Abstract
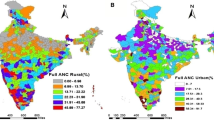
The present study identifies the prevalence, pattern & geographical distribution of pregnancy loss and its various determinants. The choropleth equal interval maps and local indicators of spatial association maps were used to investigate the locations requiring attention. Spatial regression techniques were used to investigate the factors associated with pregnancy losses across India using data derived from the fourth round of National Family Health Survey. A decision tree was constructed to investigate the interaction effect of the significant factors.The percentage of pregnancy loss in India is noted to be 14.3% (95% BCa confidence interval: 13.47, 14.79). The spatial autocorrelation coefficient (\(\rho = 0.61,~p < 0.001\)) indicated the spatial dependence in the data. Hotspots of response variable were observed in districts of Uttar Pradesh, Manipur, and Odisha. Locations, with high percentage of women who have attained education upto high school and above, women who did not want the pregnancy, and women whose family did not want more child, were likely to have increased percentage of pregnancy loss. Struggles in a womens life, family’s pressure and own desire to have child coupled with their education status are related to the pregnancy loss. Preventing the unplanned pregnancies will play a pivotal role in decreasing the pregnancy loss which further prevents maternal mortality and morbidity. Timely and adequate supplies of contraception in public health institutions particulary sub-centre, primary health centre should be ensured.

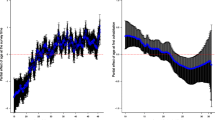
Source: Author created)

Source: Author created)

Source: Author created)

Source: Author created)

Source: Author created)
Similar content being viewed by others
Data availability
The data used in this study are available with the first and corresponding authors of this study and will be produced upon request.
References
Agyekum, P. D. (2015). Correlates of Pregnancy Loss Experiences in Ghana. University of Ghana, Doctoral dissertation.
Alhassan, A. Y., Abdul-Rahim, A., & Akaabre, P. B. (2016). Knowledge, awareness and perceptions of females on clandestine abortion in Kintampo North Municipality, Ghana. European Scientific Journal. https://doi.org/10.19044/esj.2016.v12n12p95
Anand, E., Unisa, S., & Singh, J. J. J. B. S. (2017). Intimate partner violence and unintended pregnancy among adolescent and young adult married women in south Asia. Journal of Biosocial Science, 49(2), 206–221.
Aparna, B., Kumari, S., & Devi, S. R. (2017). Socio demographic & obstetric profile of women undergoing prehospital induced abortion admitted at a tertiary care centre. JMSCR, 5(10), 29239–29243.
Bama, T. (2012). Assess The Factors Contributing To Pregnancy Loss During First and Second Trimester of Pregnancy among Post-Abortion Mothers admitted to the Postnatal Wards at Institute of Obstetrics and Gynecology, Chennai. College of Nursing, Madras Medical College, Chennai.
Banerjee, S., Gulati, S., Warvadekar, J., & Andersen, K. (2017). Abortion method, provider, and cost in transition: experience of Indian women seeking abortion over the last twelve years (2004–2015). Paper presented at the International Population Conference, Cape Town, South Africa, Oct.
Bennett, L. R. J. R. H. M. (2001). Single women’s experiences of premarital pregnancy and induced abortion in Lombok. Eastern Indonesia., 9(17), 37–43.
Blachowski, J. (2016). Application of GIS spatial regression methods in assessment of land subsidence in complicated mining conditions: Case study of the Walbrzych coal mine (SW Poland). Natural Hazards, 84(2), 997–1014.
Brown, S. S., & Eisenberg, L. (1995). The best intentions: Unintended pregnancy and the well-being of children and families. JAMA, 274(17), 1332–1332.
Chankapa, Y., Tsering, D., Kar, S., Basu, M., & Pal, R. (2011). Sociodemographic variables of contraceptive practice in Sikkim. Journal of Pharmacy and Bioallied Sciences, 3(3), 368.
Chattopadhyay, S., Mishra, A., & Jacob, S. (2018). ‘Safe’, yet violent? Women’s experiences with obstetric violence during hospital births in rural Northeast India. Culture, Health & Sexuality, 20(7), 815–829.
Cousens, S., Blencowe, H., Stanton, C., Chou, D., Ahmed, S., Steinhardt, L., Creanga, A. A., Tunçalp, Ö., Balsara, Z. P., Gupta, S., & Say, L. (2011). National, regional, and worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. The Lancet, 377(9774), 1319–1330.
De Silva, W. I., Dayananda, R. A., NishanthiPerera, N. J. A., & p. s. . (2006). Contraceptive behaviour of abortion seekers in Sri Lanka. Asian Population Studies, 2(1), 3–18.
Devi, I. T., Akoijam, B., Nabakishore, N., Jitendra, N., & Nonibala, T. (2007). Characteristics of primigravid women seeking abortion services at a referral center, Manipur. Indian Journal of Community Medicine, 32(3), 175.
Devi, K. P., Singh, L. R., Singh, L. B., Singh, M. R., & Singh, N. N. (2015). Postpartum hemorrhage and maternal deaths in north east india. Open Journal of Obstetrics and Gynecology, 5(11), 635.
Dhaded, S. M., Somannavar, M. S., Jacob, J. P., McClure, E. M., Vernekar, S. S., Kumar, S. Y., Kavi, A., Ramadurg, U. Y., Moore, J. L., Wallace, D. P., & Derman, R. J. (2018). Early pregnancy loss in Belagavi, Karnataka, India 2014–2017: a prospective population-based observational study in a low-resource setting. Reproductive Health, 15(1), 15–22.
DHIR, S. . (2015). REPRODUCTIVE FREEDOM: A HUMAN RIGHTS ISSUE WITH SPECIAL REFERENCE TO INDIA. Panjab University Chandigarh.
Englehardt, H. T. (1977). Ontology and ontogeny. The Monist. https://doi.org/10.5840/monist197760129
Fenster, L., Schaefer, C., Mathur, A., Hiatt, R. A., Pieper, C., Hubbard, A. E., Von Behren, J., & Swan, S. H. (1995). Psychologic stress in the workplace and spontaneous abortion. American Journal of Epidemiology, 142(11), 1176–1183.
Gober, P. (1994). Why abortion rates vary: A geographical examination of the supply of and demand for abortion services in the United States in 1988. Annals of the Association of American Geographers, 84(2), 230–250.
Govindasamy, P., & Ramesh, B. (1997). Maternal education and the utilization of maternal and child health services in India. International Institute for Population Sciences and Calverton, Maryland: Macro International Inc. NFHS Subject Reports. https://hdl.handle.net/10125/3472
Haddad, L. B., & Nour, N. M. (2009). Unsafe abortion: Unnecessary maternal mortality. Reviews in Obstetrics and Gynecology, 2(2), 122.
Hirve, S. S. (2004). Abortion law, policy and services in India: A critical review. Reproductive Health Matters, 12(sup24), 114–121.
Jejeebhoy, S. J. (2002). Convergence and divergence in spouses’ perspectives on women’s autonomy in rural India. Studies in Family Planning, 33(4), 299–308.
Jelen, T. G., & Wilcox, C. (2003). Causes and consequences of public attitudes toward abortion: A review and research agenda. Political Research Quarterly, 56(4), 489–500.
Joe, W., Mishra, U. S., & Navaneetham, K. (2008). Health inequality in India: evidence from NFHS 3. Economic and Political Weekly, 43(32), 41–47.
John, A., Nilima, Binu, V., & Unnikrishnan, B. (2019). Determinants of antenatal care utilization in India: a spatial evaluation of evidence for public health reforms. Public Health, 166, 57–64.
Johnson-Hanks, J. (2002). The lesser shame: Abortion among educated women in southern Cameroon. Social Science & Medicine, 55(8), 1337–1349.
Kalyanwala, S., Zavier, A. F., Jejeebhoy, S., Kumar, R. J. I. P. o. S., & Health, R. (2010). Abortion experiences of unmarried young women in India: evidence from a facility-based study in Bihar and Jharkhand. 36(2), 62–71.
Kapil Ahmed, M., Van Ginneken, J., Razzaque, A. J. T. M., & Health, I. (2005). Factors associated with adolescent abortion in a rural area of Bangladesh. Tropical Medicine & International Health, 10(2), 198–205.
Kelkar, R. (1974). Impact of the Medical Termination of Pregnancy Act, 1971: A Case Study. Journal of the Indian Law Institute, 16(4), 593–625.
Khan, M. A., Nilima, N., Prathibha, J., Tiwary, B., & Singh, M. (2020). Documentation compliance of in-patient files: A cross sectional study from an east India state. Clinical Epidemiology and Global Health, 8(4), 994–997.
MacDorman, M. F., & Gregory, E. C. (2015). Fetal and perinatal mortality: United States, 2013. National vital statistics reports.64(8). DHHS publication(PHS) 2015–1120.
Magnus, M. C., Wilcox, A. J., Morken, N.-H., Weinberg, C. R., & Håberg, S. E. J. b. (2019). Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. 364, 1869.
McClure, E. M., Goldenberg, R. L., & Bann, C. M. (2007). Maternal mortality, stillbirth and measures of obstetric care in developing and developed countries. International Journal of Gynecology & Obstetrics, 96(2), 139–146.
Nilima, Kamath, A., Shetty, K., Unnikrishnan, B., Kaushik, S., & Rai, S. N. (2018). Prevalence, patterns, and predictors of diarrhea: A spatial-temporal comprehensive evaluation in India. BMC Public Health, 18(1), 1–10.
Nilima, N., Kaushik, S., Tiwary, B., & Pandey, P. K. (2020). Psycho-social factors associated with the nationwide lockdown in India during COVID-19 pandemic. Clinical Epidemiology and Global Health, 9, 47–52.
Nilima, A., Puranik, S. M., Shreenidhi, S., & Rai, S. (2020). Spatial evaluation of prevalence, pattern and predictors of cervical cancer screening in India. Public Health, 178, 124–136.
Patki, A., & Chauhan, N. J. T. J. (2016). An epidemiology study to determine the prevalence and risk factors associated with recurrent spontaneous miscarriage in India. The Journal of Obstetrics and Gynecology of India, 66(5), 310–315.
Pintye, J., Beima-Sofie, K. M., Kimemia, G., Ngure, K., Trinidad, S. B., Heffron, R., Baeten, J., Odoyo, J., Mugo, N., Bukusi, E. A., & Kelley, M. C. (2017). “I did not want to give birth to a child who has HIV”: Experiences using PrEP during pregnancy among HIV-uninfected Kenyan women in HIV-serodiscordant couples. Journal of acquired immune deficiency syndromes (1999), 76(3), 259.
Powell-Griner, E., & Trent, K. (1987). Sociodemographic determinants of abortion in the United States. Demography. https://doi.org/10.2307/2061391
Rahman, M., DaVanzo, J., & Razzaque, A. J. T. L. (2001). Do better family planning services reduce abortion in Bangladesh? The Lancet, 358(9287), 1051–1056.
Rao, N. (2012). Male ‘providers’ and female ‘housewives’: A gendered co-performance in rural North India. Development and Change, 43(5), 1025–1048.
Ravindran, T. (2002). Gender Gaps in Research on Abortion in India: A critical review of selected studies. The Gender and Reproductive Health Research Initiative. CREA. New Delhi, 1–28.
Regan, L., & Rai, R. (2000). Epidemiology and the medical causes of miscarriage. Best Practice & Research Clinical Obstetrics & Gynaecology, 14(5), 839–854.
Regan, W., & Morrey, B. J. O. T. D. (2008). Fractures of the coronoid process of the ulna. Orthopedic Trauma Directions, 6(02), 33–37.
Rowlands, M. (2011). Arguments from Intuition in Judith Jarvis Thomson’s a Defense of Abortion and Ronald Dworkin’s Life’s Dominion. UCL Jurisprudence Rev., 17, 1.
Sarkar, N. (1990). Psycho-social factors influencing decisions to accept termination of pregnancy in Delhi. Biology and Society: the Journal of the Eugenics Society, 7(2), 95–100.
Sathar, Z. A., Singh, S., & Fikree, F. F. (2007). Estimating the incidence of abortion in Pakistan. Studies in Family Planning, 38(1), 11–22.
Shaikh, Z., Abbassi, R. M., Rizwan, N., & Abbasi, S. (2010). Morbidity and mortality due to unsafe abortion in Pakistan. International Journal of Gynecology & Obstetrics, 110(1), 47–49.
Shekhar, C., Sundaram, A., Hussain, R., Pradhan, M. R., & Kalyanwala, S. (2018). Unintended pregnancy, abortion and postabortion care in UTtar Pradesh, India—2015. In: New York: Guttmacher Institute.
Silverman, J. G., Gupta, J., Decker, M. R., Kapur, N., & Raj, A. (2007). Intimate partner violence and unwanted pregnancy, miscarriage, induced abortion, and stillbirth among a national sample of Bangladeshi women. BJOG: An International Journal of Obstetrics & Gynaecology, 114(10), 1246–1252.
Singh, S., Cabigon, J. V., Hossain, A., Kamal, H., & Perez, A. E. (1997). Estimating the level of abortion in the Philippines and Bangladesh. International Family Planning Perspectives. https://doi.org/10.2307/2950765
Singh, S., Shekhar, C., Acharya, R., Moore, A. M., Stillman, M., Pradhan, M. R., Frost, J. J., Sahoo, H., Alagarajan, M., Hussain, R., & Sundaram, A. (2018). The incidence of abortion and unintended pregnancy in India, 2015. The Lancet Global Health, 6(1), e111–e120.
Singh, S., Sundaram, A., Hossain, A., Puri, M. C., Sathar, Z., Shekhar, C., Crowell, M., & Moore, A. M. (2020). Abortion Service Provision in South Asia: A Comparative Study of Four Countries. Contraception, 102(3), 210–219.
Swain, P. K., Jena, A., & Priyadarshini, S. J. (2021). An Analysis of Trend, Pattern, and Determinants of Abortion, Miscarriage, and Stillbirths in Odisha, India. Journal of Population and Social Studies [JPSS], 29, 223–234.
Thonneau, P. F. (2001). Maternal mortality and unsafe abortion: a heavy burden for developing countries. Safe motherhood strategies: a review of the evidence. Studies in HSO&P,17.
Tiwary, B., Nilima, N., Majumdar, P., Singh, M., & Khan, M. A. (2020). Quality of services provided by public funded ambulance program: Experience from a northern state in India. Clinical Epidemiology and Global Health, 8(3), 962–966.
Torres, A., & Forrest, J. D. (1988). Why do women have abortions? Family Planning Perspectives. https://doi.org/10.2307/2135792
Wang, X., Chen, C., Wang, L., Chen, D., Guang, W., French, J. & Reproductive Health Study Group. (2003). Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertility and Sterility, 79(3), 577–584.
Warburton, D., & Fraser, F. C. (1964). Spontaneous abortion risks in man: data from reproductive histories collected in a medical genetics unit. American Journal of Human Genetics., 16(1), 1.
World Health Organization. (1993). The Prevention and management of unsafe abortion: report of a technical working group, Geneva, 12–15 April 1992. (No. WHO/MSM/92.5. Unpublished). World Health Organization.
Young, B. K. (2019). A multidisciplinary approach to pregnancy loss: the pregnancy loss prevention center. Journal of Perinatal Medicine, 47(1), 41–44.
Acknowledgements
The authors would like to acknowledge Mr. Rahul Singh (B.Tech, Mechanical Engineering) for proof reading this article.
Funding
None.
Author information
Authors and Affiliations
Contributions
BT conceptualized the study. AK extracted the data and was involved in the cleaning process. NN carried out statistical analysis and created the plots. BT, NN & SKwrote the manuscript. PKP and MAK did a critical review of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that there is no conflict of interest.
Ethical approval
The article uses freely available secondary data obtained from http://rchiips.org under the National Data sharing and Accessibility Policy of Government of India. Hence an ethical clearance was not deemed necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tiwary, B., Nilima, N., Kumar, A. et al. Spatial evaluation of pregnancy loss among child-bearing women in India. GeoJournal 87, 3815–3826 (2022). https://doi.org/10.1007/s10708-021-10464-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-021-10464-9