Health Organization; 2003.
Fakoya I, Reynolds R, Caswell G, Shiripinda I. Barriers to HIV testing for migrant black African in Western Europe. HIV Med. 2008;2:23–5.
AIDS Community Research Initiative of America & Gay Men Health Crisis (ACRIA & GMHC). Race troubles. Why do African-Americans with HIV fare worse? Achieve 2009.
Statistics Sweden. Befolkningsstatistik 2006. Migration 2005. In-och utvandring och asylsökande. Örebro, Sweden. Statistika Centralbyrån; 2006. Available at: http://www.scb.se/Pages/PublishingCalendarViewInfo_259923.aspx?PublObjId=150.
Swedish Central Ethical Review Board. Förordning (2007:1069) med instruktion för regionala Etikprövningsnämnder. Stockholm, Sweden. Available at: www.epn.se/start/bakgroundbestaemmelser/lagar-och-foerordningar.aspx.
Family Health International. Implementing AIDS prevention and care project: behavioral surveillance surveys. Guidelines for repeated behavioral surveys in populations at risk of HIV. Family Health International; 2000.
Population Council. Horizons AIDSQuest: The HIV/AIDS survey library. Available at: http://www.popcouncil.org/horizons/AIDSQuest/cmnbehvrtheo/index/html.
POLICY Project. Siyam’kela: HIV/AIDS stigma indicators: a tool for measuring the progress of HIV/AIDS stigma mitigation. Pretoria, South Africa: POLICY; 2003. Available at: http://www.policyproject.com/Special/SA_stigma.pdf.
Brouard P, Wills C. A closer look: the internalization of stigma related to HIV. Wasington, DC: United States Agency for International Development (USAID); 2006. Available at: http://www.policyproject.com/pubs/generalreport/Internal_Stigma.pdf.
Swedish National Board of Health and Welfare. Migration och Sexuell Hälsa—En litteratur översikt om sexuellt risktagande och sexuellt riskutsatthet i samband med migration. Västra Aros, Sweden: Socialstyrelsen; 2010.
Tompkins M, Smith L, Jones K, Swindells S. HIV education needs among Sudanese immigrants and refugees in the Midwestern United States. AIDS Behav. 2006;10(3):323–91.
Parker R, Aggleton P. HIV/AIDS-related stigma and discrimination: a conceptual framework and an agenda for action. New York: Population Council; 2002.
AIDS Community Research Initiative of America (ACRIA). Focus on gender—women and HIV. 2008;17:1–20.
Coker R. Compulsory screening of immigrants for tuberculosis and HIV. Br Med J. 2004;28:298–300.
Chen N et al. Predictors of HIV testing among Latinos in Baltimore City. J Immgr Minor Health. 2009. doi:10.1007/s10903-009-9297-9.
Lazarus JV, Mohammed Himedan H, Rosendal Ostergaard L. HIV/AIDS knowledge and condom use among Somali and Sudanese immigrants in Denmark. Scand J Public Health. 2006;34:92–9.
Acknowledgements
Funding for this research was provided by the Swedish Council for Working Life and Social Research (FAS) within the Centre for Global Health Research Project of Umeå University (grant number 2006-1512), the Swedish Institute for Infectious Disease Control (grant number 640/2010/183), the County Council of Västerbotten, and the Medical Faculty of Umeå University. We also acknowledge the contributions and invaluable assistance in this study from: Hans Stenlund, for his comments on the statistical analysis; the school principals and all the staff members for their collaboration/cooperation; the MPH students for their assistance in data collection; and all the other students whose participation made this study possible.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Nkulu Kalengayi, F.K., Hurtig, AK., Ahlm, C. et al. Fear of Deportation May Limit Legal Immigrants’ Access to HIV/AIDS-Related Care: A Survey of Swedish Language School Students in Northern Sweden. J Immigrant Minority Health 14, 39–47 (2012). https://doi.org/10.1007/s10903-011-9509-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-011-9509-y