Abstract
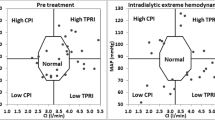
Intradialytic hypotensive events (IDH) accompanied by deleterious decreases of the cardiac output complicate up to 25% of hemodialysis treatments. Monitoring options available to track hemodynamic changes during hemodialysis have been found ineffective to anticipate the occurrence of IDH. We have assembled opto-electronic instrumentation that uses the fluorescence of a small bolus of indocyanine green dye injected in the hemodialysis circuit to estimate cardiac output and blood volume based on indicator dilution principles in patients receiving hemodialysis. The instrument and technique were tested in 24 adult end-stage renal failure subjects during 64 hemodialysis sessions. A single calibration factor could be used across subjects and across time. Intra-subject variability of the measurements over time was <10%. Stroke volume index (SVI) (mean ± SEM = 34 ± 1 vs. 39 ± 2 mL m−2) and central blood volume (CBV) index (783 ± 36 vs. 881 ± 33 mL m−2) were lower at the beginning of the sessions in which IDH eventually occurred. Cardiac index, SVI, and CBV index decreased with hemodialysis in all treatment sessions but the decrease was more intense in the IDH sessions. We conclude that hemodynamic monitoring can be implemented in patients receiving hemodialysis with minimal disruption of the treatment and could help understand intradialytic hypotension.






Similar content being viewed by others
References
Boon, D., G. A. van Montfrans, M. G. Koopman, R. T. Krediet, and W. J. W. Bos. Blood pressure response to uncomplicated hemodialysis: the importance of changes in stroke volume. Nephron Clin. Pract. 96:c82–87, 2004.
Booth, J., J. Pinney, and A. Davenport. Do changes in relative blood volume monitoring correlate to hemodialysis-associated hypotension? Nephron Clin. Pract. 117:c179–183, 2011.
Bos, W. J., S. Bruin, R. W. van Olden, I. Keur, K. H. Wesseling, N. Westerhof, R. T. Krediet, and L. A. Arisz. Cardiac and hemodynamic effects of hemodialysis and ultrafiltration. Am. J. Kidney Dis. 35:819–826, 2000.
Cavalcanti, S., S. Cavani, and A. Santoro. Role of short-term regulatory mechanisms on pressure response to hemodialysis-induced hypovolemia. Kidney Int. 61:228–238, 2002.
Compton, F., C. Hoffmann, W. Zidek, S. Schmidt, and J.-H. Schaefer. Volumetric hemodynamic parameters to guide fluid removal on hemodialysis in the intensive care unit. Hemodial. Int. 11:231–237, 2007.
Dasselaar, J. J., R. H. J. A. Slart, M. Knip, J. Pruim, R. A. Tio, C. W. McIntyre, P. E. de Jong, and C. F. M. Franssen. Haemodialysis is associated with a pronounced fall in myocardial perfusion. Nephrol. Dial. Transplant. 24:604–610, 2009.
Daugirdas, J. T. Dialysis hypotension: a hemodynamic analysis. Kidney Int. 39:233–246, 1991.
Dheenan, S., and W. L. Henrich. Preventing dialysis hypotension: a comparison of usual protective maneuvers. Kidney Int. 59:1175–1181, 2001.
Godje, O., M. Peyerl, T. Seebauer, O. Dewald, and B. Reichart. Reproducibility of double indicator dilution measurements of intrathoracic blood volume compartments, extravascular lung water, and liver function. Chest 113:1070–1077, 1998.
Hoeft, A., B. Schorn, A. Weyland, M. Scholz, W. Buhre, E. Stepanek, S. J. Allen, and H. Sonntag. Bedside assessment of intravascular volume status in patients undergoing coronary bypass surgery. Anesthesiology 81:76–86, 1994.
Imai, T., K. Takahashi, H. Fukura, and Y. Morishita. Measurement of cardiac output by pulse dye densitometry using indocyanine green: a comparison with the thermodilution method. Anesthesiology 87:816–822, 1997.
Kolb, J., T. M. Kitzler, T. Tauber, N. Morris, F. Skrabal, and P. Kotanko. Proto-dialytic cardiac function relates to intra-dialytic morbid events. Nephrol. Dial. Transplant. 26:1645–1651, 2011.
Kooman, J., A. Basci, F. Pizzarelli, B. Canaud, P. Haage, D. Fouque, K. Konner, A. Martin-Malo, L. Pedrini, J. Tattersall, J. Tordoir, M. Vennegoor, C. Wanner, P. ter Wee, and R. Vanholder. EBPG guideline on haemodynamic instability. Nephrol. Dial. Transplant. 22(Suppl 2):ii22–ii44, 2007.
Kron, J., D. Schneditz, T. Leimbach, S. Aign, and S. Kron. A simple and feasible method to determine absolute blood volume in hemodialysis patients in clinical practice. Blood Purif. 38:180–187, 2014.
Kron, S., D. Schneditz, T. Leimbach, J. Czerny, S. Aign, and J. Kron. Determination of the critical absolute blood volume for intradialytic morbid events: critical absolute blood volume. Hemodial. Int. 20:321–326, 2016.
Kron, S., R. Wenkel, T. Leimbach, S. Aign, and J. Kron. Effects of sodium on measuring relative blood volume during hemodialysis differ by techniques. ASAIO J. 59:612–616, 2013.
Leypoldt, J. K., A. K. Cheung, R. R. Steuer, D. H. Harris, and J. M. Conis. Determination of circulating blood volume by continuously monitoring hematocrit during hemodialysis. J. Am. Soc. Nephrol. 6:214–219, 1995.
Lichtwarck-Aschoff, M., R. Beale, and U. J. Pfeiffer. Central venous pressure, pulmonary artery occlusion pressure, intrathoracic blood volume, and right ventricular end-diastolic volume as indicators of cardiac preload. J. Crit. Care 11:180–188, 1996.
Lindsay, R. M., T. Shulman, S. Prakash, G. Nesrallah, and M. Kiaii. Hemodynamic and volume changes during hemodialysis. Hemodial. Int. 7:204–208, 2003.
Maarek, J.-M. I., and D. P. Holschneider. Estimation of indocyanine green concentration in blood from fluorescence emission: application to hemodynamic assessment during hemodialysis. J. Biomed. Opt. 14:054006, 2009.
Maarek, J.-M. I., D. P. Holschneider, J. Harimoto, J. Yang, O. U. Scremin, and E. H. Rubinstein. Measurement of cardiac output with indocyanine green transcutaneous fluorescence dilution technique. Anesthesiology 100:1476–1483, 2004.
Maarek, J.-M. I., D. P. Holschneider, and E. H. Rubinstein. Fluorescence dilution technique for measurement of cardiac output and circulating blood volume in healthy human subjects. Anesthesiology 106:491–498, 2007.
Maarek, J.-M. I., D. P. Holschneider, J. Yang, S. N. Pniak, and E. H. Rubinstein. Transcutaneous fluorescence dilution cardiac output and circulating blood volume during hemorrhagic hypovolemia. Anesthesiology 102:774–782, 2005.
MacRae, J. M., G. Joseph, V. Kislukhin, N. M. Krivitski, A. P. Heidenheim, and R. M. Lindsay. Determining lung water volume in stable hemodialysis patients. ASAIO J. 52:430–437, 2006.
Mitra, S., P. Chamney, R. Greenwood, and K. Farrington. Serial determinations of absolute plasma volume with indocyanine green during hemodialysis. J. Am. Soc. Nephrol. 14:2345–2351, 2003.
Nakamura, Y., T. Ikeda, S. Takata, H. Yokoi, M. Hirono, T. Abe, E. Takazakura, and K. Kobayashi. The role of peripheral capacitance and resistance vessels in hypotension following hemodialysis. Am. Heart J. 121:1170–1177, 1991.
Nette, R. W., M. A. van den Dorpel, H. P. Krepel, E. H. Y. Ie, A. H. van den Meiracker, D. Poldermans, W. Weimar, and R. Zietse. Hypotension during hemodialysis results from an impairment of arteriolar tone and left ventricular function. Clin. Nephrol. 63:276–283, 2005.
Prakash, S., D. Reddan, A. P. Heidenheim, C. Kianfar, and R. M. Lindsay. Central, peripheral, and other blood volume changes during hemodialysis. ASAIO J. 48:379–382, 2002.
Schneditz, D., B. Haditsch, A. Jantscher, W. Ribitsch, and P. Krisper. Absolute blood volume and hepatosplanchnic blood flow measured by indocyanine green kinetics during hemodialysis. ASAIO J. 60:452–458, 2014.
Selby, N. M., and C. W. McIntyre. The acute cardiac effects of dialysis. Semin. Dial. 20:220–228, 2007.
van der Sande, F. M., G. Wystrychowski, J. P. Kooman, L. Rosales, J. Raimann, P. Kotanko, M. Carter, C. T. Chan, K. M. L. Leunissen, and N. W. Levin. Control of core temperature and blood pressure stability during hemodialysis. Clin. J. Am. Soc. Nephrol. 4:93–98, 2009.
Wallin, C.-J. B., P. Rossi, S. H. Jacobson, and L. G. Leksell. Central blood volume, atrial natriuretic peptide and intermittent hemodialysis. Scand. J. Urol. Nephrol. 38:78–84, 2004.
Wynne, J. L., L. O. Ovadje, C. M. Akridge, S. W. Sheppard, R. L. Vogel, and J. M. Van de Water. Impedance cardiography: a potential monitor for hemodialysis. J. Surg. Res. 133:55–60, 2006.
Yang, N.-I., C.-H. Wang, M.-J. Hung, Y.-C. Chen, I.-W. Wu, C.-C. Lee, M.-S. Wu, L.-T. Kuo, C.-W. Cheng, and W.-J. Cherng. Real-time three-dimensional echocardiography provides advanced haemodynamic information associated with intra-dialytic hypotension in patients with autonomic dysfunction. Nephrol. Dial. Transplant. 25:249–254, 2010.
Acknowledgments
This study was supported by in part by the Alfred E. Mann Institute for Biomedical Engineering at the University of Southern California, the NIH/NHLBI (Grant R01 HL103765), and the NIH/NCRR SC-CTSI (Grant UL1 RR031986). The authors thank Ms. Radhika Ananthakrishna and Ms. Yeasmin Nazmay for their technical assistance during the clinical studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor John H. Linehan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Maarek, J.M.I., Rubinstein, E.H., Guo, Y. et al. Measurement of Cardiac Output and Blood Volume During Hemodialysis with Fluorescent Dye Dilution Technique. Ann Biomed Eng 45, 580–591 (2017). https://doi.org/10.1007/s10439-016-1711-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1711-6