Summary
Background
Time-dependent changes in glycemic control might represent a strong predictor for coronary artery disease. Since a higher benefit from outpatient appointments has been discussed for female gender, the aim of the study was to assess gender differences in HbA1c levels and metabolic parameters at baseline as well as over 3 years of follow-up.
Methods
We analyzed the data of 54 female and 65 male type 1 diabetic patients, with comparable age and diabetes duration, who visited our diabetes outpatient clinic in the year 2006 as well as the follow-up visits until 2009.
Results
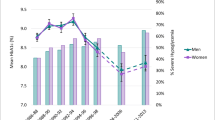
In 2006, females showed higher HbA1c levels as compared to male subjects (8.59 ± 1.60 vs. 7.75 ± 1.41, p = 0.003). Longitudinal analysis revealed that the decrease in HbA1c until 2009 was more pronounced in women (decreased to 7.52 ± 1.00) than in men (decreased to 7.50 ± 0.99, p sex:time = 0.006); however, the significance was lost after adjusting for baseline levels. Further, females showed higher levels in total-cholesterol (p = 0.001), LDL-cholesterol (p = 0.033), and HDL-cholesterol (p < 0.001) at baseline, whereas males had higher creatinine (p = 0.001) and uric acid levels (p < 0.001). No differences between the two sexes were shown for triglycerides at 2006. Additionally, uric acid levels were negatively associated with long term glycemic control, particularly in male patients.
Conclusions
Sex-related differences in metabolic parameters are present in patients with type 1 diabetes. Especially, our data suggests more adverse cardiometabolic risk markers in females. A potentially protective effect for hyperuricemia by hyperglycemia-related glucosuria is lacking in female patients with type 1 diabetes.
Zusammenfassung
Grundlagen
Zeitliche Veränderungen im glukometabolischen Profil gelten als wesentlicher prognostischer Parameter für die spätere Entwicklung kardiovaskulärer Komplikationen bei Patienten mit Typ 1 Diabetes. Ein größerer Nutzen regelmäßiger Ambulanzbesuche bei erkrankten Frauen wurde in früheren Studien diskutiert. Daher war es Ziel dieser Arbeit, geschlechtsspezifische Unterschiede von HbA1c sowie metabolischer Parameter im Verlauf von 3 Jahren zu untersuchen.
Methodik
54 Frauen und 65 Männer mit Typ 1 Diabetes (vergleichbar in Alter und Erkrankungsdauer) mit Besuchen an der Diabetesambulanz der Medizinischen Universität Wien zwischen den Jahren 2006 und 2009 wurden in diese retrospektive Untersuchung eingeschlossen.
Ergebnisse
Im Vergleich zu männlichen Patienten zeigten Frauen im Jahr 2006 höhere HbA1c Werte (8,59 ± 1,60 vs. 7,75 ± 1,41, p = 0,003). Eine Analyse des zeitlichen Trends zeigte eine deutlichere Verbesserung der Blutzuckereinstellung auf Seiten der Frauen (HbA1c Wert verringerte sich auf 7,52 ± 1,00 bei Frauen und auf 7,50 ± 0,99 bei Männern, p Geschlecht:Zeitverlauf = 0,006). Allerdings verlor sich die signifikante Interaktion nach Adjustierung für die Ausgangswerte. Weiters zeigten Frauen im Jahr 2006 höhere Werte im Gesamtcholesterin (p = 0,001), LDL-Cholesterin (p = 0,033) sowie HDL-Cholesterin (p < 0,001), wogegen höhere Serum-Kreatinin (p = 0,001) und Harnsäure Werte (p < 0,001) bei den männlichen Patienten beobachtet wurden. Keine signifikanten Unterschiede zeigten sich dagegen bei Triglyzeriden. Weiters wurde ein negativer Zusammenhang zwischen Harnsäure und HbA1c insbesondere bei männlichen Patienten beobachtet.
Schlussfolgerungen
Diese Studie zeigt geschlechtsspezifische Unterschiede in metabolischen Parametern bei Patienten mit Typ 1 Diabetes. Insbesondere zeigen Frauen ein deutlich ungünstigeres kardiometabolisches Risikoprofil. Der negative Zusammenhang zwischen Harnsäure und HbA1c zeigt sich bei Frauen weniger stark ausgeprägt.


Similar content being viewed by others
References
Kautzky-Willer A, Handisurya A. Metabolic diseases and associated complications: sex and gender matter! Eur J Clin Invest. 2009;39:631–48.
Legato MJ, Gelzer A, Goland R, et al. Writing group for the partnership for gender-specific medicine. Gender-specific care of the patient with diabetes: review and recommendations. Gend Med. 2006;3:131–58.
Auryan S, Itamar R. Gender specific care of diabetes mellitus: particular considerations in the management of diabetic women. Diabetes Obes Metab. 2008;10:1135–56.
Gale EAM, Gillespie KM. Diabetes and gender. Diabetologia. 2001;44:3–15.
Ostermann J, Lönnberg G, Arnquist HJ, Blohmé G, Bolinder J, Ekbom Schell A, Eriksson JW, Gudbjörnsdottir S, Sundkvist G, Nyström L. Gender differences and temporal variation in the incidence of type 1 diabetes: results of 8012 cases in the nationwide Diabetes Incidence Study in Sweden 1983–2002. J Intern Med. 2008;263:386–94.
Gerstl EM, Rabl W, Gröbe H, Hofer SE, Krause U, Holl RW. Metabolic control as reflected by HbA1c in children, adolescents and young adults with type 1 diabetes mellitus: combined longitudinal analysis including 27,035 patients from 207 centers in Germany and Austria during the last decade. Eur J Pediatr. 2008;167:447–53.
Schwab KO, Doerfer J, Naeke A, Rohrer T, Wiedmann D, Marg W, Hofer SE, Holl RW, on behalf of the German/Austrian Pediatric DPV Initiative. Influence of food intake, age, gender, HbA1c, and BMI levels on plasma cholesterol in 29,979 children and adolescents with type 1 diabetes—reference data from the German diabetes documentation and quality management system (DPV). Pediatric Diabetes. 2009;10:184–92.
Idzior-Walus B, Mattock MB, Solnica B, Stevens L, Fuller JH, et al. Factors associated with plasma lipids and lipoproteins in type 1 diabetes mellitus: the EURODIAB IDDM complication study. Diabetic Medicine. 2001;18:786–96.
Sparud-Lundin C, Öhrn I, Danielson E, Forsander G. Glycemic control and diabetes care utilization in young adults with type 1 diabetes. Diabetic Medicine. 2008;25:968–73.
Prince CT, Becker DJ, Costacou T, Miller RG, Orchard TJ. Changes in glycemic control and risk of coronary artery disease in type 1 diabetes mellitus: findings from the Pittsburgh Epidemiology of Diabetes Complications Study (EDC). Diabetologia. 2007;50:2280–88.
Soedamah-Muthu SS, Chaturvedi N, Toeller M, Ferriss B, Reboldi P, Michel G, Manes C, Fuller JH, et al. Risk factors for coronary heart disease in type 1 diabetic patients in Europe. The EURODIAB prospective complications study. Diabetes Care. 2004;27:530–37.
American Diabetes Association. Diagnosis and classification of Diabetes Mellitus. Diabetes Care. 2010;33(S1):62–9.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
Barnett AG, Van Der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2005;34:215–20.
Morton V, Torgerson J. Effect of the regression to the mean on decision making in the health care. BMJ. 2003;326:1083–84.
Kacerovsky-Bielesz G, Lienhardt S, Hagenhofer M, Kacerovsky M, Forster E, Roth R, Roden M. Sex-related psychological effects on metabolic control in type 2 diabetes mellitus. Diabetologia. 2009;52:781–88.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. NEJM. 1993;329:977–86.
Jenkins AJ, Lyons TJ, Zheng D, Otvos JD, Lackland DT, McGee D, Garvey WT, Klein RL, The DCCT/EDIC Research Group. Serum lipoproteins in the diabetes control and complications trial/epidemiology of diabetes intervention and complications cohort. Diabetes Care. 2003;26:810–18.
Nádas J, Putz Z, Fövényi J, Gaál Z, Gyimesi A, Hidvégi T, Hosszúfalusi N, Neuwirth G, Oroszlán T, Pánczél P, Széles G, Vandorfi G, Winkler G, Wittmann I, Jermendy G. Cardiovascular risk factor characteristic for the metabolic syndrome in adult patients with type 1 diabetes. Exp Clin Endocrinol Diabetes. 2009;117:107–12.
Thorn LM, Forsblom C, Fagerudd J, Thomas MC, Pettersson-Fernholm K, Saraheimo M, Wadén J, Rönnback M, Rosengard-Bärlund M, Björkesten CG, Taskinen MR, Groop PH, FinnDiane Study group. Metabolic syndrome in type 1 diabetes: association with diabetic nephropathy and glycemic control (the FinnDiane study). Diabetes Care. 2005;28:2019–24.
Metascreen Writing Committee. The metabolic syndrome is a risk indicator of microvascular and macrovascular complications in diabetes. Results from Metascreen, a multicenter diabetes clinic-based survey. Diabetes Care. 2006;29:2701–07.
Pambianco G, Costacou T, Orchard TJ. The prediction of major outcomes of type 1 diabetes: a 12-year prospective evaluation of three separate definitions of the metabolic syndrome and their components and estimated glucose disposal rate: the Pittsburgh epidemiology of diabetes complications study experience. Diabetes Care. 2007;30:1248–54.
Göbl CS, Brannath W, Bozkurt L, Handisurya A, Anderwald C, Luger A, Krebs M, Kautzky-Willer A, Bischof MG. Sex-specific differences in glycemic control and cardiovascular risk factors in elderly patients with insulin-treated type 2 diabetes mellitus. Gender Medicine. 2010;7:593–99.
Maric C. Risk factors for cardiovascular disease in women with diabetes. Gend Med. 2010;7:551–56.
Rodriguez G, Soriano LC, Choi HK. Impact of diabetes against the future risk of developing gout. Ann Rheum Dis. 2010;69:2090–94.
Sui X, Church TS, Meriwether RA, Lobelo F, Blair SN. Uric acid and the development of metabolic syndrome in women and men. Metabolism. 2008;57:845–52.
Freedman DS, Williamson DF, Gunter EW, Byers T. Relation of serum uric acid to mortality and ischemic heart disease. The NHANES I Epidemiologic Follow-up Study. Am J Epidemiol. 1995;141:637–44.
Choi HK, Ford ES. Hemoglobin A1c, fasting glucose, serum C-peptide and insulin resistance in relation to serum uric acid levels—the Third National Health and Nutrition Examination Survey. Rheumatology. 2008;47:713–17.
Chou P, Lin KC, Lin HY, Tsai ST. Gender differences in the relationship of serum uric acid with fasting serum insulin and plasma glucose in patients without diabetes. J Rheumatol. 2001;28:571–76.
Kautzky-Willer A, Dorner T, Jensby A, Rieder A. Women show a closer association between educational level and hypertension or diabetes mellitus than males: a secondary analysis from the Austrian HIS. BMC Public Health. 2012;12. doi:10.1186/1471-2458-12-392.
Conflict of interest
The authors declare that there is no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Göbl, C., Bozkurt, L., Lueck, J. et al. Sex-specific differences in long-term glycemic control and cardiometabolic parameters in patients with type 1 diabetes treated at a tertiary care centre. Wien Klin Wochenschr 124, 742–749 (2012). https://doi.org/10.1007/s00508-012-0246-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-012-0246-6